-
PDF
- Split View
-
Views
-
Cite
Cite
Annabel Stout, Lakshmi Santharam, Nazzia Mirza, A rare case of jejuno-ileal intussusception secondary to a gastrointestinal stromal tumour, Journal of Surgical Case Reports, Volume 2015, Issue 1, January 2015, rju142, https://doi.org/10.1093/jscr/rju142
Close - Share Icon Share
Abstract
Gastrointestinal stromal tumours (GISTs) are rare tumours, making up 0.2–1% of gastrointestinal malignancies [Zakaria and Daradkeh (Jejunojejunal intussusception induced by a gastrointestinal stromal tumour. Case Rep Surg 2012;2022:173680)]. Their relative rarity combined with non-specific presentation results in tumours often remaining undiagnosed until surgery or histological examination [Martis et al. (A rare case of jejunojejunal intussusception in an adult. Indian J Surg 2013;75(Suppl 1):18–20)]. Presentation as a lead point for intussusception is particularly rare. We present the first case of GIST leading to intussusception at the jejuno-ileal junction in an otherwise well patient prior to presentation. Provisional diagnosis was made during emergency laparotomy, and confirmed through histological analysis. A typical immunohistochemical profile was identified, after which the patient was commenced on adjuvant imatinib therapy. We discuss classical presentation of intussusception and GIST. Further considerations of the investigation and treatment options of GISTs are also presented.
INTRODUCTION
Gastrointestinal stromal tumours (GISTs) are rare tumours of the GI tract, making up 0.2–1% of gastrointestinal malignancies [1]. First identified by Mazur and Clark in 1983 [2], these mesenchymal tumours can occur anywhere along the gastrointestinal tract [1, 3]. Relative rarity combined with non-specific presentation results in delayed diagnosis [4, 5]. Their presentation as a lead point for intussusception is particularly rare. We present the first case of GIST leading to intussusception at the jejuno-ileal junction in an otherwise well patient prior to presentation.
CASE REPORT
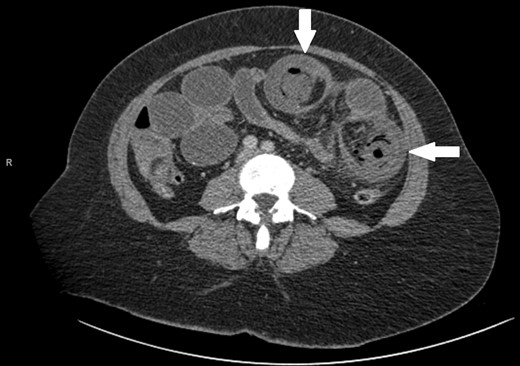
A 47-year-old female presented as an emergency with severe abdominal pain and profuse vomiting. She had been experiencing symptoms of intermittent vague abdominal pain associated with weight loss over 6 months, but no change in bowel habit. She had no significant past medical history. On examination she was tachycardiac, pyrexial and abdominal examination revealed distended abdomen with localized tenderness in the left iliac fossa. Blood tests revealed an elevated white cell count (18.8), C-reactive protein (25), microcytic anaemia (Hb 108) and a mildly raised lactate (2.37). She was commenced on intravenous fluids. An abdominal plain film showed prominent bowel loops and ultrasound of the abdomen revealed numerous loops of a distended, fluid filled, non-peristalsing bowel. There was some evidence of bowel wall thickening, but no clear source of obstruction was identified. A CT scan was performed showing mesenteric vascular gas and a target sign, virtually pathognomonic of intussuception [5, 6] (Figs 1 and 2).

The patient underwent a laparotomy, which revealed small bowel obstruction with evidence of impending perforation. A pedunculated polypoid lesion at the jejuno-ileal junction was identified as the lead point for intussusception. The intussuscepted segment of small bowel was resected and end-to-end primary anastomosis formed.
Postoperatively, the patient made a satisfactory recovery and was discharged a week later. Histological findings were in keeping with a 75-mm GIST, jejuno-ileal in origin, with a mitotic count of <5/mm2 and a moderate (24%) risk of recurrence. The tumour was positive for CD117 and carried a c-KIT mutation with a deletion in exon 11.
The patient was subsequently commenced on adjuvant imatinib therapy.
DISCUSSION
Intussusception is the telescoping of a proximal loop of bowel and its mesentery (intussusceptum) into the lumen of bowel distal to it (intussuscipiens) [5]. The phenomenon is rare in adults and presents with non-specific symptoms, such as recurrent abdominal pain, nausea and vomiting. Up to 90% of adult cases have a defined lesion acting as the lead point, which is malignant in overhalf of cases [1, 6].
While correct diagnosis is based on operative findings, suspicion may be raised following imaging techniques. CT with both oral and intravenous contrast is now widely recognized as the most accurate diagnostic tool (58–100% accuracy in a recent case series) [1, 4]. Alternating hyper- and hypodense layers of the bowel wall of the intussuscepted segment give rise to a classical ‘target sign’ [5] (Fig. 1).
GISTs are rare tumours demonstrating a broad spectrum of invasiveness [5, 7] and unpredictable behaviour, with recent suggestion that these tumours should no longer be classified as benign or otherwise [7].
Classically GISTs grow exophytically, into the peritoneal cavity or adjacent organs [5], further decreasing their likelihood of causing an intussusception. Rarely, however, GISTs can grow as a pedunculated polyp, as in our case, which may go on to act as a lead point for an intussusception [3]. Their growth pattern leads to a range of non-specific symptoms (much like an intussusception), meaning GISTs often remain unnoticed until advanced enough to cause complications such as ulceration, obstruction or GI bleed [1].
A definitive diagnosis requires histological analysis of a resected specimen. GISTs originate from a malignant transformation of the interstitial cells of Cajal [1, 3]. 95% of cases show a mutation in the KIT proto-oncogene [8], setting them apart from leiomyomas, leiomyosarcomas and schwannomas of the small intestine. Furthermore, near universal expression of CD117—a product of the KIT proto-oncogene which makes up part of the KIT transmembrane receptor tyrosine kinase—is found [3]. Again, this is typically negative in alternative tumours situated in the GI tract. The haematopoietic progenitor cell CD34 is also present in 70–80% of cases [8].
Following the relatively recent discovery of this immunohistochemical profile, management of GISTs has been transformed. Imatinib, a targeted tyrosine kinase inhibitor, has revolutionized treatment since its introduction in 2001. Universal guidelines for its use are not currently available; however, it has a clear role in both adjuvant therapy and neoadjuvant therapy for unresectable or borderline resectable tumours [1, 3, 9, 10].
Prior to the introduction of imatinib, surgery was the only treatment available and to this day offers the only chance of cure [8]. Surgery is offered for all tumours over 2 cm in diameter, along with a role in debulking or symptomatic relief [10]. Below 2 cm the natural history of these rare tumours is relatively unknown; therefore, treatment planning is difficult. Segmental resection should be performed rather than a peritumoural approach. Given the rarity of spread to lymph nodes, regional lymphadenectomy has not been found to be useful [10].
Intussusception is a rare finding in adults, even more so when occurring secondary to a gastrointestinal stromal tumour. We present the first case of a jejuno-ileal intussusception secondary to a GIST in an otherwise well patient. Diagnosis can be difficult given the non-specific nature of the symptoms, and while different imaging modalities may be useful in evaluating these patients, a firm diagnosis cannot be made until histological analysis. Curative treatment can only be offered by surgery; however, imatinib has a role in both adjuvant and neoadjuvant treatment.



