-
PDF
- Split View
-
Views
-
Cite
Cite
António Gomes, Vanessa Santos, Gonçalo Dias, Rita Theias Manso, Lucília Gonçalves, Margarida Coiteiro, Helena Gaspar, Antónia Nazaré, An 18-year-old woman with a 34-cm metaplastic breast carcinoma, Journal of Surgical Case Reports, Volume 2015, Issue 1, January 2015, rju141, https://doi.org/10.1093/jscr/rju141
Close - Share Icon Share
Abstract
Metaplastic breast carcinomas (MBCs) are rare malignancies usually with poor prognosis. We report a case of an 18-year-old African female patient who presented with a 34-cm tumor on the right breast. Biopsy showed an extensively necrotic MBC negative for estrogen receptor, progesterone receptor and human epidermal growth factor receptor 2 (triple negative). A modified right radical mastectomy was performed, followed by adjuvant chemotherapy. Histology confirmed a widely necrotic undifferentiated malignant tumor, with strong and diffuse expression of vimentin and B-cell lymphoma 2, focal high-molecular-weight keratins and focal CD34 expression; Ki67 was >90%. There was no skin, deep margin or lymph node involvement. Six months after surgery, the patient showed a 9 × 7 cm nodule adjacent to the suture and adherent to the anterior chest wall. The tumor was considered unresectable and the patient evolved with rapid systemic deterioration. The patient had a progression-free survival of 6 months and overall survival of 9 months.
INTRODUCTION
Metaplastic breast carcinoma (MBC) is a rare aggressive breast malignancy with poor prognosis [1]. There are no specific recommendations for MBC management, the standard regimen being surgery combined with adjuvant therapy, although there is evidence to suggest that MBCs have lower response rates to conventional adjuvant chemotherapy and a worse clinical outcome than other forms of breast cancers negative for estrogen receptor, progesterone receptor and human epidermal growth factor receptor 2 (triple negative) [2]. In younger women, breast cancer is associated with even worse outcomes [3]. We report a case of an 18-year-old African female patient with MBC, who was subjected to the standard of care, but had a progression-free survival (PFS) of 6 months and an overall survival (OS) of 9 months, thus supporting the poor prognosis of MBC in young women.
CASE REPORT
An 18-year-old African female patient with no relevant past or family history was admitted at our hospital due to a 34-cm tumor on the right breast (Fig. 1). The patient, from Cape Verde, delayed her appointment with a doctor because she could not afford to miss a day at work. When she finally went to the doctor, due to rapid growth of the mass, the tumor was extremely large, and she was immediately evacuated to Portugal. Biopsy showed an extensively necrotic MBC, triple negative, with Ki67 >90%. Thorax, abdomen and pelvic CT showed axillary lymph node involvement, without other secondary foci. Breast MRI showed probable muscle infiltration (Fig. 2). A multidisciplinary team decided that a modified right radical mastectomy should be performed (Fig. 3).

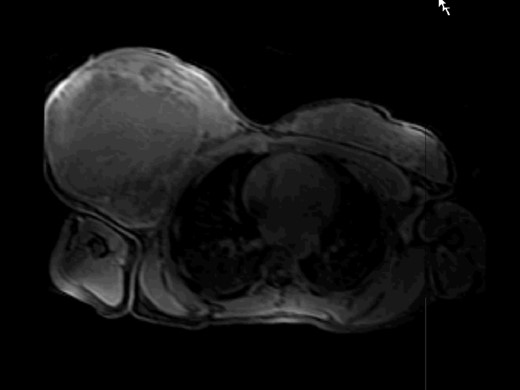
MRI T1f study after paramagnetic contrast showing a large mass occupying the entire right breast with extensive central necrosis.
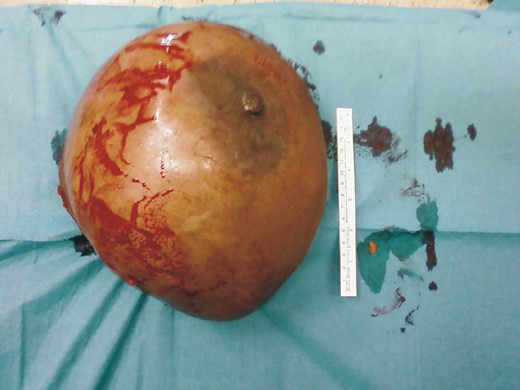
Pathology confirmed a widely necrotic tumor with ∼3500 g and 34 cm, replacing the whole breast. Histology showed atypical spindle and some epitheliod cells, with high nuclear pleomorphism, organized in long fascicles with an interwoven pattern and in a hemangiopericytoid fashion (Fig. 4A and B); the mitotic index was high, with >20 mitosis/10 high-power fields. There was focal expression of high-molecular-weight keratins CK903 and AE1/3 (Fig. 4C), and CD34; Ki67 was >90%. Neoplastic cells strongly and diffusely expressed vimentin (Fig. 4D) and B-cell lymphoma 2. The tumor was triple negative and also negative for HMB45, desmin and actin. Skin and deep margin showed no evidence of neoplasia. None of the 12 isolated lymph nodes showed tumor invasion (pT3N0). Based on the unequivocal expression of high-molecular-weight keratins [2], a diagnosis of metaplastic spindle cell carcinoma was rendered.
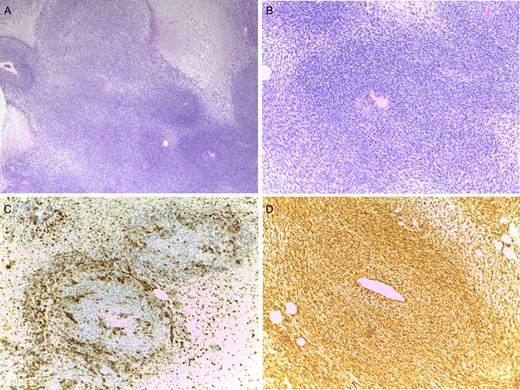
(A) Spindle cell proliferation with a hemangiopericitoid growth pattern (×4). (B) Nuclear pleomorphism and numerous mitoses (×10). (C) Focal expression of CK903, revealing epithelial differentiation (×10). (D) Strong and diffuse expression of vimentin (×10).
The patient underwent adjuvant therapy with four cycles of doxorubicin and cyclophosphamide. Six months after surgery, the patient showed a hard and painful nodule adjacent to the suture and adherent to the chest wall. Ultrasound confirmed a heterogeneous multicystic nodule of 9 × 7 cm (Fig. 5). Chest CT revealed right pleural effusion, pleural thickening and consolidation of the adjacent parenchyma. Cytological analysis raised a suspicion for the presence of malignant cells. Pleural biopsy was negative for malignancy.
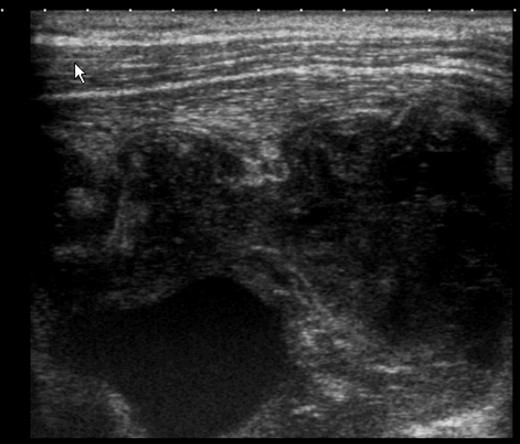
Ultrasound of the mastectomy bed showing a hypoechoic solid mass in subpectoral topography with signs of muscle invasion.
Given the chest wall involvement, the tumor was considered unresectable and the patient evolved with rapid systemic deterioration and multiple organ failure. PFS was 6 months and OS 9 months.
DISCUSSION
Young women are more likely to develop more aggressive subtypes of breast cancer with poor prognosis, probably due to multiple factors, including unfavorable disease biology, delay in diagnosis and age [3]. On the other hand, MBCs are aggressive regardless of age, usually characterized by rapid progression, needing immediate surgical treatment and en bloc resection. MBCs account for 0.2–5% of all invasive breast cancers [2], which usually present as high-grade neoplasms with a large tumor size, less likely nodal involvement, triple negative, poorly differentiated or undifferentiated [1, 4, 5] and high Ki67 [6]. Our patient presented with these characteristics, but was much younger than the reported mean age of 61–63 years [1, 4, 6]. Also, the tumor was much larger than the reported range of 3.4–13 cm [7, 8].
Although with the use of neoadjuvant therapy for downstaging and downsizing, together with currently available oncoplastic techniques, it is possible to perform conservative breast oncologic surgery in cases previously treated with radical mastectomy, our first surgical option was a modified right radical mastectomy given the exceptionally large tumor, followed by adjuvant chemotherapy. The use of adjuvant therapy has been the subject of some debate [1, 4, 6–8]. In our case, adjuvant hormonal therapy was not an option given the tumor was triple negative. Since there is no standard treatment regimen specific for MBC, we followed the clinical practice guidelines for invasive breast adenocarcinoma [8], and adjuvant chemotherapy was decided by our breast cancer multidisciplinary group, given it is used more often for patients with MBC [4]. Also, its use in breast cancer is based on disease stage, not histologic subtype [1], as the prognostic value of histological grading in MBCs is uncertain [2]. Owing to several clinical complications arising during the CT cycles, relapse and deterioration of the patient's general health status, adjuvant radiotherapy could not be offered.
Despite the aggressive treatment, our patient relapsed 6 months after surgery and had an OS of 9 months. PFS and OS of our patient were much lower than in other studies [1, 5, 8]. This dismal scenario was not surprising given the tumor presentation at hospital admittance and the patient's age and ethnicity. Not only breast cancer in young women has been associated with more aggressive, poorly differentiated, estrogen receptor (ER) negative tumors, but also African-American women have an increased risk of breast cancer at younger ages and are more likely to have higher grade, ER-negative cancers [3].
Presently, there are no validated prognostic markers for metaplastic carcinomas [2]. It is of paramount importance to rapidly identify these tumors and treat them aggressively, which can only be achieved with a multidisciplinary approach. The case we report did not have a good outcome, for a number of reasons. Although MBC is rare, there are still a significant number of patients who, due to limited access to primary health care, present with very advanced tumors at hospital admittance, and there is a need to know how to manage these patients, in order to achieve the best possible outcome.
The procedures followed were in accordance with the ethical standards of the Helsinki Declaration of the World Medical Association. The patient's written consent was obtained. The work has been approved by the Hospital Professor Doutor Fernando da Fonseca ethical committee.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- b-cell lymphomas
- biopsy
- cancer
- carcinoma
- adjuvant chemotherapy
- cd34 antigens
- keratins
- ki-67 antigen
- mastectomy, radical
- necrosis
- epidermal growth factor receptors
- estrogen receptors
- receptors, progesterone
- surgical procedures, operative
- sutures
- vimentin
- breast
- histology
- lymph nodes
- neoplasms
- skin
- surgery specialty
- metaplastic carcinoma of breast
- anterior chest wall
- progression-free survival



