-
PDF
- Split View
-
Views
-
Cite
Cite
Jawaher Alrumayh, Meshal Albesher, Fayez Alrohaimi, Deep-seated intermuscular lipoma of posterior neck muscles: a case report and review of literature, Journal of Surgical Case Reports, Volume 2024, Issue 7, July 2024, rjae451, https://doi.org/10.1093/jscr/rjae451
Close - Share Icon Share
Abstract
Lipomas are the most common soft tissue tumours, accounting for nearly 50% of all soft tissue neoplasms. Among the types of lipomas, intermuscular lipomas are rare. We report the case of a 46-year-old man with a deep-seated lipoma located between the trapezius and splenius capitis muscles in the posterior neck triangle. A successful surgical excision was performed. This case highlights challenges in diagnosis, surgical management, and the importance of complete excision in minimizing the risk of recurrence. This type of lipoma remains relatively understudied; therefore, further studies are needed to increase awareness of its incidence, clinical presentation, diagnostic evaluation, and optimal management.
Introduction
Lipomas are benign tumours of mesenchymal origin and account for nearly 50% of soft tissue neoplasms [1]. However, their occurrence in the head and neck region has been observed in ~13% of cases [2]. Lipomas are either subcutaneous, located superficially to the enclosing fascia within the subcutaneous tissue, or deep-seated, located beneath the enclosing fascia [3]. Deep-seated lipomas may be located between muscles (intermuscular) or within muscles (intramuscular); both cases are rare, comprising only 0.3% and 1.8% of fatty tumours, respectively [4, 5]. In a study by Myhre-Jensen et al. [6], which examined 707 lipomas over 7 years, <1% were identified as deep-seated. Here, we report the case of a deep-seated lipoma located between the posterior neck muscles. This study aimed to improve the understanding and recognition of similar lesions for better outcomes in patients with deep-seated lipomas.
Case report
A 46-year-old man presented with a 1-month history of right-sided neck swelling following a fall. The patient did not experience any compression symptoms and denied any associated constitutional symptoms, such as fever, weight loss, decreased appetite, and night sweats. Furthermore, the patient had no family history of malignancies.
On physical examination, the patient had a body mass index of 28, and all vital signs were normal. Neck examination revealed a soft, non-fluctuant 3 × 3 cm mass in the posterior triangle under the trapezius muscle. The patient had no palpable cervical lymph nodes, no cranial neuropathy, normal flexible nasopharyngolaryngoscopy, and otherwise, unremarkable physical examination.
A contrast-enhanced computed tomography (CT) scan revealed a right posterior neck lipoma between the trapezius and splenius capitis muscles. No associated enhancing solid nodules or cervical lymphadenopathy were observed. The radiological findings were consistent with those of benign lipomas (Fig. 1).
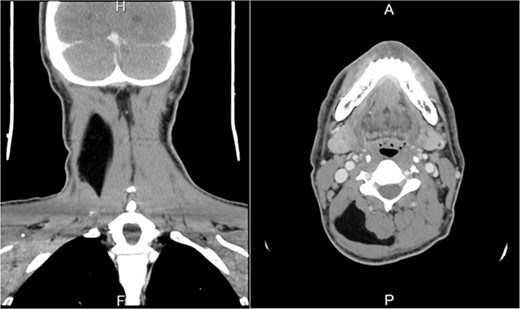
Preoperative contrast-enhanced CT image. (A) A coronal section shows a right hypodense mass between the trapezius and splenius capitis muscle. (B) Axial section shows a right hypodense mass between the trapezius and splenius capitis muscles.
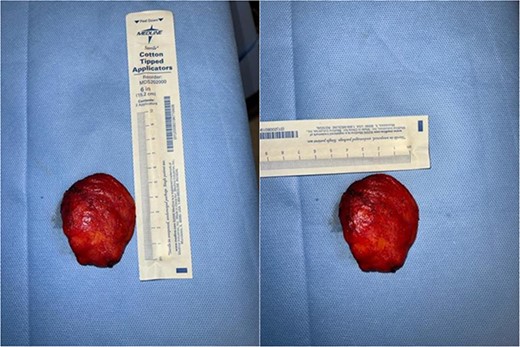
We counselled the patient about surgical options, and he agreed to participate. After obtaining written informed consent, the patient with a preliminary diagnosis of lipoma underwent surgery under general anaesthesia. After induction of general anaesthesia and intubation, the patient was placed in the lateral decubitus position for easier exposure. A 5-cm incision was made in the right posterior neck, and the skin flaps were dissected superiorly and inferiorly. The trapezius muscles were divided along the muscle fibres. The deep lipoma bed appeared to be on the scalene muscles, which were well dissected to completely remove the mass. The mass was completely excised en bloc (Fig. 2). The mass did not infiltrate the deep cervical muscles and exhibited a dissection plane. The dissected trapezius muscle edges were approximated, and the surgical wound was closed in layers. A surgical drain was not inserted. Postoperatively, the patient had an uneventful hospital stay with no adverse sequelae. The patient was discharged on the same day that the surgery was conducted. Histopathologically, the excised specimen comprised a 4.5 × 4.0 × 2.0-cm round-to-oval piece of fibrofatty tissue weighing 25 g. Histopathological examination confirmed mature fibro adipose tissue, consistent with a lipoma. The patient’s postoperative course was uneventful. Follow-ups at one and four weeks postoperatively showed good cosmetic results and no functional impairment.
Discussion
Lipomas are the most common benign soft tissue tumours. However, intermuscular lipomas are relatively rare and represent only a small proportion of fatty tumours [5, 7]. Their occurrence in the posterior neck region is extremely rare, with few published cases [2, 8–10]. Table 1 presents a comparative analysis of the reported cases, including patient demographics, symptoms, complications, and histopathological findings in intermuscular lipomas located within the posterior neck muscles. The clinical presentations of posterior neck lipomas vary, with some cases being asymptomatic, while others show concurrent symptoms, such as neck pain, limited range of motion, upper limb paraesthesia, and sleep difficulties [11, 12].
Literature review of deep-seated intermuscular lipomas in the posterior neck
| Author name/year . | Age . | Sex . | Location . | Size . | Complications . | Symptoms . | Histopathology . |
|---|---|---|---|---|---|---|---|
| Jung Sik Choi et al. (2015) | 49 | Man | Intermuscular space of the left neck, bordered by the splenius capitis, levator scapulae, and semispinalis muscles | 6 × 5 cm | None | Growing neck mass | Lipoma |
| Lee, K. S. et al. (2023) | 39 | Man | Intermuscular space of the left neck, bordered by the splenius capitis muscle, levator scapulae muscle, and semispinalis muscle. | 10.07 cm | None | Growing neck mass | Lipoma |
| Ferdinand Rico et al. (2019) | 30 | Woman | Substernocleidomastoid neck lipoma from C3 to the lung apex, abutting the carotid sheath and cervical thoracic duct. | 6.7 cm × 1.8 cm × 4.8 cm | None | Growing neck mass, dysphagia | Lipoma |
| Rattan, K. N. et al. (2021) | 3 | Man | Right posterior cervical region, deep to the sternocleidomastoid muscle, anteriorly abutting the parotid gland | 5.52 × 3.07 cm | None | Inability to fully turn the head | Fibrolipoma |
| Presented Case | 46 | Man | Between the trapezius and splenius capitis muscles in the posterior neck triangle | 4.5 × 4.0 × 2.0 cm | None | Growing neck mass | Fibrolipoma |
| Author name/year . | Age . | Sex . | Location . | Size . | Complications . | Symptoms . | Histopathology . |
|---|---|---|---|---|---|---|---|
| Jung Sik Choi et al. (2015) | 49 | Man | Intermuscular space of the left neck, bordered by the splenius capitis, levator scapulae, and semispinalis muscles | 6 × 5 cm | None | Growing neck mass | Lipoma |
| Lee, K. S. et al. (2023) | 39 | Man | Intermuscular space of the left neck, bordered by the splenius capitis muscle, levator scapulae muscle, and semispinalis muscle. | 10.07 cm | None | Growing neck mass | Lipoma |
| Ferdinand Rico et al. (2019) | 30 | Woman | Substernocleidomastoid neck lipoma from C3 to the lung apex, abutting the carotid sheath and cervical thoracic duct. | 6.7 cm × 1.8 cm × 4.8 cm | None | Growing neck mass, dysphagia | Lipoma |
| Rattan, K. N. et al. (2021) | 3 | Man | Right posterior cervical region, deep to the sternocleidomastoid muscle, anteriorly abutting the parotid gland | 5.52 × 3.07 cm | None | Inability to fully turn the head | Fibrolipoma |
| Presented Case | 46 | Man | Between the trapezius and splenius capitis muscles in the posterior neck triangle | 4.5 × 4.0 × 2.0 cm | None | Growing neck mass | Fibrolipoma |
Literature review of deep-seated intermuscular lipomas in the posterior neck
| Author name/year . | Age . | Sex . | Location . | Size . | Complications . | Symptoms . | Histopathology . |
|---|---|---|---|---|---|---|---|
| Jung Sik Choi et al. (2015) | 49 | Man | Intermuscular space of the left neck, bordered by the splenius capitis, levator scapulae, and semispinalis muscles | 6 × 5 cm | None | Growing neck mass | Lipoma |
| Lee, K. S. et al. (2023) | 39 | Man | Intermuscular space of the left neck, bordered by the splenius capitis muscle, levator scapulae muscle, and semispinalis muscle. | 10.07 cm | None | Growing neck mass | Lipoma |
| Ferdinand Rico et al. (2019) | 30 | Woman | Substernocleidomastoid neck lipoma from C3 to the lung apex, abutting the carotid sheath and cervical thoracic duct. | 6.7 cm × 1.8 cm × 4.8 cm | None | Growing neck mass, dysphagia | Lipoma |
| Rattan, K. N. et al. (2021) | 3 | Man | Right posterior cervical region, deep to the sternocleidomastoid muscle, anteriorly abutting the parotid gland | 5.52 × 3.07 cm | None | Inability to fully turn the head | Fibrolipoma |
| Presented Case | 46 | Man | Between the trapezius and splenius capitis muscles in the posterior neck triangle | 4.5 × 4.0 × 2.0 cm | None | Growing neck mass | Fibrolipoma |
| Author name/year . | Age . | Sex . | Location . | Size . | Complications . | Symptoms . | Histopathology . |
|---|---|---|---|---|---|---|---|
| Jung Sik Choi et al. (2015) | 49 | Man | Intermuscular space of the left neck, bordered by the splenius capitis, levator scapulae, and semispinalis muscles | 6 × 5 cm | None | Growing neck mass | Lipoma |
| Lee, K. S. et al. (2023) | 39 | Man | Intermuscular space of the left neck, bordered by the splenius capitis muscle, levator scapulae muscle, and semispinalis muscle. | 10.07 cm | None | Growing neck mass | Lipoma |
| Ferdinand Rico et al. (2019) | 30 | Woman | Substernocleidomastoid neck lipoma from C3 to the lung apex, abutting the carotid sheath and cervical thoracic duct. | 6.7 cm × 1.8 cm × 4.8 cm | None | Growing neck mass, dysphagia | Lipoma |
| Rattan, K. N. et al. (2021) | 3 | Man | Right posterior cervical region, deep to the sternocleidomastoid muscle, anteriorly abutting the parotid gland | 5.52 × 3.07 cm | None | Inability to fully turn the head | Fibrolipoma |
| Presented Case | 46 | Man | Between the trapezius and splenius capitis muscles in the posterior neck triangle | 4.5 × 4.0 × 2.0 cm | None | Growing neck mass | Fibrolipoma |
Lipomas are commonly diagnosed based on characteristic clinical and radiological features, with ultrasonography often serving as the initial diagnostic modality for suspected head and neck lipomas [13, 14]. Lipomas typically present as hyperechoic elliptical masses with linear echogenic lines on ultrasonography. Notably, they may appear isoechoic or hypoechoic, making them less distinctive than more advanced imaging modalities [13]. In the case report of a substernocleidomastoid muscle lipoma, ultrasonography was used as the primary imaging modality, revealing a circumscribed solid echogenic mass that was subsequently identified as a lipoma [10]. CT scans are more accurate for the diagnosis of lipomas, as they demonstrate the size, location, and extent of infiltration into surrounding tissues [15]. Benign lipomas appear as hypoattenuated, homogeneous masses without contrast enhancement [16]. In the present case, the CT findings were consistent with a benign lipoma located between the trapezius and splenius capitis muscles. The absence of infiltrative growth or increased density supported the diagnosis of benign lipomas. However, CT may not detect microscopic infiltration or early malignant transformation, contributing to recurrence [17].
Surgical excision is generally used to treat lipomas [18]. Complete excision is crucial to prevent residual diseases, leading to recurrence, and the need for additional surgical interventions with increased risks and complications [19]. Studies have shown that intermuscular lipomas have lower recurrence rates than intramuscular lipomas, with most recurrences observed in infiltrative lipomas [5].
Follow-ups are important for monitoring any signs of recurrence or complications. Our patient had regular follow-ups at 1 and 4 weeks postoperatively, and these visits showed good cosmetic results and no functional impairment.
Conclusion
Head and neck deep-seated lipomas present unique challenges. This case report contributes to the limited literature on posterior neck intermuscular lipoma. Further research and documentation of such cases are necessary to enhance the understanding of their incidence, clinical presentation, diagnostic evaluation, and optimal management strategies.
Acknowledgements
The authors would like to thank Editage (www.editage.com) for English language editing.
Conflict of interest statement
None declared.
Funding
None declared.



