-
PDF
- Split View
-
Views
-
Cite
Cite
Eduardo Crema, Eliane Anrain Trentini, Celso Júnior Oliveira Teles, Paulo Ricardo Monti, Croider Franco Lacerda, Juverson Alves Terra Junior, Alex Augusto Silva, Laparoscopic reconstruction of the extrahepatic bile duct using a jejunal tube: an innovative, more physiological and anatomical technique for biliodigestive derivation, Journal of Surgical Case Reports, Volume 2014, Issue 1, January 2014, rjt106, https://doi.org/10.1093/jscr/rjt106
Close - Share Icon Share
Abstract
The incidence of bile duct injuries has increased as a consequence of the increasing number of cholecystectomies. However, the results of biliodigestive derivation currently used for bile duct reconstruction are unsatisfactory. We report here the case of a patient with iatrogenic Bismuth II bile duct injury and propose a new technique that permits more anatomical and physiological reconstruction of extensive bile duct injuries using transverse retubularization of a pedicled jejunal segment interposed between the bile duct and duodenum.
INTRODUCTION
As a consequence of the increase in the number of cholecystectomies and the learning curve of surgeons, the incidence of bile duct injuries has also increased, ranging from 0.1 to 0.3% in laparoscopic procedures even at referral centers [1–5]. Among iatrogenic injuries, bile duct injury has a greater clinical significance because of its potential to produce disability and long-term sequelae [6].
Since in most cases the borders of the bile duct are separated and/or the distal portion cannot be identified, bile duct reconstruction is frequently performed by choledochoduodenal or choledochojejunal bypass drained through an excluded loop of a jejunal segment of ∼40–60 cm (Roux-en-Y reconstruction) [7].
We propose a new technique consisting of the interposition of a tube of jejunum between the dilated common bile duct and duodenum in an attempt to restore the bile duct with a short segment of the small bowel whose caliber is proportional to that of the duct and to minimize obstruction caused by the circular folds of the jejunal segment. This procedure of interposition of a tube of small bowel segment was performed similar to the technique proposed by Monti [8, 9] for continent diversion of neobladders.
This study reports the first case of reconstruction of bile duct transit after extensive iatrogenic injury by transverse retubularization of a pedicled jejunal segment, which was based on the study of Crema et al [10].
CASE REPORT
A 41-year-old man was referred to the University Hospital, Department of Digestive Surgery, Triangulo Mineiro Federal University, with jaundice, choluria and fecal hypocholia. The patient had undergone laparotomic cholecystectomy 2 days earlier. Upon physical examination, the patient was in good general health, pale (1+/4+), hydrated, jaundiced (1+/4+) and afebrile. The abdomen was slightly tender and bowel sounds were reduced. Abdominal ultrasonography performed on admission demonstrated dilatation of the intrahepatic bile ducts and only the proximal portion of the common hepatic duct was seen. The patient presented hyperbilirubinemia. Gamma-glutamyl transferase (γ-GT) was 235.4 U/L, alkaline phosphatase 187.6 U/L, aspartate aminotransferase (AST) 183.4 U/L and alanine aminotransferase (ALT) 485.7 U/L.
The patient was submitted to surgical intervention. Inspection showed a small fistula (probably the duct of Luschka [6]) in the gallbladder bed, the common hepatic duct was sectioned with loss of substance between segments, and the proximal and distal stumps were ligated with cotton suture. Next, catheterization of the fistula in the duct of the gallbladder bed was performed with a No. 4 Levine catheter. Cholangiography showed moderate dilatation of the intrahepatic bile duct and a sudden obstruction in the common hepatic duct 1 cm from the confluence of the hepatic ducts, corresponding to bile duct injury classified as Bismuth II (Fig. 1).
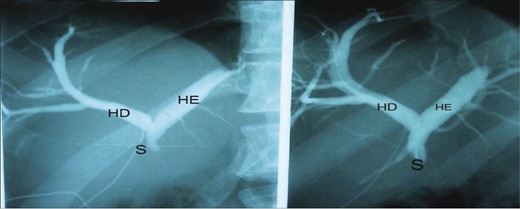
Right hepatic duct (RH), left hepatic duct (LH) and obstructed common hepatic duct (O).
The intervention chosen was reconstruction of the bile duct by interposition of a pedicled jejunal segment between the hepatic duct bifurcation and duodenum. A 5-cm segment was cut from the jejunal loop at a distance of 40 cm from Treitz angle (Fig. 2) and divided into two segments of 2.5 cm, each containing their respective vascular pedicles (Fig. 3).
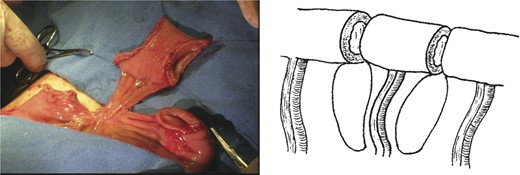
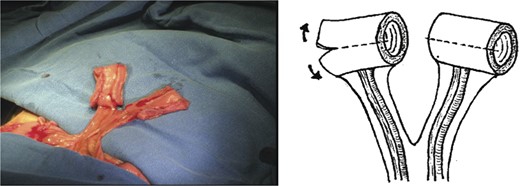
The mesenteric and antimesenteric borders of the two segments were cut longitudinally (Fig. 4), promoting jejunal detubularization and forming two separate pedicled rectangles (Fig. 5). Side-to-side anastomosis proximal to the pedicle was performed with 3-0 continuous sutures of polyglactin 910 (Vicryl®) on a single plane.

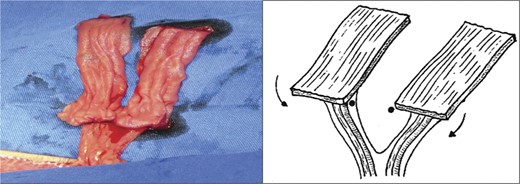
Transverse retubularization of the loop was performed with a No. 12 Levine catheter as a mold. A 21-cm tube was created using 3-0 continuous sutures of polyglactin 910 (Vicryl®) (Figs 6 and 7). The size of the tube was reduced to 15 cm by resection of the distal ends by ∼3 cm. A transmesocolic passage for the tube was created and an entero-enteral anastomosis was performed for reconstruction of jejunal transit.

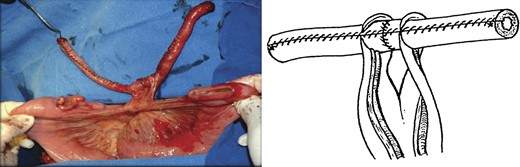
The tube was formed and the common hepatic duct was anastomosed with interrupted 3-0 polypropylene (Prolene®) sutures. A longitudinal incision of ∼3 cm was made in the second portion of the duodenum, comprising the serous and muscle layers and preserving the mucosa.
The Levine catheter was maintained and exteriorized through the opening in the duodenum for subsequent radiological control and external biliary drainage into the duodenum.
Magnetic resonance cholangiography performed 45 months after surgery showed a functioning tube (Fig. 8). The patient continues to be anicteric and laboratory tests are normal.
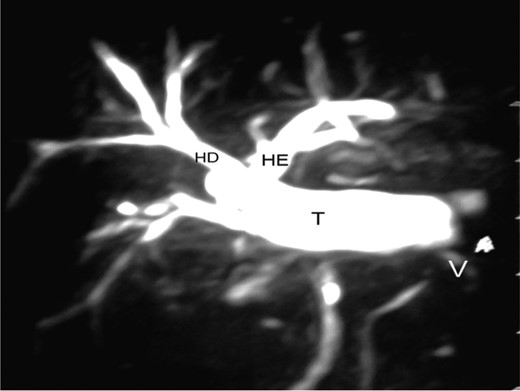
Right hepatic duct (RH), left hepatic duct (LH), interposed jejunal tube (T) and antireflux valve (V).
DISCUSSION
The Monti procedure described in 1997 is a major contribution to the treatment of different urinary tract disorders. This procedure was adapted in the present case for the reconstruction of the bile duct, showing extensive injury and an indication for biliodigestive derivation.
The incidence of intestinal reflux to the bile duct is lower in the case of excluded Roux-en-Y loop reconstruction. However, the disadvantages of this approach include bile duct stenosis, secondary biliary cirrhosis and ascending cholangitis. In addition, since the procedure is not anatomical, it deviates the flow of alkaline bile to the duodenum, causing long-term problems of peptic ulcer and impairing or preventing endoscopic access to the bile duct for diagnostic and therapeutic purposes.
The objective of this study was to propose a new type of reconstruction of extensive bile duct injuries that is more anatomical and physiological.
In 2006, Crema et al. [10] published a study investigating the efficacy of interposition of a jejunal tube between the dilated bile duct and duodenum in adult dogs as a technical option for bile duct reconstruction. Regression of jaundice was observed in all animals at the end of the study, confirming that the interposed tube was effective in the conduction of bile.
This technique has been applied so far to seven patients, four with bile duct stenosis and three with bile duct cysts. Postoperative evolution of the patients was satisfactory and bile duct permeability was restored in all cases.
The interposition of a jejunal tube for bile duct reconstruction was satisfactory and efficient. The procedure is simple and technically reproducible and represents a new option for the reconstruction of extensive extrahepatic bile injuries.
CONFLICT OF INTEREST
All authors warrant that they have sole ownership of the work submitted, that the work is original and has never been published, and the authors have full powers to grant such rights.
There are no conflicts of interest. All authors have substantial contribution in this work, as the analysis and interpretation of data, writing and critical review, stating that participated sufficiently in the work to take public responsibility for the content.
REFERENCES
Author notes
The study was performed at the Department of Digestive Surgery, Triangulo Mineiro Federal University (UFTM), Minas Gerais, Brazil.



