-
PDF
- Split View
-
Views
-
Cite
Cite
Tarik Deflaoui, Anas Derkaoui, Mohammed Hassani, Rihab Amara, Abdelali Guellil, Rachid Jabi, Mohammed Bouziane, Left anterior paraduodenal hernia: a rare observation and clinical implications, Journal of Surgical Case Reports, Volume 2025, Issue 3, March 2025, rjaf120, https://doi.org/10.1093/jscr/rjaf120
Close - Share Icon Share
Abstract
Paraduodenal hernias account for ~53% of internal hernias due to embryological anomalies in intestinal rotation. While left paraduodenal hernias are the most common type, the anterior left variant is exceptionally rare. It involves herniation of the small intestine in front of the duodenum through a mesenteric defect. We present a case of a left anterior paraduodenal hernia diagnosed and surgically treated in our department, along with a discussion of its clinical and therapeutic aspects.
Introduction
Intestinal obstruction caused by internal hernias is rare, accounting for only 1%–5% of cases of acute bowel obstruction [1]. Among these, paraduodenal hernias (PDH) are the most common, representing 53%, but the anterior left variant is extremely rare. This anomaly arises from abnormal midgut rotation, leading to defects in the mesentery or mesocolon [2]. Given its nonspecific clinical presentation, diagnosing this condition can be challenging. Computed tomography (CT) is critical for identifying such abnormalities [3]. Treatment is surgical, aiming to reduce the hernia and prevent recurrence or complications [4].
Case presentation
A 45-year-old man with no significant medical history presented to the emergency department with acute epigastric pain accompanied by bilious vomiting. Physical examination revealed epigastric tenderness without guarding or signs of peritonitis.
Abdominal CT revealed a cluster of small bowel loops in front of the duodenum on the left side of the midline, associated with proximal mechanical obstruction. These findings were consistent with a left paraduodenal hernia.
Laparotomy confirmed a left anterior paraduodenal hernia, with the small bowel incarcerated through a defect in the mesocolon. The herniated bowel was manually reduced, and the defect was enlarged to prevent recurrence. There were no signs of strangulation. The patient had an uncomplicated postoperative recovery (Fig. 1 and Video 1).
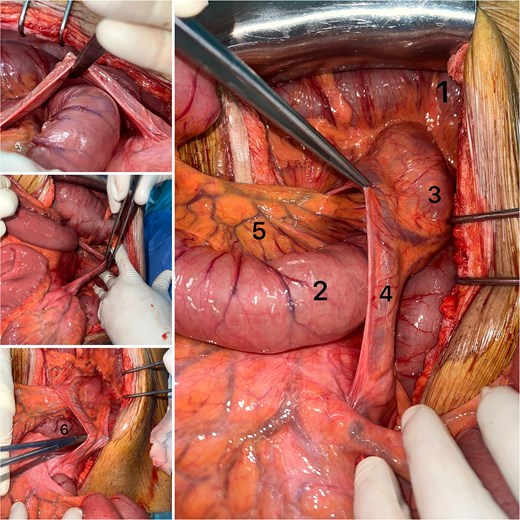
Left anterior paraduodenal hernia. (1) left colic flexure, (2) ileum, (3) descending mesocolon, (4) ascending left colic artery, (5) mesentery, (6) jejunum.
Discussion
Paraduodenal hernias result from abnormal midgut rotation, leading to defects in the transverse mesocolon [2]. In the left variant, the small intestine herniates through an opening anterior to the ligament of Treitz. The anterior left variant, although exceptionally rare, can lead to serious complications such as intestinal obstruction or ischemia [4, 5].
Patients often present with recurrent abdominal pain or acute obstructive symptoms. CT imaging is the diagnostic modality of choice, typically showing clustered small bowel loops to the left of the midline with signs of proximal obstruction and displaced mesenteric vessels [6, 7].
Blachar et al. emphasized the role of CT in differentiating internal hernias and proposed specific diagnostic criteria for paraduodenal hernias [8]. Uematsu et al. highlighted laparoscopy as a valuable diagnostic and therapeutic tool [9].
The treatment for paraduodenal hernias is exclusively surgical. This involves reducing the herniated bowel and widening the hernia defect to prevent recurrence. Unlike other types of hernias, closing the defect is generally avoided to prevent vascular compromise or secondary obstruction [10].
Conclusion
Left anterior paraduodenal hernia is a rare clinical entity with significant implications. Prompt recognition through imaging and appropriate surgical management are essential to prevent severe complications.
Conflict of interest statement
None declared.
Funding
None declared.



