-
PDF
- Split View
-
Views
-
Cite
Cite
Su Su Hlaing (Sharon), Jai Hoff, Prasad Jayaratne, Kayla Tran, Mairi Jarvis, Yiu Ming Ho, Anastomosing hemangioma of adrenal gland: rare benign vascular tumor, Journal of Surgical Case Reports, Volume 2025, Issue 7, July 2025, rjaf467, https://doi.org/10.1093/jscr/rjaf467
Close - Share Icon Share
Abstract
Anastomosing hemangioma of the adrenal gland is a rare benign vascular neoplasm that often presents incidentally during imaging for unrelated conditions. This tumor may mimic more aggressive lesions, such as angiosarcoma, due to its vascular nature; however, it is characterized by a distinctive lobular architecture and the absence of significant cytologic atypia. Typically found in older patients, anastomosing hemangiomas range in size and are usually solitary. The patient is 49-year-old gentleman who underwent laparoscopic left adrenalectomy for incidentally found 5 cm left adrenal tumor. Histologically, it was confirmed as anastomosing hemangioma with proliferating size spaced lined by epithelium with hobnail morphology. This case aims to contribute to sparse literature for future imaging findings, histology findings, and options of management: observation vs. operative.
Introduction
Anastomosing hemangioma is a rare benign vascular neoplasm that can occur in various anatomical locations, most commonly in the genitourinary tract (kidneys), retroperitoneum, soft tissues, bones, and rarely involved adrenal gland. Given its rarity, there is no standard diagnostic test when suspected, and only confirmed during histology after surgical removal. In this case report, we present a patient with an incidental adrenal anastomosing hemangioma during workup for a chest infection.
Case report
A 49-year-old male referred by his general practitioner for evaluation of an incidental left adrenal mass identified on a computed tomography (CT) scan of the chest conducted due to a suspected chest infection. He has a background of paranoid schizophrenia, mild intellectual impairment; severe obstructive sleep apnea (OSA) managed with continuous positive airway pressure (CPAP), morbid obesity (BMI 40.49), cervical spine osteophyte, hypertension, and a significant smoking history (25 cigarettes per day).
CT of the abdomen and pelvis revealed a nearly 6 cm adrenal mass characterized by necrosis, with no evidence of distant metastases. The mass showed a thin rind of lobulated peripheral hyperenhancement associated with fat stranding and fluid extending into the left perinephric space. The left adrenal gland appeared distorted.
A positron emission tomography (PET) scan showed mild fluorodeoxyglucose (FDG) uptake within the medial aspect of the left adrenal mass, raising suspicion for an adrenal cortical carcinoma. Despite the mass’s size and characteristics, the patient did not exhibit any endocrine symptoms, including signs of Cushing’s syndrome or malignant hypertension. There were false-positive marginal elevations of plasma metanephrines, prompting further investigation with supine plasma metanephrines and 24-hour urinary free cortisol assessments, which confirmed a nonfunctioning adrenal tumor (Fig. 1).
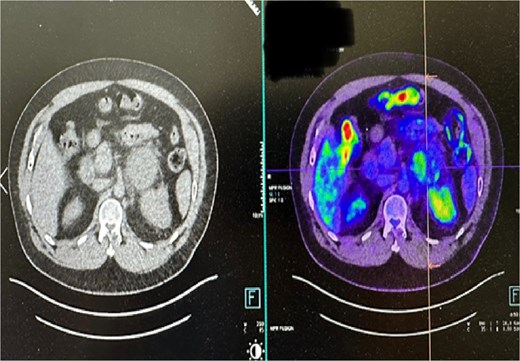
PET CT scan: minimal to mild FDG uptake in the medial aspect of enlarged left adrenal mass.
Patient underwent a laparoscopic left adrenalectomy a few months after investigations. He had an uneventful surgery with an area of tissue adhesion at the renal margin. The histology reveals a circumscribed, non-encapsulated lesion in the periadrenal fat, characterized by irregular, anastomosing capillary-sized spaces lined by a single layer of endothelial cells with hobnail morphology. There is no nuclear atypia or mitotic activity. The surrounding stroma is edematous, with areas of fibrous and hemorrhagic cystic degeneration. Immunohistochemical staining for CD31 and CD34 confirms the endothelial nature of the lesion, leading to a diagnosis of anastomosing hemangioma. Clear margins were achieved during resection. The patient was discharged the following day after overnight monitoring. A follow-up appointment in the outpatient department three weeks post-surgery confirmed the patient was recovering well.
Discussion
To date, there have only been 16 reported cases of adrenal anastomosing hemangioma in the literature, according to our knowledge, with an estimated incidence of 3%–4% [1]; therefore, highlighting the limited clinicopathological and radiological findings to diagnose this condition. Adrenal hemangiomas are usually asymptomatic and found mostly incidentally during imaging for unrelated presentations. The mean age of anastomosing hemangiomas is 49 years, with a range of 32–68 years old, and no gender predilection [1]. However, it is found that 68% (11) of 16 reported cases were men, and 33% [5] were women. The mean tumor size in one of the case series is 2 cm, with the largest reported by Nishikimi et al. as 7.2 × 6.4 × 5.6 cm in size, which was removed by robot-assisted adrenalectomy [2].
Due to its rare occurrence, there were no radiologic features to definitively diagnose anastomosing hemangioma, which can mimic renal cell carcinoma, neuroendocrine tumor, and pheochromocytoma. The usual contrast-enhanced CT findings are nonspecific, with homogenous or heterogenous enhancement in the periphery, similar to our case. On magnetic resonance imaging (MRI), they can present as iso or high intensity during T2-weighted and diffusion-weighted imaging (DWI) [3]. It has been reported that MRI can differentiate hemangiomas and malignant tumors with 97% accuracy, 100% sensitivity, and 92% specificity in hepatic lesions, as per McFarland et al. [4].
It is commonly diagnosed postoperatively by histologic examination, which requires differentiation from aggressive angiosarcoma. Grossly, they are well-circumscribed hemorrhagic lesions and histologically show prominent hobnailing of endothelial cells with anastomosing sinusoidal spaces without evidence of atypia or invasive malignancy. Recent retrospective study of 13 anastomosing hemangiomas showed GNAQ gene mutation as a driver for pathogenesis of anastomosing hemangioma, which is not found in angiosarcoma [5]. This could potentially be useful in preoperative biopsy to distinguish from angiosarcoma (Fig. 2).
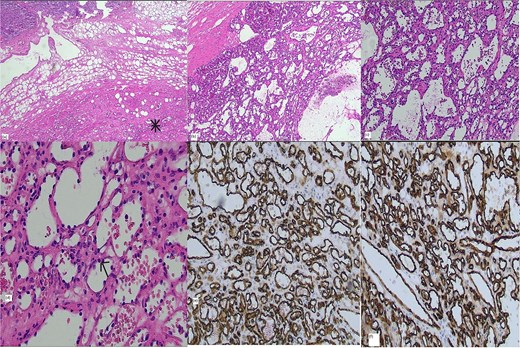
Histology: (a) Hematoxylin and eosin (H&E) stain × 2 magnification showing interface of adrenal (top) and vascular lesion (bottom), (b) H&E stain × 4 magnification (c) H&E stain × 10 magnification, (d) H&E stain × 20 magnification, positive vascular endothelial immunohistochemical markers CD 31 (e) and CD 34 (f).
Current management of adrenal tumor is guided by adrenal incidentaloma, which recommends surgical resection for lesions >4 cm in size for definitive tissue diagnosis due to high risk or malignancy [6]. Anastomosing hemangioma is a benign tumor, which is cured after complete surgical resection without risk of recurrence in the literature [1]. For this reason, some patients may be suitable for observation without unnecessary surgical intervention.
Conclusion
In conclusion, this is a case of rare incidental anastomosing adrenal hemangioma, which can pose diagnostic challenges due to its scarcity in the literature regarding its clinical, pathological, and radiological findings. The currently accepted treatment is surgical resection; however, a further understanding of this condition could lead to more accurate diagnoses, potentially avoiding unnecessary operations due to its benign nature.
Author contributions
SH: manuscript preparation, conceptualization, editing. JH: editing and final approval. YMH: editing and final approval. KT, PJ, MJ: histopathology slides and pathological review.
Conflict of interest statement
No conflicts of interest to declare.
Funding
No funding required.
Patient consent
Consent obtained directly from the patient.



