-
PDF
- Split View
-
Views
-
Cite
Cite
Juan Iaconis Campbell, Federico Coppola, Emilio Volpe, Eduardo Salas Lopez, Thoracic spinal cord injury without radiologic abnormality in a pediatric patient case report, Journal of Surgical Case Reports, Volume 2018, Issue 10, October 2018, rjy250, https://doi.org/10.1093/jscr/rjy250
Close - Share Icon Share
Abstract
Spinal Cord Injury Without Radiologic Abnormality (SCIWORA) accounts for up to 19% of spinal cord related lesions in pediatric population, mostly comprising the cervical spine. A 2-year-old patient is presented, who suffered a motor-vehicle accident. After being admitted, neither X-Ray nor spinal TC scan showed any structural abnormalities. Neurological examination showed complete sensory and motor loss under T7 as well as bladder and bowel dysfunction. Magnetic resonance imaging (MRI) showed spinal cord lesion extending from T7 to T10. The patient was treated with external immobilization and physical therapy. Thoracic SCIWORA is an uncommon diagnosis that should be considered in pediatric patients who suffer spinal trauma. Spinal cord MRI has proven to be the most accurate modality for diagnosis.
INTRODUCTION
Spinal cord injury without radiologic abnormality (SCIWORA) was defined by Pang and Wilberger as ‘objective symptoms of myelopathy as a result of trauma with no radiologic or computed tomographic (CT) evidence of spinal fracture or ligamentous instability’. This definition does not include obstetric complications, congenital spine anomalies and penetrating or electric current spinal injuries [1].
The prevalence of SCIWORA is 6–19% of all pediatric spinal cord injuries [1], having a first peak under the age of 8, and a second in elder patients with spondylosis [2].
In the pediatric population, predisposing factors (such as horizontal orientated facets, ligamentous laxity, anterior vertebral body wedging, weak nuchal musculature and large head-to-trunk ratio) are prone to convey inherent elasticity to the spine, and thus greater capacity to be deformed without being fractured, causing contusion or ischemia due to temporary occlusion of vertebral arteries followed by the return of the spine to its original position [3]. These injuries are normally caused by a hyperextension mechanism, as seen in motor-vehicle accidents. Most of these injuries are observed in the cervical spinal cord [2] and only 9–13% involve the thoracic spine [3].
This syndrome classically presents with clinical-radiologic dissociation, where the main symptom is upper extremity neurological deficit. The onset of clinical symptoms is usually delayed, occurring in the first 48 h post-trauma in 50% of the patients [1].
MRI is the most effective method to evaluate the spinal cord. T1, T2, gradient-echo T2 (T2-GRE) and STIR-weighted MRI sequences show high sensitivity in to detect these lesions [4]. A four-pattern classification is used to describe the outcome and clinical improvement [4]. Pattern 1 is described as normal spinal cord, 2 as single level edema, 3 as multilevel edema and 4 as a mix of hemorrhage and edema [5, 6]. Bozzo et.al [4] described that 65% of the patients showing hemorrhage in the MRI tend to have a more severe American Spinal Injury Association injury grade with a poor outcome, while single level edema tends to a carry a better prognosis.
The most recommended treatment consists in external immobilization [1] of the spine and some authors suggest antihypertensive treatment [7].
CASE REPORT
A 2-year-old female patient was referred to our institution after suffering a motor-vehicle accident. She was admitted under sedation with miotic pupils, left iliac hematoma and cervical collar. At admission, brain, chest, abdominal and pelvic CT scans reported right pneumothorax and a hyperdense hepatic lesion. Spine CT scan showed no fracture or any other pathologic findings (Fig. 1A).
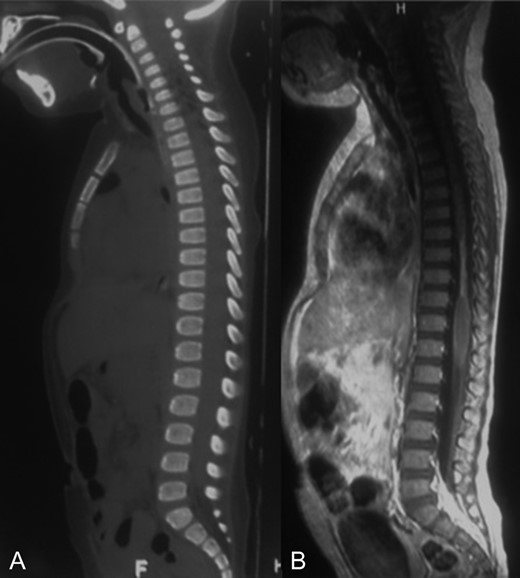
A-B: A. Sagittal bone window of spine showing normal alignment and no fracture. B. Sagittal T1 contrast enhanced sequence showing a narrowed spinal cord from T7 to T10 that could correspond to gliosis and edema.
Extubation was delayed 20 days due to respiratory complications.
Neurological examination showed complete motor and sensory loss under T7 with arreflexia, bladder and bowel dysfunction.
MRI showed a narrowing lesion of the spinal cord from T7 to T10 (Figs 1B, 2A and B).
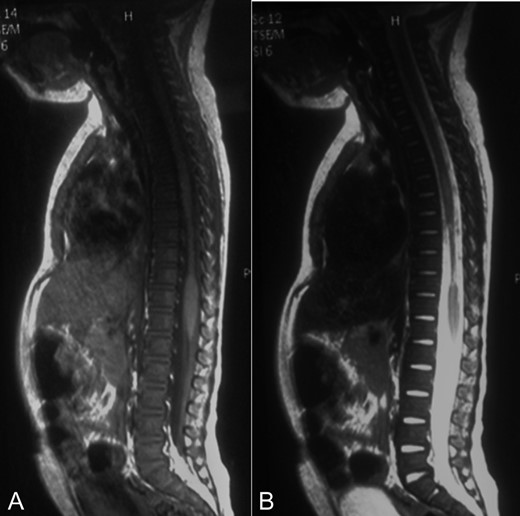
A-B: A. Sagittal T1 sequence showing a narrowed spinal cord from T7 to T10. B. Sagittal STIR-weighted MRI of the thoracic spine showing chronic appearance of a string-like atrophic cord.
The patient was treated with external immobilization of the spine. At 3-month follow-up she presented with paraplegia, positive bilateral Babinski´s and clonus, complete sensory loss under T7, and bladder and bowel dysfunction.
DISCUSSION
SCIWORA represents 19% of the spinal cord injuries in the pediatric population [1], affecting mostly children under the age of 8 [8]. Kasimatis et al. [9] describe that there is a clinical-radiological dissociation, where the main symptom is upper extremity neurological deficit.
MRI shows to be the most accurate method to detect these injuries and describes different patterns that help to predict patient outcome [4]. Bracken et al. suggest that high-dose of methylprednisolone is the only effective treatment for post-traumatic spinal cord edema, in absence of cord compression or instability of the spine [10].
Our case shows coincidence with the literature, as being a 2-year-old patient who suffered spinal trauma featuring clinical-radiological dissociation. The main difference is that she presented with lower limb neurological deficit due to the thoracic localization of the lesion. Although in our case the diagnosis was 20 days post-trauma, we believe that her MRI pattern corresponded to a type 4.
The patient received external immobilization of the spine and no corticosteroids were administrated due to the late diagnosis.
Thoracic SCIWORA is an uncommon diagnosis that should be considered in pediatric patients that suffer spinal trauma with clinical-radiologic dissociation and non-pathological findings on X-Ray or CT. The examination should be followed by a spinal cord MRI which has proven to be the most accurate imaging resource for this type of injuries.
CONFLICT OF INTEREST STATEMENT
None declared.



