-
PDF
- Split View
-
Views
-
Cite
Cite
Yohsuke Yoshioka, Eiki Yamachika, Masakazu Matsubara, Seiji Iida, Okayama University Hospital and Okayama University, Okayama, Japan, Stage IV sporadic Burkitt's leukaemia with osteolysis in the maxillary sinuses, Journal of Surgical Case Reports, Volume 2016, Issue 2, February 2016, rjw011, https://doi.org/10.1093/jscr/rjw011
Close - Share Icon Share
Abstract
We present a case of paediatric Stage IV sporadic Burkitt's leukaemia presenting as cheek enlargement with osteolysis of the maxilla. An 8-year-old boy was referred to our department with diffuse swelling of both cheeks. Head and neck examination revealed bilateral diffuse nontender swelling, non-fluctuant but slightly compressible. Computed tomography imaging showed enhancing bilateral bulky lesions expanding the maxillary sinuses, with associated osteolysis in the posterior walls of both sinuses. Laboratory results included blast cells in the peripheral blood, suggesting a haematopoietic tumour. We referred the patient to the Department of Paediatric Haematology and Oncology. Additional examinations eventually led to the diagnosis of Stage IV sporadic Burkitt's leukaemia.
INTRODUCTION
In the World Health Organization (WHO) classification, Burkitt's lymphoma can be divided into three main clinical variants: the endemic (also called the ‘African variant’), the sporadic (also known as ‘non-African’) and the immunodeficiency-associated (associated with HIV infection) variants. Burkitt's lymphoma accounts for ∼0.8% of all mature B-cell tumours. The leukaemic variant of sporadic Burkitt's lymphoma, presenting with an accumulation of B blasts in the bone marrow, is quite rare [1].
The initial manifestation of sporadic Burkitt's leukaemia in this case was masses in the maxillary sinuses, which is very rare in sporadic, as opposed to endemic, cases [1], and this patient was initially diagnosed with bilateral dentigerous cysts at another hospitals. We present a rare case of Stage IV sporadic Burkitt's leukaemia presenting with masses and bilateral osteolysis in the maxillary sinuses.
CASE REPORT
An 8-year-old boy was referred to our department in September 2014 suffering from pain and swelling of the cheeks. This swelling had increased gradually over a period of 1 month. A diagnosis of dentigerous cysts had been made at another hospital based on computed tomography (CT) findings.
The patient had had general fatigue, anorexia and low-grade fever. Examination of the head and neck revealed nontender, non-fluctuant, slightly compressible diffuse swelling of the cheeks. Intra-oral examination revealed bilateral ill-defined diffuse swelling of the maxilla, extending from the primary molars to the second molars. The overlying mucosa was not inflamed or ulcerated. Vital signs were normal.
A CT examination performed with contrast showed enhancing bilateral expansile masses (right: 3.8 × 3.7 × 2.5 cm, left 3.5 × 3.1 × 2.5 cm) within the maxillary sinuses, with osteolysis of the posterior walls (Fig. 1A).
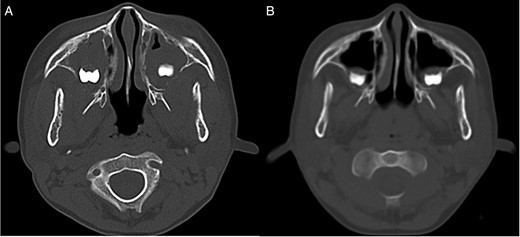
CT image. (A) CT image showing bilateral mass lesions within the maxillary sinuses, with osteolysis involving the posterior walls (right: 3.8 × 3.7 × 2.5 cm, left 3.5 × 3.1 × 2.5 cm). (B) CT image after one course of chemotherapy showing partial reduction of the masses.
Haematology testing showed a slightly increased white blood cell (WBC) count (11.39 × 103/μl) and decreased red blood cell (RBC) (3.64 × 106/μl) and platelet counts (50.0 × 103/μl). Routine chemistry revealed increased lactate dehydrogenase (2864 IU/l), uric acid (17.9 mg/dl), urea nitrogen (30.5 mg/dl), creatinine (1.25 mg/dl) and phosphorus (5.4 mg/dl). Blast cells were found in the peripheral blood. We referred the patient to the Department of Paediatric Haematology and Oncology of our hospital with the presumptive diagnosis of a haematopoietic tumour.
The patient had additional examinations at the department. Bone marrow aspiration from the ilium showed a diffuse monotonous pattern of infiltration by medium-sized cells with round nuclei and basophilic cytoplasm containing vacuoles. Immunophenotype analysis was negative for CD3, TdT, MPO, MIC2 and BCL2 and positive for CD10, CD20, CD79a, c-myc and Ki67 (Fig. 2, data not shown partially). Chromosome banding by fluorescence in situ hybridization (FISH) showed translocations t (8;14)(q24;q32) (data not shown). Positron emission tomography/CT (PET/CT) showed diffusely increased 18F-fluorodeoxyglucose uptake in bone (Fig. 3A). Based on the physical examination, immunohistochemical staining, genetic analysis and imaging findings, the final diagnosis was Stage IV Burkitt's leukaemia.
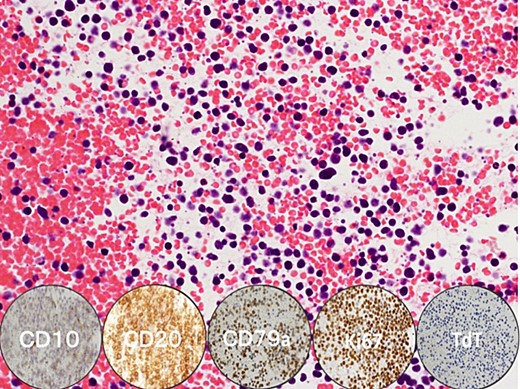
Pathological image. Burkitt's leukaemia stained with haematoxylin & eosin shows infiltration of tumour cells with deeply basophilic cytoplasm, abundant lipid vacuoles in the cytoplasm, multiple small nucleoli and finely dispersed chromatin in the nuclei. Immunostaining was negative for TdT and positive for CD10, CD20, CD79a and Ki67 (circular insets, below).
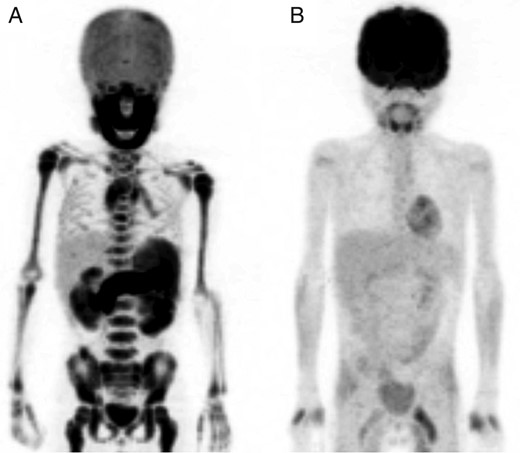
PET/CT image. (A) PET/CT image showing increased 18F-fluorodeoxyglucose uptake in the whole skeleton. (B) PET/CT image after two course of chemotherapy showing complete remission of 18F-fluorodeoxyglucose uptake.
The patient underwent chemotherapy based on the Japanese Paediatric Leukaemia/Lymphoma Study Group B-NHL03 protocol [2]. After one course of chemotherapy, CT images showed partial reduction in the size of the masses in the maxillary sinuses (Fig. 1B). Following two courses of chemotherapy, complete remission of abnormal uptake in the entire body was confirmed by PET/CT imaging (Fig. 3B). To date, the patient is alive and under regular surveillance by the Department of Paediatric Haematology and Oncology.
DISCUSSION
In the WHO classification, Burkitt's lymphoma accounts for ∼0.8% of all mature B-cell tumours. The leukaemia variant of Burkitt's lymphoma, which presents with the accumulation of B blasts in the bone marrow, is quite rare [1]. This case showed osteolysis of the posterior wall of the maxillary sinuses, but the finding of diffuse skeletal involvement has been rarely reported [3] and we were unable to find other reported cases describing involvement of the maxillary sinuses.
The masses in the maxillary sinuses involved the maxillary wisdom teeth. The wisdom tooth begins as a tooth germ at 4 years of age and begins to form a crown with calcification at 7 years. If lymphoma cells appear in the maxilla during this time, the crown may be covered with lymphoma, giving a dentigerous cyst-like appearance on CT as seen in Fig. 1A.
Leukaemic involvement of the jaw is often misdiagnosed as dental infection, cysts or other tumours. However, diagnosis of this disease is often established by finding the presence of blast cells in the peripheral blood, so in those cases biopsy is not required. Delayed diagnosis of Burkitt's leukaemia can have fatal consequences. It is vital to make an accurate diagnosis and referral to the appropriate department for treatment.
CONFLICTS OF INTEREST STATEMENT
None declared.
ACKNOWLEDGEMENTS
We thank Prof. T. Yoshino and Dr T. Tanaka (Department of Pathology, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences Japan) for their assistance in the compilation of data for this paper.



