-
PDF
- Split View
-
Views
-
Cite
Cite
Masashi Nagata, Jun Miyagi, Yoshihiko Kanai, Shinichi Yamamoto, Hiroyoshi Tsubochi, Shunsuke Endo, Air leakage directly into dissected upper mediastinum following right upper lobectomy, Journal of Surgical Case Reports, Volume 2025, Issue 7, July 2025, rjaf461, https://doi.org/10.1093/jscr/rjaf461
Close - Share Icon Share
Abstract
Postoperative subcutaneous emphysema (SE) can sometimes lead to clinical complications, mainly due to abnormal air leakage (AL) into the chest wall through the surgically breached parietal pleura. In this report, we describe a patient who, following a right upper lobectomy and upper mediastinal dissection, developed progressive mediastinal and SE on postoperative day 6, which persisted despite thoracostomy. Reoperation indicated AL from the resected interlobular plane directly into the upper mediastinum through dense adhesions. These adhesions were released, and the leakage site was re-sealed. Subsequently, the emphysema regressed. This report presents a unique route of airflow that may occur especially following right upper lobectomy, highlighting the importance of surgical treatment and AL prevention strategies in such cases.
Introduction
Extensive subcutaneous emphysema (SE) following lung resection can lead to significant clinical complications, including facial swelling, inability to open the eyes, hoarseness, and distress, potentially delaying hospital discharge. Such cases have been reported in 6.3% and 2.05% of patients following thoracotomy [1] and video-assisted thoracic surgery (VATS) [2], respectively. The primary aetiology involves air leakage (AL) through a tear in the visceral pleura and into the subcutaneous tissue of the chest wall through surgically disrupted parietal pleura [1, 2].
Herein, we present an unusual case of right upper lobectomy complicated by progressive SE due to suspected late-onset AL directly into the dissected upper mediastinum.
Case report
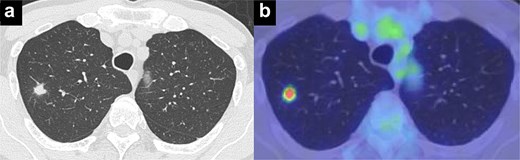
A man in his 70s presented for evaluation of a lung nodule on follow-up computed tomography (CT) 1 year postsurgery for early gastric adenocarcinoma. He had a history of heavy smoking (1.5 packs per day for 50 years) and had quit 1 year prior. CT revealed a 1.5 cm irregularly marginated solid nodule in the apical segment of the right upper lobe (Fig. 1a). Positron emission tomography (PET) revealed a maximum standard uptake value of 4.6 on the nodule (Fig. 1b). PET and brain magnetic resonance imaging revealed no metastases. All tested serum tumour marker values were within normal ranges. CT revealed emphysema of the lung. Pulmonary function tests indicated a forced expiratory volume in 1 s (FEV1.0) of 2130 ml and an FEV1.0/forced vital capacity ratio (FEV1.0%) of 65.3%. Bronchoscopic biopsy was not performed owing to difficulty in obtaining an informative specimen, and the lesion was suspected to be primary lung cancer. Although the size and location of the nodule met the criteria for intentional limited resection to treat lung cancer [3], lobectomy was considered more appropriate than apical segmentectomy for a sufficient margin and tolerable pulmonary function.
Thoracoscopic right upper lobectomy and upper mediastinal dissection were performed after obtaining informed consent. We detected the AL near the staples on the resected interlobular plane of the middle lobe and sealed it with a polyglycolic acid (PGA) sheet and fibrin glue (Video 1). Pathological examination revealed squamous cell carcinoma without lymph node metastasis. The peri- and postoperative courses were uneventful, with no evidence of AL. The chest drain was removed on postoperative day (POD) 3.
On POD 6, SE developed and spread to the chest, neck, and face. CT demonstrated remarkable mediastinal and SE with minimal lung collapse (Fig. 2; Video 2). Therefore, a chest tube was inserted, but minimal AL occurred from the chest tube, and the emphysema worsened. On POD 11, we performed thoracoscopic exploration and therapeutic intervention. Dense adhesion was confirmed between the staples on the interlobular plane and the dissected upper mediastinum. These were released, revealing the previous pleural tear. No other causative factors were observed. CT and operative findings suggested late-onset AL into the dissected mediastinum through dense adhesions. A leak test under positive pressure of up to 20 cmH2O revealed no AL from the pleural tear. The tear was sealed using a PGA sheet and fibrin glue, and 130 ml of autologous blood was injected into the pleural space to seal the dissected mediastinum and prevent air inflow (Video 3).
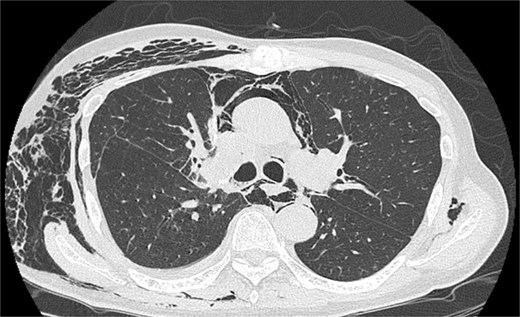
Image of postoperative mediastinal and SE with little lung collapse.
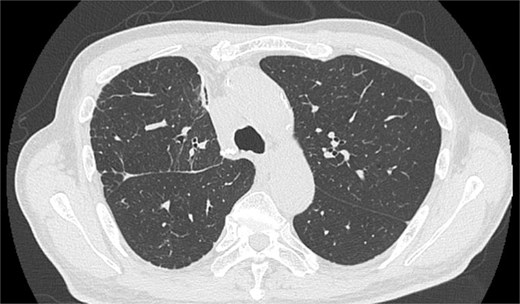
After the reoperation, AL was not observed, and SE regressed. The chest tube was removed on POD 5 after the reoperation (POD 16 after initial surgery). The patient was discharged on POD 18 after initial surgery. CT performed after 1 year revealed no emphysema or cancer recurrence (Fig. 3). The patient was informed of the complications and accepted the treatment outcomes.
Discussion
Our report suggests a unique route of air flow forming extensive SE. Although AL usually flows into both the pleural cavity and dissected mediastinum, minimal AL into the pleural cavity was seen in this case. Although AL was not detected during reoperation, it may develop under increased negative intrapleural pressure, which can be monitored using the digital chest drainage system [4]. Liu et al. described a mechanism similar to spontaneous pneumomediastinum as a potential cause of postoperative SE, where alveolar rupture leads to airflow along the bronchovascular sheath to the hilum, known as the Macklin effect [2]. However, few reports have proved progressive SE due to the Macklin effect after lobectomy. Tanaka et al. reported a large pulmonary cyst formed following the right lower lobectomy with mediastinal and SE [5], possibly caused by intrapulmonary airflow.
Right upper lobectomy with upper mediastinal dissection, pulmonary emphysema, and the use of PGA sheets may have contributed to the complication observed in our patient. After the right upper lobectomy, the middle lobe overinflates to fill the dead space, causing the resected interlobular plane to contact the upper mediastinum. The emphysematous lung is a risk factor for postoperative delayed AL and tends to overinflate, causing dense adhesion to the mediastinum. The PGA sheet can adhere strongly to adjacent tissues [6].
Here, the patient required releases of the adhesions between the lung and mediastinum. The primary treatment for postoperative extensive SE typically involves chest tube insertion into the pleural cavity to evacuate AL properly. If ineffective, VATS may be performed to seal ALs, release adhesions between the lung and chest wall, and reposition the chest tube. Additionally, various subcutaneous drainage techniques can be considered [1, 2]. However, in our case, these treatments might have been insufficient.
For patients undergoing right upper lobectomy and upper mediastinal dissection, additional prevention of AL is crucial. One such measure could be the attachment of pericardial fat [7]. A certain volume of pericardial fat between the resected interlobular plane and dissected upper mediastinum can adhere to and compress the over-expanded lung. Measures to stop airflow to the mediastinum, such as the blood patch used in our case, may be unnecessary. It is evident that segmentectomy and omitting mediastinal dissection could prevent such events.
Conclusion
We report a rare case of uncontrolled postoperative SE needing surgical intervention, ensuring the release of the adhesion between the lungs and mediastinum. This complication may occur exclusively after right upper lobectomy and upper mediastinal dissection, highlighting the importance of AL prevention.
Conflict of interest statement
None declared.
Funding
None declared.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.



