-
PDF
- Split View
-
Views
-
Cite
Cite
William Qian, Jewel Soares, Ishanth Devinda Jayewardene, Nigel Peck, Bouveret syndrome preceding classical gallstone ileus: a rare presentation of a cholecystoduodenal fistula, Journal of Surgical Case Reports, Volume 2024, Issue 7, July 2024, rjae421, https://doi.org/10.1093/jscr/rjae421
Close - Share Icon Share
Abstract
Bouveret syndrome is the rarest variant of gallstone ileus characterized by the passage and impaction of a gallstone through a bilioenteric fistula leading to gastric outlet obstruction. The documented movement of an impacted gallstone in Bouveret syndrome through the gastrointestinal tract has not been previously discussed in the literature. A 64-year-old man presented with acute on chronic epigastric pain, fevers, and vomiting. Abdominal computed tomography established a diagnosis of Bouveret syndrome. A trial of endoscopic gallstone extraction was unsuccessful. Laparoscopic gastrotomy and stone removal were later attempted, however, intraoperatively it was noted that the stone had migrated and was now impacted in the jejunum causing a small bowel obstruction. The clinical picture was now that of gallstone ileus. Laparoscopic enterolithotomy was performed successfully. This article discusses the radiological, endoscopic, and intraoperative findings in this rare case of Bouveret syndrome that had evolved into classical gallstone ileus following stone migration.
Introduction
Bouveret syndrome is the rarest variant of gallstone ileus characterized by the passage and impaction of a gallstone through a bilioenteric fistula leading to gastric outlet obstruction [1]. It carries a high mortality rate estimated from 12% to 30% [2], underscoring the lack of agreed workup and management owing to its complexity and rarity. We herein discuss a rare case of Bouveret syndrome diagnosed on computed tomography (CT) which failed endoscopic treatment. Subsequently the gallstone had migrated and impacted in the jejunum causing a small bowel obstruction. This atypical association between Bouveret syndrome and classical gallstone ileus has not been discussed previously in the literature. The patient was treated successfully with laparoscopic enterolithotomy.
Case report
A 64-year-old male presented with a 1-month history of epigastric pain that had acutely worsened in the 3 days prior with fevers, anorexia, and multiple vomits. This was on a background of type 2 diabetes mellitus and hypertension. An abdominal CT, 4 years prior incidentally demonstrated multiple dependent calculi in the gallbladder, the largest measuring 23 × 23 mm. On examination, he was haemodynamically stable and afebrile. His abdomen was soft although tender in the right upper quadrant. Murphy’s sign was positive. Routine biochemistry revealed mildly elevated inflammatory markers and alkaline phosphatase (Table 1). CT of the abdomen and pelvis revealed the known gallstone, now 28 mm in diameter, had dislodged and impacted between the first and second parts of the duodenum through a cholecystoduodenal fistula. There was associated gastric distension, pericholecystic inflammatory stranding, and pneumobilia (Fig. 1). These findings satisfy Rigler’s triad of an ectopic gallstone, gastric outlet obstruction, and pneumobilia. Accordingly, a diagnosis of Bouveret syndrome was made.
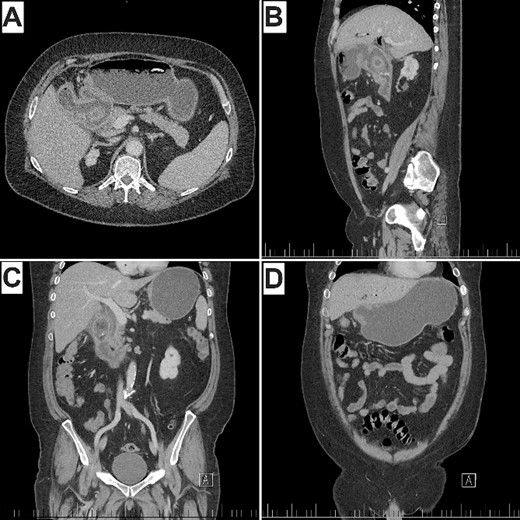
CT of the abdomen and pelvis (A) axial, demonstrating pneumobilia, cholecystoduodenal fistula, and impacted gallstone. (B) Sagittal, (C) coronal, demonstrating obstructing gallstone in the proximal duodenum with distal duodenal collapse and pericholecystic inflammatory stranding. (D) Gastric distension proximal to the impacted stone. Note Rigler’s triad of pneumobilia (A), ectopic gallstone (A, B, C), and gastric outlet obstruction (B, D).
| Pathology . | Day of presentation . | Normal range . |
|---|---|---|
| Bilirubin | 10 uμmol/L | < 20 μmol/L |
| Alkaline phosphatase | 126 unit/L | 30–110 unit/L |
| Gamma-glutamyltransferase | 49 unit/L | 5–50 unit/L |
| Alanine aminotransferase | 11 unit/L | 1–40 unit/L |
| Aspartate aminotransferase | 23 unit/L | 10–35 unit/L |
| C-reactive protein | 9 mg/L | < 5 mg/L |
| White blood cell count | 13.2 × 109/L | 4.0–11.0 × 109/L |
| Pathology . | Day of presentation . | Normal range . |
|---|---|---|
| Bilirubin | 10 uμmol/L | < 20 μmol/L |
| Alkaline phosphatase | 126 unit/L | 30–110 unit/L |
| Gamma-glutamyltransferase | 49 unit/L | 5–50 unit/L |
| Alanine aminotransferase | 11 unit/L | 1–40 unit/L |
| Aspartate aminotransferase | 23 unit/L | 10–35 unit/L |
| C-reactive protein | 9 mg/L | < 5 mg/L |
| White blood cell count | 13.2 × 109/L | 4.0–11.0 × 109/L |
| Pathology . | Day of presentation . | Normal range . |
|---|---|---|
| Bilirubin | 10 uμmol/L | < 20 μmol/L |
| Alkaline phosphatase | 126 unit/L | 30–110 unit/L |
| Gamma-glutamyltransferase | 49 unit/L | 5–50 unit/L |
| Alanine aminotransferase | 11 unit/L | 1–40 unit/L |
| Aspartate aminotransferase | 23 unit/L | 10–35 unit/L |
| C-reactive protein | 9 mg/L | < 5 mg/L |
| White blood cell count | 13.2 × 109/L | 4.0–11.0 × 109/L |
| Pathology . | Day of presentation . | Normal range . |
|---|---|---|
| Bilirubin | 10 uμmol/L | < 20 μmol/L |
| Alkaline phosphatase | 126 unit/L | 30–110 unit/L |
| Gamma-glutamyltransferase | 49 unit/L | 5–50 unit/L |
| Alanine aminotransferase | 11 unit/L | 1–40 unit/L |
| Aspartate aminotransferase | 23 unit/L | 10–35 unit/L |
| C-reactive protein | 9 mg/L | < 5 mg/L |
| White blood cell count | 13.2 × 109/L | 4.0–11.0 × 109/L |
A nasogastric tube successfully decompressed the stomach before the patient was taken for gastroscopy. There, the impacted gallstone was visualized between the first and second parts of the duodenum (Fig. 2). Multiple attempts to extract the gallstone with various instruments were unsuccessful and the procedure was abandoned. Laparoscopic gastrotomy and stone retrieval was planned for 3 days’ time. The patient was kept fasted with total parenteral nutrition and intravenous piperacillin–tazobactam in between the cases. During the operation there was difficulty mobilizing omentum that was adherent to the fistula. An intraoperative gastroscopy was able to enter the cholecystoduodenal fistula as well as the third part of the duodenum, failing to reveal the impacted gallstone. A cholecystotomy displayed a gallbladder clear of stones. The small bowel was inspected and the gallstone was encountered ~30 cm distal to the duodenojejunal flexure. Here, it was again obstructing with proximal small bowel distension. Laparoscopic enterolithotomy was successful in retrieving the stone (Fig. 3). The cholecystotomy was sutured close. The patient was discharged eight days later following an unremarkable post-operative recovery. At 4- and 6-week follow-up, the patient was well and remained pain free with no new issues.
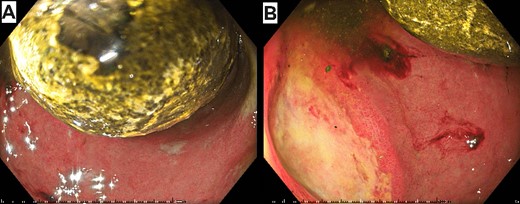
Initial gastroscopy showing impacted gallstone between the first and second parts of the duodenum (A) and the cholecystoduodenal fistula (B).

Successful laparoscopic enterolithotomy via longitudinal incision in the jejunum.
Discussion
We report on a rare case of gastric outlet obstruction secondary to an impacted gallstone in the proximal duodenum following its passage through a bilioenteric fistula. First described by the surgeon M. Beassier in 1770, this syndrome was later named after the physician L. Bouveret following his comprehensive reporting of two such cases in 1896 [3]. In this case the bilioenteric fistula presented as a cholecystoduodenal fistula, the most common form, seen in 68% of cases [4]. Cholecystogastric or cholecystocolic fistulas are less common comprising of 5% and 17% of cases, respectively [5]. Such fistulas form following an attack of calculous cholecystitis where the local inflammation contributes to pressure necrosis of the closely adherent gallbladder wall and adjacent viscous, facilitating the creation of a tract between the two lumens [4]. In this case, there was likely an element of calculous cholecystitis correlating with the patient’s one month history of epigastric pain.
Gallstone ileus is uncommon, accounting for <1% of all mechanical bowel obstruction cases [6]. Bouveret syndrome constitutes between 1% and 3% of gallstone ileus cases [2]. In the 50 years between 1967 and 2016, there have only been 315 cases reported in the literature [7]. Worth noting is the low success rate of endoscopic gallstone extraction (43.0%) compared with surgery (94.1%) in Bouveret syndrome [8]. Unique to this case is the evolution of CT-confirmed Bouveret syndrome into classical gallstone ileus, a development not previously discussed in the literature. This raises the question of whether the impacted stone was mechanically aided distally following the unsuccessful endoscopic retrieval attempt, or if the stone had spontaneously migrated in the 3 days between the initial gastroscopy and surgery. In the wake of stone migration in this case, the management was altered intraoperatively where the planned gastrotomy was changed to enterolithotomy.
There is no consensus on the best approach to cholecystectomy and fistula repair when treating Bouveret syndrome. However, the literature has demonstrated that cholecystectomy and fistula repair at the time of enterolithotomy is associated with increased mortality (20%–30%) when compared to stone extraction alone (12%) [5]. Furthermore, only 10% of patients will require additional surgery for persistent biliary symptoms when the gallbladder and fistula are left in situ [9]. Accordingly, a cholecystectomy or fistula repair was not performed in this case, where the primary goal was to relieve the patient’s obstruction.
Of note in this case is the prompt diagnosis of Bouveret syndrome just hours following presentation, owing to CT imaging. The scan promptly demonstrated Rigler’s triad; pneumobilia, ectopic gallstone, and gastric outlet obstruction (Fig. 1), pathognomonic for Bouveret syndrome [4]. A limitation of CT, however, is its inability to detect iso-attenuating stones, the scenario in ~15% to 25% of cases [4]. In these situations, magnetic resonance cholangiopancreatography may be considered.
Conclusion
A rare case which demonstrates that impacted gallstones in Bouveret syndrome may migrate distally, either mechanically following gastroscopy or spontaneously, a factor to consider in the surgical planning of Bouveret syndrome. This case report lends credence to the effectiveness of CT in promptly diagnosing Bouveret syndrome when there is not an iso-attenuating stone, as well as the viability of laparoscopic enterolithotomy in treating gallstone ileus.
Conflict of interest statement
None declared.
Funding
None declared.



