-
PDF
- Split View
-
Views
-
Cite
Cite
Anthony M De Gregorio, K Robert Shen, Luis F Tapias, Diaphragmatic rupture due to massive gastric volvulus after robotic-assisted diaphragm plication, Journal of Surgical Case Reports, Volume 2024, Issue 9, September 2024, rjae546, https://doi.org/10.1093/jscr/rjae546
Close - Share Icon Share
Abstract
Gastric volvulus has been rarely associated with diaphragmatic paralysis or eventration. In this article, we present the case of a patient with idiopathic paralysis of the left hemidiaphragm that underwent treatment with a robotic thoracoscopic diaphragm plication, which was complicated by massive gastric volvulus resulting in such significant intra-abdominal hypertension that the ipsilateral diaphragm ruptured anterior to the plication suture line.
Introduction
Diaphragmatic eventration is an uncommon, permanent elevation of the hemidiaphragm with etiologies ranging from congenital defects due to poor migration of myoblasts to the septum transversum, to acquired including trauma, iatrogenic, infectious, or neurologic conditions resulting in dysfunction of the phrenic nerve [1]. However, many cases are idiopathic. Incidence is estimated at 0.05%, with a male predominance, and disproportionately affecting the left hemidiaphragm [1]. Clinical presentation includes respiratory symptoms, such as dyspnea on exertion or orthopnea, or gastrointestinal symptoms like epigastric pain, bloating, heartburn, dysphagia, or constipation. Depending on the severity of symptoms, management ranges from supportive to operative via diaphragmatic plication [1]. Gastric volvulus has been documented in association with eventration before and after diaphragm plication in case reports [2–5]. Gastric volvulus has also been documented in patients with chronic diaphragmatic eventration, with presentations suspicious for chronic volvulus before a major acute event, even resulting in gastric perforation [6]. Over time, a non-functional diaphragm becomes weak and thinned, theoretically increasing the risk of rupture [7]. Here, we present a scenario occurring within 48-h of surgery, where a patient developed acute massive gastric volvulus after diaphragmatic plication that likely resulted in intra-abdominal hypertension, ultimately leading to diaphragmatic rupture requiring reoperation.
Case report
This is a case of a 26-year-old male patient who presented with symptoms of dyspnea on exertion, left chest pressure, and constipation for 7 years. He was a never smoker with no history of trauma, nor prior neck and chest surgeries. Baseline pulmonary functions tests revealed FEV1 of 71% predicted and DLCO of 77% predicted. Work-up included a computed tomography (CT) of the chest which revealed marked left hemidiaphragm elevation with compression atelectasis of the left lower lobe (Fig. 1). A fluoroscopic sniff test showed paradoxical movement of the left hemidiaphragm consistent with diaphragmatic paralysis. Interestingly, abdominal imaging obtained 14 months before surgery showed a displaced stomach but without volvulus (Fig. 2). Due to the impact on the patient’s quality of life, he was offered surgical treatment with a robotic-assisted left thoracoscopic plication of the diaphragm. This was done using a three-arm technique using the Da Vinci Xi surgical system (Intuitive Surgical, Sunnyvale, CA) with an additional assistant port. Plication was performed by placing multiple horizontal mattresses sutures reinforced with pledgets in an anterior–posterior orientation, and systematically working medial to lateral. A postoperative chest X-ray showed a satisfactory result (Fig. 3).

Pre-operative imaging revealing marked left diaphragm eventration.

CT from 14-months pre-operation, demonstrating a full, but non-volvulized stomach.
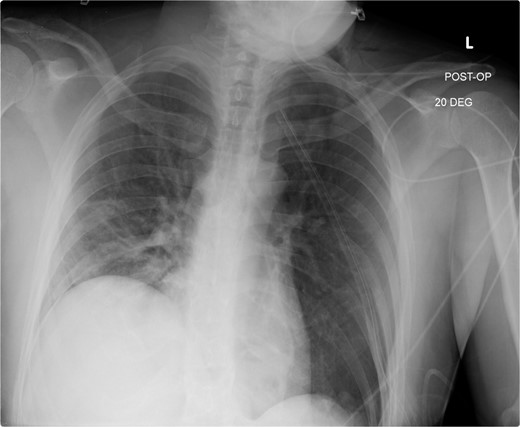
Immediate post-operative film demonstrates intact repair, and well-positioned chest-tube.
The early postoperative course was unremarkable. The patient reported feeling mild bloating, but was discharged on postoperative Day 1 after removal of a chest tube (Fig. 4). A few hours after discharge from the hospital, he developed dysphagia, progressive abdominal pain, distension, and dyspnea that prompted a return to the hospital. Physical examination revealed tachycardia (132 bpm), mild hypoxia requiring supplemental O2 at 2 L/min via nasal canula, and abdominal distension. Laboratory studies showed WBC of 12 600 cells/μL. A CT scan of the abdomen and pelvis revealed a large, acute organo-axial gastric volvulus without evidence of ischemia, and an intact left hemidiaphragm plication at a similar height to the right hemidiaphragm (Fig. 5). A nasogastric tube was placed with immediate drainage of 1 L of dark bilious fluid with immediate relief of the patient’s symptoms. However, a subsequent film revealed the nasogastric tube projecting toward the upper left chest with presence of colonic haustra (Fig. 6), consistent with acute hemidiaphragm rupture.
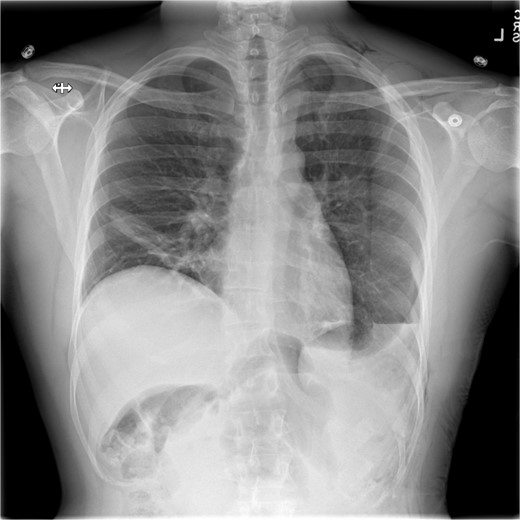
Following chest-tube removal, a film was taken, revealing even hemi-diaphragms, which was notably higher than immediate post-operatively, but within normal limits.

CT revealing intact diaphragm plication with massive organo-axial gastric volvulus.
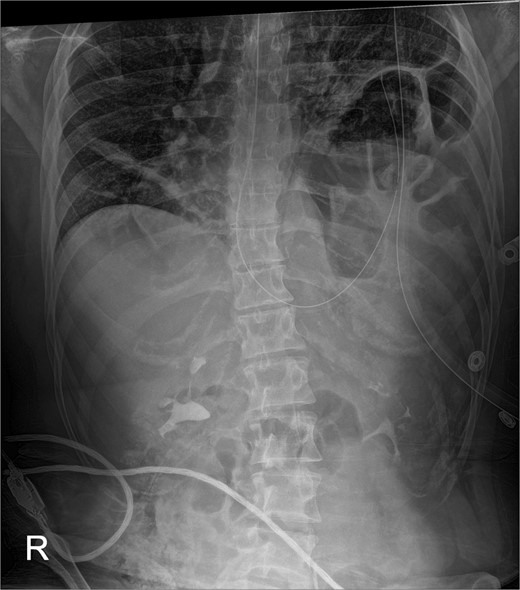
Confirmatory abdominal film for nasogastric tube placement demonstrating acute elevation in the left hemidiaphragm, 90-min after the CT, identifying the gastric volvulus.
He returned to the operating room where thoracoscopic exploration confirmed rupture of the left hemidiaphragm with herniation of the entire stomach, spleen, transverse and left colon. There was a small-volume hemothorax related to a superficial splenic capsular tear. Attempts for the reduction of herniated contents were unsuccessful thoracoscopically, thus we converted to thoracotomy. After a challenging reduction of herniated contents, a linear rupture defect anterior to the plication suture line was appreciated, extending medially from the level of entry of the left phrenic nerve to laterally 1–2 cm from the chest wall insertion. The defect was repaired with a 2 mm expanded polytetrafluoroethylene (ePTFE) patch (Gore-Tex; WL Gore & Associates, Flagstaff, Arizona) secured circumferentially with interrupted horizontal mattress sutures using 0-Ethibond sutures (Johnson and Johnson, Piscataway, NJ). This provided a robust and lower tension repair, all while keeping the diaphragm down avoiding compression on the left lung. Given the presentation with gastric volvulus, after closure of the thoracotomy, the patient was placed supine and exploratory laparoscopy was performed. This confirmed adequate orientation and position of the stomach. The patient recovered well and was discharged from the hospital on postoperative Day 5.
Discussion
Diaphragmatic plication has been proven to improve symptoms and quality of life in patients with diaphragmatic eventration/paralysis [8]. Here, we present a case of acute organo-axial gastric volvulus after robotic diaphragm plication resulting in diaphragmatic rupture. We have presented a clear timeline and imaging documentation that establishes a temporal relationship between the operation and this complication. Published case reports have described the association of gastric volvulus with diaphragm eventration (Table 1). Chronic elevation of the left hemidiaphragm might result in excessive laxity of the ligamentous attachments of the stomach that permits excess mobility after returning the stomach to a more anatomical position after plication, which can predispose to volvulus. The plicating sutures on the diaphragm could also change the position of parts of the stomach attached to the left hemidiaphragm, which can contribute to this phenomenon. Diaphragm eventration/paralysis results in thin tissue [2, 3, 7], which histologically can demonstrate fibroelastic changes with a paucity of muscle fibers [1]. Like the case presented here, a thin diaphragm has been reported in the setting of non-traumatic diaphragmatic rupture [7]. Diaphragmatic plication results in higher intra-abdominal pressure and tension across the plicated diaphragm which can further predispose to rupture in the setting of additional factors resulting in elevated intra-abdominal pressure, like gastric volvulus.
| . | Age . | Sex . | Pre-Volvulus Diaphragm Plication . | Eventration . | Complication . |
|---|---|---|---|---|---|
| 1[2] | 45 | M | No | Left | Organo-axial gastric volvulus |
| 2[4] | 16 | M | No | Left | Meso-axial gastric volvulus |
| 3[5] | 56 | M | No | Left | Organo-axial gastric volvulus |
| 4[6] | 13 | M | No | Bilateral | Perforated Organo-axial gastric volvulus |
| 5[7] | 5 | M | No | Left | Unknown axis gastric volvulus, Left diaphragm rupture |
| . | Age . | Sex . | Pre-Volvulus Diaphragm Plication . | Eventration . | Complication . |
|---|---|---|---|---|---|
| 1[2] | 45 | M | No | Left | Organo-axial gastric volvulus |
| 2[4] | 16 | M | No | Left | Meso-axial gastric volvulus |
| 3[5] | 56 | M | No | Left | Organo-axial gastric volvulus |
| 4[6] | 13 | M | No | Bilateral | Perforated Organo-axial gastric volvulus |
| 5[7] | 5 | M | No | Left | Unknown axis gastric volvulus, Left diaphragm rupture |
Events of gastric volvulus in the setting of diaphragm eventration, revealing cases of gastric volvulus have been seen to occur with predilection to the left, and occurring without preceding diaphragm plication.
| . | Age . | Sex . | Pre-Volvulus Diaphragm Plication . | Eventration . | Complication . |
|---|---|---|---|---|---|
| 1[2] | 45 | M | No | Left | Organo-axial gastric volvulus |
| 2[4] | 16 | M | No | Left | Meso-axial gastric volvulus |
| 3[5] | 56 | M | No | Left | Organo-axial gastric volvulus |
| 4[6] | 13 | M | No | Bilateral | Perforated Organo-axial gastric volvulus |
| 5[7] | 5 | M | No | Left | Unknown axis gastric volvulus, Left diaphragm rupture |
| . | Age . | Sex . | Pre-Volvulus Diaphragm Plication . | Eventration . | Complication . |
|---|---|---|---|---|---|
| 1[2] | 45 | M | No | Left | Organo-axial gastric volvulus |
| 2[4] | 16 | M | No | Left | Meso-axial gastric volvulus |
| 3[5] | 56 | M | No | Left | Organo-axial gastric volvulus |
| 4[6] | 13 | M | No | Bilateral | Perforated Organo-axial gastric volvulus |
| 5[7] | 5 | M | No | Left | Unknown axis gastric volvulus, Left diaphragm rupture |
Events of gastric volvulus in the setting of diaphragm eventration, revealing cases of gastric volvulus have been seen to occur with predilection to the left, and occurring without preceding diaphragm plication.
Conclusion
The true incidence and association of gastric volvulus and diaphragm eventration is unknown, particularly after plication. A high index of suspicion is needed when patients report upper gastrointestinal symptoms after plication of the diaphragm, particularly the left. Although rare, gastric volvulus should be part of the differential diagnosis.
Conflict of interest statement
None declared.
Funding
None declared.



