-
PDF
- Split View
-
Views
-
Cite
Cite
Birkaran Sadhar, David Slupek, Andrew Steehler, Carter Denne, Kirk Steehler, Primary diffuse large B-cell lymphoma of the lacrimal sac with involvement of maxillary sinus: a case report and review of literature, Journal of Surgical Case Reports, Volume 2024, Issue 7, July 2024, rjae453, https://doi.org/10.1093/jscr/rjae453
Close - Share Icon Share
Abstract
Primary lacrimal sac lymphoma is a rare condition, often presenting with nasolacrimal duct obstruction. Herein, we present a unique case of diffuse large B-cell lymphoma (DLBCL) involving the lacrimal sac, maxillary sinus, and infraorbital nerve. Prompt diagnosis via biopsy is essential for timely treatment and the prevention of tumor progression. A 66-year-old female presented with intractable epiphora, infraorbital nerve hypesthesia, and medial canthal swelling. Imaging revealed a soft tissue mass in the right maxillary sinus extending into the right inferior orbit and nasal cavity. A biopsy confirmed DLBCL, prompting systemic chemotherapy. Residual disease prompted high-dose involved-site radiation, resulting in tumor regression. To our knowledge, this is the first case of primary DLBCL of the lacrimal sac with concurrent involvement of the maxillary sinus and infraorbital nerve. This case underscores the significance of lacrimal sac biopsy in refractory dacryocystitis or unilateral sinus disease and the effectiveness of multimodal treatment approaches in managing DLBCL.
Introduction
Primary lacrimal sac lymphoma is a rare condition that typically presents as nasolacrimal duct obstruction [1]. Diffuse large B-cell lymphoma (DLBCL) ranks as the third most prevalent primary ocular adnexal lymphoma (OAL), constituting ~8% of all such lymphomas [2]. DLBCL is more frequently found in the lacrimal sac compared to other orbital structures and is a high-grade non-Hodgkin’s lymphoma with an aggressive course [2]. Systemic chemotherapy with adjuvant radiotherapy yields a good prognosis with low recurrence rates [1]. This report discusses a unique case of primary DLBCL of the lacrimal sac involving the maxillary sinus and demonstrates the need to consider lacrimal sac biopsy for intractable dacrocystitis, epiphora, or intractable unilateral sinus disease given the concern for a neoplastic process.
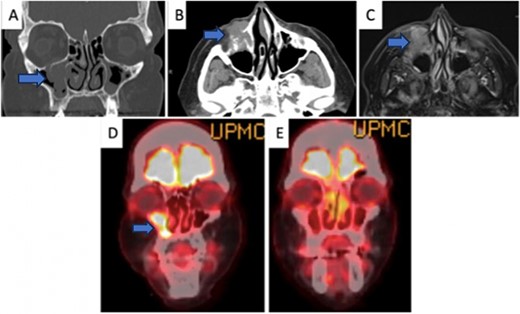
(A) Coronal CT (bone window) depicting the involvement of the tumor in the maxillary sinus extending into the lacrimal duct. (B) Axial CT (soft tissue window) of the tumor showing extent of involvement in the bone and surrounding soft tissue structures. (C) Axial MR of a similar window to Fig. 1B. (D) Initial coronal PET-CT depicting the avidity of the tumor before treatment. (E) Post-treatment PET-CT showing a significant reduction in uptake to the tumor.
Case report
A 66-year-old female presented to the emergency department with a 10-week history of worsening right-sided epiphora, recently developed infraorbital nerve hypesthesia, and medial canthal swelling refractory to dicloxacillin (for presumed dacrocystitis). Nasal endoscopy revealed right lateral nasal cavity fullness with healthy mucosa without masses or lesions. Computed tomography (CT) imaging revealed a destructive soft tissue mass in the anteromedial right maxillary sinus with osseous erosion into the right inferior orbit and nasal cavity (Fig. 1A and B). On palpation, a distinct, fluctuant mass was noted. The patient was admitted for further workup, and an incisional biopsy was performed at the bedside to assess potential neoplastic involvement. After appropriate local anesthesia, a scalpel was used to make a 1.5-cm incision just above the orbital rim toward the medial canthus ~1 cm below the eyelid. The incision was then carried down through the orbicularis oculi muscle, and the tissue appeared scalloped with a gray-tan appearance, distinct from the bony tissue surrounding it. A biting forceps was used to remove several pieces of tissue. A 4-0 chromic was placed to approximate the muscle. The skin was reapproximated using a 5-0 chromic in a running fashion. The patient tolerated the procedure well with a good cosmetic outcome on follow-up.
Pathological study (Fig. 2) of the biopsied tissue was consistent with DLBCL positive for CD20 and leukocyte common antigen. Subsequent FISH high-grade lymphoma panel was positive for IGH/BCL-2 fusion, with gains but not rearrangements of BCL6 and MYC. Pathologic workup suggested single-hit lymphoma, which generally has a better prognosis.
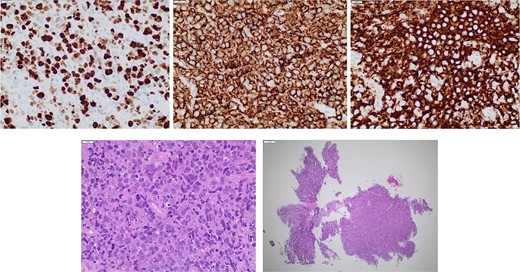
Pathology studies on the incisional biopsy, including CD20 and leukocyte common antigen. FISH high-grade lymphoma panel with IGH/BCL-2 fusion positivity, with gains but not rearrangements of BCL6 and MYC.
Contrast-enhanced magnetic resonance imaging (MRI) (Fig. 1C) exhibited involvement of the right infraorbital nerve, consistent with the initial physical exam findings. There was a single ipsilateral level 2 neck node with avid uptake, suggesting regional metastasis. Positron emission tomography-CT (PET-CT) confirmed the final diagnosis of Stage IIa DLBCL of the right lacrimal duct and orbit with maxillary sinus involvement and a secondary cervical lymph node (Fig. 1D) with no distant metastasis.
The patient opted for three cycles of R-CHOP (rituximab, cyclophosphamide, doxorubicin hydrochloride, vincristine sulfate, and prednisone) therapy. Follow-up PET-CT revealed avid uptake at the floor of the right maxillary sinus, with increased uptake compared to the initial PET-CT. This was concerning for refractory lymphoma. The patient decided not to pursue additional R-CHOP chemotherapy and instead opted for high-dose involved-site radiation to the refractory disease. PET-CT at 6 months post-radiotherapy suggested a Deauville-4 response with some residual FDG avidity at the floor of the maxillary sinus. Oncology recommended Rituxan to treat the residual disease; however, she declined. The final PET-CT at 9 months revealed a reduction in residual uptake in the floor of the right maxillary sinus (Fig. 1E), with the maximum SUV decreasing from 11.5 to 9.2. Due to personal reasons, the patient opted to proceed with continued observation and deferred additional chemotherapy. She continues to follow up at 6-month intervals without any growth of the tumor to date.
Discussion
Lymphoma of the lacrimal sac accounts for a small portion of OALs with one large study showing 2.5% (9/353) of OALs occurring in the lacrimal sac [3]. Neerukonda et al. [1] highlighted that of 566 lacrimal sac histological specimens, only three cases of primary lacrimal sac lymphoma were reported, and only one case manifested as a lacrimal sac mass. Of all reported OAL diagnoses, DLBCL has been responsible for a death rate of 38% to 48%, prompting the need for timely biopsy [4, 5]. Age (>59 years), stage IV, high-grade histological subgroup, and the presence of B symptoms, adversely affect the overall survival rate [6]. Although our patient was older, her staging (IIa), lack of a high-grade histological subgroup, and lack of B symptoms supported a good prognosis with adequate treatment.
Less than 15% of cases with malignant lacrimal sac tumors receive an accurate and immediate diagnosis [7]. Biopsy confirmation is essential for diagnoses, as seen in our case. Utilizing CT and MRI can assist in establishing a definitive diagnosis, staging, and treatment planning [7]. In addition, PET-CT was used in this case to both diagnose and monitor the effectiveness of treatment therapy.
The primary treatment of DLBCL is systemic chemotherapy with adjuvant radiotherapy [2, 4]. Using rituximab alongside chemotherapy provides a notable advantage in overall survival and response rate for DLBCL cells expressing the CD20 antigen, compared to chemotherapy alone [8]. The patient deferred surgical removal of the tumor and was referred to radiation and medical oncology, and received three cycles of R-CHOP followed by intensity-modulated radiotherapy.
Based on a review of the literature, this case was unique in that it additionally involved the maxillary sinus and the infraorbital nerve. Two recent cases of DLBCL localized to the lacrimal sac employed chemotherapy along with other treatments. Kim et al. [2] presented a case of DLBCL limited to the lacrimal sac that was successfully treated with a dacryocystectomy and six courses of CHOP following an initial post-surgical relapse. Ueathaweephol et al. [9] presented a case that was successfully treated with eight cycles of R-CHOP and intrathecal methotrexate. While neither case incorporated adjuvant radiotherapy, they support the efficacy of expeditious biopsy and multimodal treatment approaches, as our case does.
Further investigation into the characteristics, local structural involvement, treatment modalities, and outcomes of DLBCL affecting the lacrimal sac and maxillary sinus is essential.
Conflict of interest statement
All authors declare that they have no conflicts of interest.
Funding
None declared.



