-
PDF
- Split View
-
Views
-
Cite
Cite
Andrea Pires Damin, Bibiana Quatrin Tiellet, Marcia Portela de Melo, Angela E Zucatto, Rodrigo Cericatto, Jorge Villanova Biazus, Case report of the combination of a TRAM flap, lipofilling, and 3-D tattooing after failed implant-based reconstruction: improving aesthetic results, Journal of Surgical Case Reports, Volume 2024, Issue 9, September 2024, rjae581, https://doi.org/10.1093/jscr/rjae581
Close - Share Icon Share
Abstract
We present a complex case of a patient diagnosed with bilateral breast cancer. The patient initially underwent bilateral skin-sparing mastectomy and immediate subpectoral implant-base breast reconstruction. She had an uncomplicated postoperative recovery. However, three months later, she developed a severe and persistent local infection during adjuvant chemotherapy, resulting in the loss of the breast implants and the formation of massive deforming scars in the chest area. To address this, the patient underwent a series of reconstructive procedures. Lipofilling was used on the chest wall to improve skin quality, followed by a late bilateral transverse rectus abdominis myocutaneous flap for breast reconstruction. Additionally, the final aesthetic result was enhanced by applying a 3-D tattoo. This case highlights the use of a sequence of reconstructive procedures as a feasible alternative to manage complex and extensive scars after failure of primary breast reconstruction.
Introduction
Following mastectomy, immediate implant-based reconstruction is currently the most common method used in breast reconstruction [1]. The advantages of implant-based breast reconstruction over autologous breast reconstruction include a shorter procedure time, shorter hospital stay, and faster overall recovery [2]. However, implant loss can occur in approximately 8% of patients, usually due to surgical site infection (SSI), which is a serious complication requiring complex therapeutic interventions [3].
Most SSI complications occur within 30 days following the procedure, but late infections have been observed months or even years after implant-based breast reconstruction. Late SSI can lead to a higher rate of implant failure and more severe consequences [4].
Breast reconstruction after an implant failure poses a therapeutic challenge, particularly following radiotherapy. Using a patient’s own tissue for restoration can be an effective alternative [5]. Additionally, lipofilling can be used to improve the results of both autologous and implant breast reconstruction, as well as to enhance skin quality [6–8].
We present the case of a patient who experienced late SSI after immediate bilateral implant-based breast reconstruction, which led to implant failure and scar formation. A series of procedures were performed for breast reconstruction, resulting in favorable aesthetic outcomes. Importantly, even in a severe surgical scar scenario, it is possible to recover the patient’s self-steam with a series of surgical procedures.
Case report
A 45-year-old woman with bilateral breast invasive carcinomas of no special type underwent bilateral skin-sparing mastectomies and immediate subpectoral implant-based breast reconstruction. Pathology of the right breast revealed a grade 2 tumor measuring 1.3 cm in maximum diameter, and that of the left breast revealed a grade 3 tumor measuring 4.5 cm in maximum diameter. Direct axillary dissection was performed on the right side, which revealed 2 positive nodes with extranodal extension out of 13 retrieved lymph nodes. On the left side, a sentinel node procedure recovered two axillary nodes without metastasis. Both breast tumors were classified as luminal A carcinomas. The patient subsequently underwent adjuvant chemotherapy with docetaxel, doxorubicin (A), and cyclophosphamide (C). During the second cycle of AC, 3 months after the surgical procedure, she developed marked redness in both reconstructed breasts, indicating extensive infection of the surgical site. The breast implants were removed, followed by several surgical interventions to remove infected and necrotic tissues, which eventually resulted in the formation of extensive deforming scars in the chest (Fig. 1A and B). She subsequently received radiotherapy on both sides of the chest wall. After finishing radiotherapy, she started receiving tamoxifen. Four years after the initial procedure, breast reconstruction was again proposed. The first step of the process involved lipofilling of the chest wall and bilateral laparoscopic ligation of the deep inferior epigastric arteries (Fig. 1C and D). After 4 months, the patient underwent bilateral reconstruction with a combination of transverse rectus abdominis myocutaneous (TRAM) flaps and lipofilling (392 cc on the left and 484 cc on the right side) (Fig. 1E and F). The nipple–areola complex was reconstructed with local flaps (Fig. 2A and B). Two months after late surgery, a 3D tattoo improved the final aesthetic result. (Fig. 2C and D).
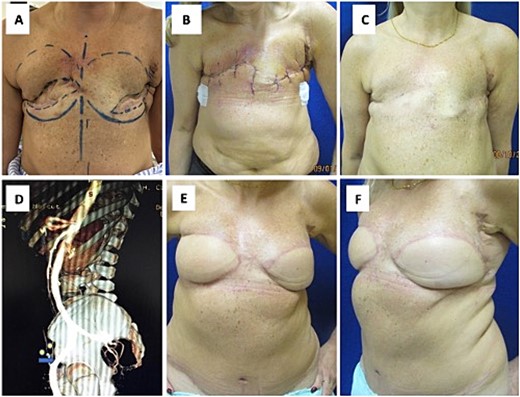
(A, B) Surgical debridement of the scars, (C) lipofilling in the chest wall (123 cc left, 125 cc right), (D) angiotomography confirming the ligation of the deep and superficial inferior epigastric vessels, and (E, F) surgical aspect three months after reconstruction with the TRAM flap.
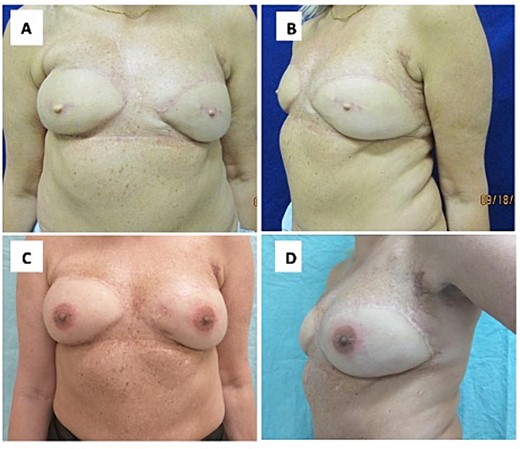
(A, B) Surgical aspect three months after lipofilling and nipple reconstruction. (C, D) Results after 3D tattooing of the nipple–areola complex.
Discussion
In recent years, there has been a noticeable increase in the frequency of immediate breast reconstruction following mastectomy. Breast reconstruction, which may include implants, tissue expanders, and autologous reconstruction, has been shown to have a significantly positive psychological impact on patients’ self-esteem, femininity, and sexuality without compromising the oncological outcome of breast cancer patients [3, 4]. However, as these reconstructive techniques are more widely used, potentially severe complications have also become more common [5].
In this article, we present the case of a patient who experienced extensive scar deformation on the chest after undergoing immediate breast reconstruction with implants. The initial procedure was complicated by a late surgical infection, causing implant failure. Szymankiewicz et al. [6] analysed 648 breasts reconstruction procedures using artificial implants and reported that 83% of implant failures were caused by infection, with 87% occurring within one year of implantation.
To address such a complex case, it was necessary to perform a sequence of procedures. Initially, we conducted bilateral laparoscopic ligation of the epigastric inferior arteries, which is a straightforward and safe procedure that can reduce the risk of partial or complete necrosis of muscle flaps, especially when large amounts of tissue are mobilized [5]. Then, we carried out a bilateral TRAM flap in combination with lipofilling. According to Visser et al. [8], autologous reconstruction after implant-based reconstruction is effective and has a low rate of complications. Finally, the final aesthetic result in this case was achieved through nipple-areola reconstruction via a 3D tattoo, resulting in a more natural appearance [7].
In conclusion, we demonstrated that even the most complex cases of scarring after initial complicated breast reconstruction can be successfully managed with a combination of different techniques. Lipofilling seems to be essential for remodeling the shape of the breast. In addition, 3-D tattooing of the areola and nipple should be considered a fundamental step in the whole process, clearly improving patient satisfaction and self-confidence.
Conflict of interest statement
None declared.
Funding
None declared.
References
Uhlmann NR, Martins MM, Piato S.
Visser NJ, Damen TH, Timman R, et al.



