-
PDF
- Split View
-
Views
-
Cite
Cite
Sean Rezvani, Bachar Zelhof, Alastair Hutchison, Peter Selby, Michael Picton, Ben R. Grey, Dissolution of extensive urolithiasis: extending the utility of rasburicase can avoid the need for surgical intervention and renal replacement therapy, Journal of Surgical Case Reports, Volume 2016, Issue 2, February 2016, rjw009, https://doi.org/10.1093/jscr/rjw009
Close - Share Icon Share
Abstract
A 79-year-old male with chronic myelomonocytic leukaemia and extensive bilateral renal stone disease was treated with intravenous rasburicase for persistent hyperuricaemia. Subsequent imaging revealed a complete dissolution of stone burden, avoiding the need for complex, invasive stone surgery and further renal replacement therapy.
INTRODUCTION
The incidence of nephrolithiasis-induced acute renal failure (RF) is poorly understood. It is thought to account for 3.2% of cases of end-stage renal disease, with uric acid stones implicated in 17.8% of those cases [1].
Rasburicase, a recombinant form of urate oxidase, metabolizes uric acid to the more soluble substance, allantoin. Recent reports demonstrate its benefit in the treatment of tophaceous gout [2–4], uric acid nephropathy [5, 6] and obstructive urolithiasis [7].
We report the case of a 79-year-old male with a background of chronic myelomonocytic leukaemia (CMML) and extensive bilateral stone disease who demonstrated complete stone burden dissolution following the administration of intravenous rasburicase for persistent hyperuricaemia.
We propose the novel use of rasburicase in the treatment of patients with a large uric acid stone burden whereby surgical intervention is difficult or contraindicated.
CASE REPORT
A 79-year-old male with a recent diagnosis of CMML was admitted to hospital with anuria, bilateral hydronephrosis and significant RF with an estimated glomerular filtration rate (eGFR) of 4 ml/min/1.73 m2.
He underwent bilateral nephrostomy insertion and required haemodialysis on two occasions for a raised creatinine of 1044 umol/l (reference range 59–104 µmol/l), which subsequently reduced and stabilized to a level of around 500 µmol/l, with an eGFR of 11 ml/min/1.73 m2.
His plasma urate was significantly raised at 1.2 mmol/l (reference range 0.17–0.48 mmol/l). Following the decision to administer 12 mg of intravenous rasburicase, his persistently elevated serum urate became undetectable at <0.1 mmol/l.
The aetiology of his RF was attributed to extensive bilateral ureteric calculi and a left-sided partial staghorn calculus, presumably of uric acid composition (Fig. 1).
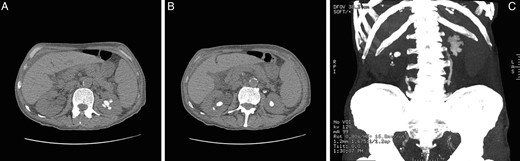
Computed tomography of kidneys, ureters, bladder images demonstrating stone load in a 79-year-old male with CMML, prior to treatment with rasburicase. (A) Partial left-sided stag horn calculi. (B) Bilateral lower pole calculi. (C) Coronal reconstruction demonstrating total renal and ureteric stone load.
Six weeks post nephrostomy insertion, his renal function remained at the pre-dialysis stage. To avoid encrustation of the prosthetic material, the patient was subsequently admitted for nephrostomy exchange and a repeat computed tomography (CT) scan to reassess stone load and plan future surgical intervention.
Thought was given to the introduction of alkalinizing agents through the nephrostomies to debulk the stone burden and thereby, hopefully, reducing the complexity and invasiveness of surgery. However, repeat CT scanning demonstrated a complete dissolution of the entire stone load.
In the weeks following, his bilateral nephrostomies were removed, and the patient experienced an improvement in eGFR without the need for further dialysis.
DISCUSSION
It was unclear as to whether this patient's CMML was ultimately responsible for his hyperuricaemia. He had received cytoreduction treatment for CMML in the months preceding; however, he was known to have had renal calculi in the past and radiological evidence of joint crystallization some 30 years previously without symptoms of gout.
Uric acid-related RF may develop through either direct urinary tract obstruction or as a result of urate crystal deposition within the kidney interstitium and collecting ducts [4]. Recent studies have also suggested that uric acid may augment acute kidney injury through inflammatory-mediated renal vasoconstriction and anti-angiogenic effects [8].
The degree to which each pathology contributed to this patient's RF can only be inferred. Though acute anuria, hydronephrosis and CT findings point to a primary obstructive picture, the slow renal recovery and hyperuricaemia could equally point to an underlying nephropathy.
Regardless of origin, the finding of complete stone dissolution following intravenous rasburicase is remarkable and worthy of reporting. To the best of our knowledge, there are only two reported cases of uric acid stone dissolution following the administration of rasburicase for nephrolithiasis-induced RF [7].
Rasburicase is a recombinant form of urate oxidase, an enzyme which metabolizes uric acid to allantoin, a more water-soluble compound [4, 7]. Its use is well established in the prevention of tumour lysis syndrome, a critical illness whereby chemotherapy-induced tumour cell death leads to significant hyperphosphataemia, hypocalcaemia and hyperuriceamia [4, 9].
Depending on the degree of hyperuricosuria and urinary pH, uric acid may become supersaturated in the urine leading to precipitation and crystallization within the medulla of the kidney [9, 10]. A rapidly progressive renal impairment often ensues, necessitating the use of renal replacement therapy.
With a molecular weight of 34 kDa, rasburicase is theoretically able to pass through the glomerular filtration system in quantities comparable with other similar weighted human plasma proteins. Segura Torres et al. postulate that due to this low molecular weight, rasburicase is able to exert its enzymatic effect within the renal calyces, pelvis and ureters [7].
Current European Association of Urology guidelines state uric acid stones can be treated through percutaneous dissolution with tris(hydroxymethyl)aminomethane solutions; however, oral chemolysis with potassium citrate, allopurinol and a high fluid intake are preferable.
This case demonstrates that rasburicase offers an intravenous therapeutic option for those in whom surgery is not possible or contraindicated. In this case, as a consequence of the rasburicase, the patient did not need dialysis, surgery or long-term nephrostomies. Doubtless, this improved the patient's quality of life and meant that he was not exposed to the risks of surgical intervention in a patient with significant comorbidity.
CONFLICT OF INTEREST STATEMENT
None declared.



