-
PDF
- Split View
-
Views
-
Cite
Cite
Bojana Misheva, Roy Hajjar, Hugo Chapdelaine, Herawaty Sebajang, Frank Schwenter, Ectopic jejunal pancreas with pancreatitis mistaken for a post-transplant lymphoproliferative disease in an immunosuppressed kidney transplant patient, Journal of Surgical Case Reports, Volume 2018, Issue 10, October 2018, rjy259, https://doi.org/10.1093/jscr/rjy259
Close - Share Icon Share
Abstract
An ectopic pancreas, also known as pancreatic rest or heterotopic pancreas, consists of pancreatic tissue found in a location with no continuity with the anatomic pancreas. This lesion can occasionally cause gastrointestinal obstruction, ulceration or become inflamed and cause ectopic pancreatitis. We present the case of a 29-year-old immunocompromised female patient due to a previous kidney transplant. She presented with nausea and vague abdominal discomfort and was admitted for investigation and treatment of an acute kidney injury. A small bowel mass of unknown etiology was incidentally found on abdominal computed tomography imaging. Due to the high suspicion of a post-transplant lymphoproliferative disease, a surgical exploration took place and revealed the presence of a pancreatic rest with chronic pancreatitis. Ectopic pancreas diagnosis is challenging and surgical exploration is warranted when a neoplastic process is suspected.
INTRODUCTION
Ectopic pancreas, also known as pancreatic rest, refers to pancreatic tissue found in a location without anatomic or vascular continuity with the anatomic pancreas. An ectopic pancreas is usually incidentally found in 1–15% of autopsies. When encountered in the gastrointestinal tract, it usually consists of submucosal dilated exocrine cells, but endocrine or mixed types of cells have also been described [1]. When symptomatic, these lesions can present with pancreatitis, gastrointestinal obstruction, ulceration, bleeding or even malignancy [1].
A jejunal ectopic pancreas is a very rare event, and its manifestation as a pancreatitis is even scarcer.
CASE PRESENTATION
A 29-year-old female patient presented to the emergency room with nausea and vomiting. Her past medical history included chronic kidney failure due to bilateral ureterovesical reflux for which she had a cadaveric kidney transplant at the age of 17 with chronic immunosuppressive medication. She presented with acute renal failure 9 years after the transplant, due to postinfectious glomerulonephritis, from which renal function did not fully recover.
The patient’s symptoms were accompanied by vague abdominal discomfort. Although no urinary symptoms were reported, a potential graft infection was suspected due to an abnormal urinalysis. The patient was discharged with a 7-day regimen of ciprofloxacin. The patient was rapidly readmitted due to cytopenias, arterial hypertension and acute kidney failure.
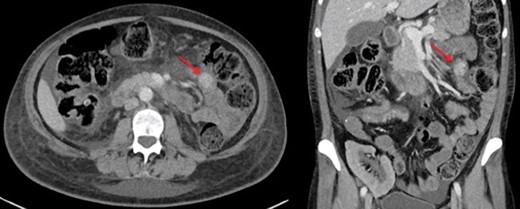
A renal biopsy was performed and showed atypical glomerulopathy with immune complexes. An autoimmune panel was negative. Investigations were performed to assess the presence of an inflammatory or infectious process. An abdominopelvic computed tomography (CT) scan revealed a hyperdense mass in the small bowel (Fig. 1). CT enterography further showed a 2 cm homogeneous jejunal lesion with no extraluminal extension (Fig. 2). Positron emission tomography scan displayed no hypermetabolism in the small bowel or in the renal allograft. Differential diagnosis included gastrointestinal stromal tumor and leiomyoma, but due to the transplant immunosuppression and the Epstein-Barr viral load of 16 596 copy/mL, a post-transplant lymphoproliferative disease (PTLD) was highly suspected.

Surgical exploration was required to determine if immunosuppressive treatments could be safely resumed. Exploratory laparotomy revealed a jejunal inflammatory lesion 10 cm distal to the Treitz ligament. Small bowel resection and anastomosis were performed. Histopathological examination revealed the presence of ectopic pancreatic tissue with chronic pancreatitis, located between the bowel mucosa and serosa. No atypia was present.
Although the lipase level was normal preoperatively, an asymptomatic acute lipase elevation was noted postoperatively, which warranted an abdominal ultrasound that showed no biliary or pancreatic abnormalities. The lipase normalized gradually a month later. Elevated lipase levels were attributed to the immunosuppressive medication the patient received.
Extensive dysmorphology work-up to identify other anatomical abnormalities, including comparative genomic hybridization, was negative. Clinical presentation and presence of thrombotic microangiopathy on renal biopsy led to the diagnosis of hemolytic uremic syndrome. Surgical and hematological evolution was favorable, but her renal function remains deteriorated and still requires hemodialysis.
DISCUSSION
We hereby present the case of a jejunal pancreatic rest with chronic pancreatitis mimicking a PTLD in an immunosuppressed patient.
The patient’s lesion was big enough to be detected on CT imaging, whereas usual ectopic pancreatic rests usually present as smaller hardly noticeable nodules located in the distal stomach, duodenum, proximal jejunum, or even the gallbladder and bile ducts [2]. They are typically discovered incidentally during endoscopy, surgery or autopsy. CT findings that may help differentiate ectopic pancreatic tissue from other submucosal lesions include a flat-ovoid shape, a location in the antrum, pylorus or duodenum, an endoluminal growth pattern with an ill-defined border and a prominent enhancement of the overlying mucosa [3]. Kim et al. [3] found that the presence of at least two of the above findings had a sensitivity of 100% and a specificity of 82.5% for diagnosing a pancreatic rest in the upper gastrointestinal tract. Nonetheless, radiological diagnosis remains a challenge as shown in this case. None of the above CT signs were specifically described to suggest a pancreatic rest rather that a neoplastic process.
Although most patients with pancreatic rests are asymptomatic, some may develop abdominal pain, pancreatitis or gastrointestinal obstruction [1, 4, 5]. Some cases of malignant transformation have also been reported, with an incidence of up to 12.7% [6–8]. It is worth noting in the present case that no potential associations have been described in recent literature between ectopic pancreas and autoimmune pathologies, renal failure or ureterovesical reflux.
On endoscopic examination, a pancreatic rest appears as a submucosal nodule, usually with a central umbilication that corresponds to a draining duct. On endosonographic examination, it appears as a hypoechoic heterogeneous lesion with indistinct margins that arises from the third or fourth layer of the gastrointestinal tract. Anechoic areas within the lesion correlate with ductal structures [1].
The diagnosis can be confirmed with biopsies or surgical specimens. Therapeutic strategies should be guided by symptoms and suspicion of malignancy. In the asymptomatic patient, periodic customized monitoring is an option. Medical treatment is not effective for symptomatic patients, and localized surgical excision has been shown to be reasonable unless malignant transformation has occurred [9]. Surgical resection is preferred to endoscopic resection when the muscularis propria is involved. Intraoperative frozen section is useful to exclude malignancy, determine the extent of resection and avoid thus unnecessary radical surgery [10].
In conclusion, ectopic pancreas is a rare pathology that is challenging to recognize. Its incidental occurrence in immunosuppressed patients where a neoplastic process might be suspected poses additional challenges to diagnosis and management.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- pancreatitis
- renal transplantation
- abdominal pain
- pancreatitis, chronic
- ulcer
- renal failure, acute
- immunocompromised host
- intestine, small
- lymphoproliferative disorders
- nausea
- neoplastic processes
- diagnosis
- diagnostic imaging
- jejunum
- pancreas
- transplantation
- gastrointestinal obstruction
- abdominal ct
- ectopic pancreas
- causality
- exploratory surgery
- pancreatic rest



