-
PDF
- Split View
-
Views
-
Cite
Cite
A Ümit Güllü, Sahin Senay, Basak Ozkan, Muharrem Kocyigit, Cem Alhan, Aortic valve reconstruction with autologous pericardium in a patient with osteogenesis imperfecta, Journal of Surgical Case Reports, Volume 2018, Issue 10, October 2018, rjy251, https://doi.org/10.1093/jscr/rjy251
Close - Share Icon Share
Abstract
Cardiac valve surgery for patients with osteogenesis imperfecta is associated with a high incidence of complications such as perioperative bleeding and valve detachment. In this report, we present a patient who was diagnosed with osteogenesis imperfecta and severe aortic insufficiency and also discussed treatment options.
INTRODUCTION
Thromboembolism, bleeding and prosthetic valve endocarditis are still the major complications following prosthetic heart valve replacement. Additionally, valve dehiscence due to extreme friability of the annulus is another complication of valve replacement in patients with connective tissue disorders such as osteogenesis imperfecta (OI) [1]. Reconstruction of all three leaflets of aortic valve using autologous pericardium recently defined by Ozaki et al. [2], may prevent these complications earlier described above. Therefore, this report presents a patient diagnosed with OI and aortic insufficiency with discussions of treatment options.
CASE REPORT
A 37-year-old male with diagnosis of OI was referred with exertional dyspnea. Echocardiographic examination showed severe degenerative aortic valve insufficiency, enlarged left ventricle (end diastolic diameter=64 mm) and decreased left ventricular ejection fraction (55%). Medical history revealed recurrent epistaxis and spontaneous bone fractures. An aortic valve intervention was planned based on the symptoms and echocardiographic results. Ozaki procedure was preferred choice of treatment related to bleeding tendency and the risk for prosthetic valve dehiscence. The technical details were described previously by Ozaki et al. [2]. Briefly, this technique can be described as the placement of the patient’s own pericardium into the aortic annulus following trimming and preparation according to the leaflet size (Fig. 1). Following the termination of cardiopulmonary bypass, transesophageal echocardiography showed no aortic valve regurgitation and gradient (2 mmHg) across the valve (Fig. 2). Postoperative follow-up was uneventful and the patient was discharged from the hospital on the fifth postoperative day. As an antiaggregant therapy just acetylsalicylic acid (300 mg) was prescribed. The transthoracic echocardiography showed no regurgitation or other pathological signs at one year follow-up.
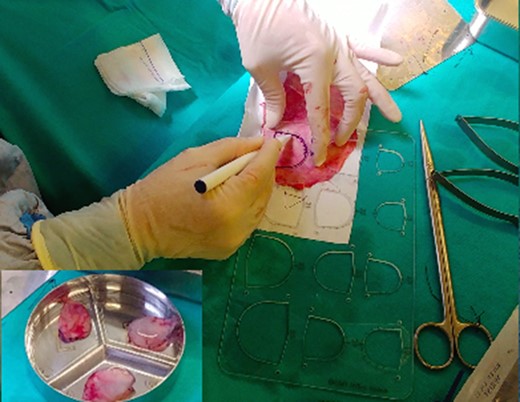
Trimming the pericardium according to each cusb size. The stitch points are marked on the pericardium.
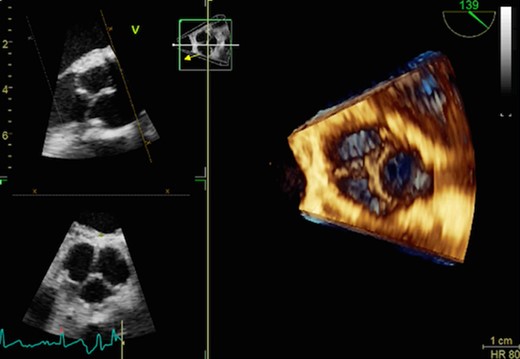
Postoperative 3D echocardiographic view shows perfect competent neovalves.
DISCUSSION
Although aortic valve replacement is the gold standard surgical technique for severe aortic valve disease, the choice of prosthesis type should always be individualized. The concerns surrounding durability of bioprosthesic compared with mechanical valves and the need for lifelong anticoagulation required with mechanical valves must be weighed [3].
For our patient who had a tendency for bleeding and spontaneous bone fractures related to OI, biological solution was the first choice. Over the last decades the use of bioprosthetic valves has significantly increased across all age groups, even there is no evidence currently to support lowering the age threshold for implanting prosthesis. On the other hand, the life expectancy of patients is improving continuously which exposes the patients with prosthesis to a higher risk of reinterventions [3].
OI, is clinically characterized by fragile bones, a post-natal growth deficiency, blue sclerae, overly extensible joints and cardiovascular abnormalities caused by weak, friable, tissues that are secondary to an underlying connective tissue disorder [1]. Cardiac surgery for patients with OI is associated with a high incidence of complications such as perioperative bleeding and prosthetic valve detachment. The scientific evidence for the defining the best choice of prosthesis in patients with OI undergoing valve replacement is still debatable. The existing data are based mainly on case reports in small numbers. Bioprosthetic valves have been recommended against mechanical valves in recent review articles [4]. The main reason for this recommendation was valve dehiscence, paravalvular leak and bleeding complications. Since there is no prosthetic annular suture line in Ozaki technique, this issue may be advantageous over prosthetic solutions to prevent detachment. Additionally, this technique provides general advantages of biological prosthesis over mechanical alternatives in means of postoperative bleeding. Aortic valve reconstruction using autologous pericardium may be another biological solution in patients who should avoid anticoagulation treatment and also at risk for prosthetic valve dehiscence.
Ozaki et al. [2] reported early and midterm results of aortic valve reconstruction using autologous pericardium along with excellent hemodynamics. In their group of 404 patients, there were no conversion to prosthetic valve replacement and no thromboembolic event and also freedom from re-operation was 96.2% at 53 months of follow-up. Halees et al. reported their aortic valve reconstruction technique with autolog and bovine pericardium and they did not found any difference in terms of valve degeneration in 16 years of follow up. The autolog pericardium was easily available, cheap and less calcified compared to bovine pericardium [5].
Another advantage of this technique is the satisfactory hemodynamic results related to absence of prosthetic suture ring. Because autologous pericardium is sutured to the native aortic annulus, the effective orifice area is expected to include a fully opened valve with the given native annulus. This advantage might be another option in patients with small aortic root.
In conclusion, Ozaki procedure is an alternative treatment option for patients who need AVR to avoid anticoagulation. This technique may provide a good quality of life without anticoagulation.
CONFLICT OF INTEREST STATEMENT
None declared.



