-
PDF
- Split View
-
Views
-
Cite
Cite
Mahmoud M Taha, Mohamed M Arnaout, Ahmad Alkheder, Khaled Abdel Aziz Jr, Mazen M Taha, Khaled Alsayed Abualkhair, Rare dorsal ossified meningioma in an elderly female: a case report and comprehensive review of literature, Journal of Surgical Case Reports, Volume 2024, Issue 6, June 2024, rjae389, https://doi.org/10.1093/jscr/rjae389
Close - Share Icon Share
Abstract
Meningiomas, typically benign neoplasms originating in the central nervous system, display a predilection for female patients. Although they predominantly manifest within the cranial vault, ~25% of primary spinal neoplasms are attributed to these tumors. The occurrence of ossification in spinal meningiomas is an uncommon phenomenon, with scant documentation in medical literature. In this report, we detail the clinical journey of an octogenarian female patient afflicted with an ossified spinal meningioma, which was associated with left lower extremity weakness and reduced sensation. Diagnostic imaging, specifically magnetic resonance imaging, identified a mass exerting pressure on the spinal cord, necessitating its surgical removal. Subsequent histopathological examinations corroborated the initial diagnosis. Postoperative magnetic resonance imaging scans confirmed the absence of residual tumor tissue and ruled out recurrence. A comprehensive review of existing literature yielded 47 analogous cases, with a majority involving elderly female patients and the thoracic region of the spine being the most common site. The standard therapeutic approach is surgical intervention, which is often complicated by the tumor’s tenacious adherence to surrounding structures and the potential for ensuing operative complications. This case highlights the exceptional nature of ossified spinal meningiomas and emphasizes the critical need for meticulous surgical management.
Introduction
Meningiomas stand as the most prevalent primary benign tumors within the central nervous system. They typically manifest as benign growths and exhibit a prevalence twice as high in females compared to males. Factors contributing to their occurrence encompass ethnicity, familial predisposition, and prior exposure to radiation [1, 2]. Although meningiomas predominantly arise intracranially, they can also manifest within the spinal cord. Spinal meningiomas constitute ~25% of primary spinal tumors [2]. Ossification within spinal meningiomas is an infrequent occurrence, with only 46 reported cases preceding the one detailed in this case report. Herein, we present a case of ossified spinal meningioma in an 80-year-old female.
Case presentation
An otherwise healthy 80-year-old female patient presented with left lower extremity weakness following frequent falls ~1 month ago. Upon examination, motor power in the left lower limb was graded as III, accompanied by hypoesthesia. Without any other accompanying symptoms, magnetic resonance imaging (MRI) of the spine revealed a lesion within the vertebral canal causing compression of the spinal cord at the D10–D11 level (Fig. 1). T1-weighted images (T1WI) displayed hypointense calcified regions

Preoperative MRI, sagittal view, T2WI, shows tumor mass at levels D10–D11.
within the lesion, while T2-weighted images (T2WI) exhibited variable signal intensity, predominantly hypointense, in addition to surrounding tissue changes indicative of compression and edema (Fig. 2). Subsequently, the patient underwent surgical excision of the lesion, including laminectomy of D10–D11. A sharp dissection of the mass from the dura was performed during the surgery (Fig. 3). Two months after surgery, the patient underwent a short course of physiotherapy for several weeks, and now they can ambulate without support. The postoperative period was uneventful. Histopathological analysis revealed the presence of classical psammoma bodies, characterized by calcium deposits or punctate calcifications within the tumor mass, consistent with a diagnosis of classic meningioma ossified (Fig. 4). A follow-up MRI performed after 3 months demonstrated complete excision with no evidence of tumor recurrence (Fig. 5).

Preoperative MRI, axial view, T2WI, shows of hypointensely calcified regions within the tumor.
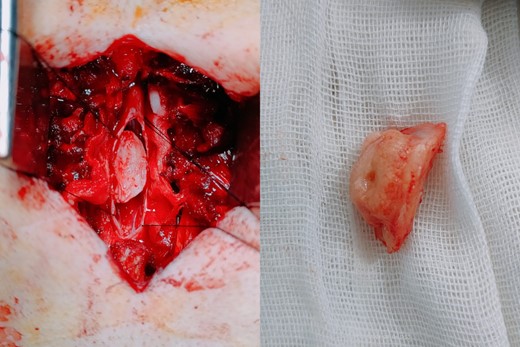
Intraoperative images showing the tumor after dissection and after complete excision.
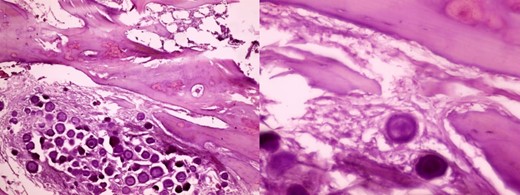
Histopathology shows the classical psammoma bodies, which are composed of calcium deposits or punctate calcifications within the tumor mass.

Postoperative MRI, sagittal view, T2WI, showing complete resection of the tumor.
Discussion
Spinal meningioma exhibits various classifications, comprising up to 15 histologic subtypes, with the psammomatous, meningothelial, and transitional types being the most prevalent. Ossification of spinal meningioma is a relatively uncommon occurrence, reported in 5%–10% of cases [3].
Based on our comprehensive review of the existing literature, our investigation identified 47 cases of ossified spinal meningioma, which includes the case detailed in this report (Table 1). Our analysis revealed a predominance of occurrences in females (42 cases) compared to males (5 cases). The average age of patients afflicted with ossified spinal meningioma was 64.6 years, with ages ranging from 15 to 90 years. The thoracic spine was the most common site of manifestation, accounting for 89.3% (42 cases) of cases, followed by the cervical spine (4 cases, 9%) and lumbar spine (1 case, 1.7%). Treatment modalities primarily involved gross total resection in 42 cases, subtotal resection in 3 cases, and insufficiently described resection extents in 2 cases. Postoperatively, the majority of patients demonstrated gradual improvement, with 25 cases showing no recurrence, although recurrence status was not reported for the remainder of the cases (Table 1).
| Study (Year) . | Age/ Gender . | . | Tumor number . | Ossified . | Level . | Location . | Symptoms . | Treatment . | Clinical outcomes . | Recurrence . | Histological characteristics . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Roger et al., 1928 [5] | 16/F | 1 | Ossified | T9 | Lateral | Myelopathy | GTR | Improved (3 months) | No | Psammoma bodies, bone cells | |
| Freidberg et al., 1972 [6] | 69/F | 1 | Ossified | T1–2 | Ventral | Myelopathy | GTR + dura | Improved (6 weeks) | NA | Psammoma bodies, mature cancellous bone | |
| Kandel et al., 1989 [7] | 17/F | 1 | Ossified | T8 | Dorsal | Myelopathy | GTR | NA | No | Meningotheliomatous, psammoma bodies, bone spicule | |
| Niijima et al., 1993 [8] | 75/F | 1 | Ossified | T8–9 | Dorsolateral | Myelopathy | GTR + dura | Improved (14 months) | NA | Psammoma bodies, bone spicule | |
| Kitagawa et al., 1994 [9] | 75/F | 1 | Ossified | T9–10 | NA | Myelopathy | NA | NA | NA | Psammoma bodies, bone tissue | |
| 60/F | 1 | Ossified | T6–8 | NA | Myelopathy | NA | NA | NA | Psammoma bodies, bone tissue | ||
| Nakayama et al., 1996 [10] | 74/F | 1 | Ossified | T9 | Dorsal | Myelopathy | GTR | NA | NA | Matured lamellar bone tissue | |
| 45/M | 1 | Ossified | C1–3 | Ventral | Myelopathy | GTR | NA | NA | Matured bone tissue | ||
| Huang et al., 1999 [11] | 73/F | 1 | Ossified | T5 | Lateral | Myelopathy | GTR | Improved | NA | Psammoma bodies, bone marrow | |
| Saito et al., 2001 [12] | 54/F | 1 | Ossified | T11 | Dorsal | NA | GTR + dura | Improved | No | Metaplastic (osseous) | |
| Naderi et al., 2001 [13] | 15/M | 1 | Ossified | T4 | Dorsal | Myelopathy | GTR + dura | Improved (3 months) | NA | Psammoma bodies, mature bone tissue | |
| Liu et al., 2006 [14] | 70/F | 1 | Ossified | T11 | Dorsolateral | Myelopathy | GTR | Improved (2 years) | No | Psammoma bodies, woven bone | |
| Hirabayashi et al., 2009 [15] | 82/F | 1 | Partially ossified | L3 | Dorsolateral | Cauda equina syndrome | GTR | Improved | No (5 years) | Osseous | |
| Tahir et al., 2009 [16] | 40/F | 1 | Partially ossified | T6 | Dorsolateral | Myelopathy | GTR | Improved (8 months) | No | Mineralized bone | |
| Uchida et al., 2009 [17] | 40/F | 2 | Ossified | T8 and T12 | Dorsal, dorsolateral | Myelopathy | GTR + dura | Improved | No (2 years) | Psammoma bodies, mature bone | |
| Licci et al., 2010 [18] | 58/F | 1 | Ossified | T6 | Dorsal | Myelopathy | GTR | Improved (1 year) | NA | Psammoma bodies, lamellar bone tissue, hematopoiesis | |
| Chotai et al., 2013 [19] | 61/F | 1 | Ossified | T4–5 | Dorsal | Myelopathy | GTR + dura | Improved (1 month) | NA | Psammoma bodies, mature lamellar bone, hematopoiesis | |
| Study (Year) | Age/Gender | Tumor number | Ossified | Level | Location | Symptoms | Treatment | Clinical outcomes | Recurrence | Histological characteristics | |
| Ju et al., 2013 [20] | 61/F | 1 | Ossified | T9–10 | Lateral | Myelopathy | GTR + dura | Improved (1 month) | NA | Heterotopic ossification | |
| Taneoka et al., 2013 [21] | 78/F | 1 | Ossified | T9 | Dorsal | Myelopathy | GTR + dura | Improved | NA | Psammoma bodies, mature bone, hematopoiesis | |
| Yamane et al., 2014 [22] | 61/F | 1 | Ossified | T12 | Ventrolateral | Myelopathy | GTR | Improved | No (2 years) | Psammoma bodies, cancellous bone with bone marrow | |
| Chan et al., 2014 [23] | 64/F | 1 | Ossified | T9–10 | Dorsal | Myelopathy | GTR | Improved (6 month) | NA | Psammoma bodies, bone marrow, hematopoiesis | |
| Alafaci et al., 2015 [24] | 45/M | 1 | Ossified | T2–3 | Ventral 4, lateral 1, dorsal 4 | Myelopathy | GTR | Improved | No | Seven cases of osseous component in association with psammoma bodies, two cases of immature bone trabeculae | |
| 75/F | 1 | Ossified | T3–4 | Myelopathy | GTR | Improved | No | ||||
| 86/F | 1 | Ossified | T3–4 | Myelopathy | GTR | Improved | No | ||||
| 65/F | 1 | Ossified | T7 | Myelopathy | GTR | Improved | No | ||||
| 72/F | 1 | Ossified | C7 | Myelopathy | STR | Improved | No | ||||
| 40/F | 1 | Ossified | T1–2 | Myelopathy | STR | Improved | No | ||||
| 65/F | 1 | Ossified | T7–8 | Myelopathy | GTR | Improved | No | ||||
| 40/F | 1 | Ossified | C7 | Myelopathy | GTR | Improved | No | ||||
| 41/F | 1 | Ossified | T2–3 | Myelopathy | GTR | Improved | No | ||||
| Kim et al., 2016 [28] | 51/F | 1 | Ossified | T4 | Dorsal | Myelopathy | GTR | Improved | No | Psammoma bodies | |
| 77/F | 1 | Ossified | T9 | Dorsal | Myelopathy | GTR | Improved | No | Psammoma bodies | ||
| Demir et al., 2016 [25] | 26/F | 1 | Ossified- calcified | T9–11 | Dorsal | Myelopathy | GTR | NA | NA | Psammoma bodies | |
| Cochran et al., 2016 [26] | 47/F | 1 | Ossified | T8 | Ventral | Radiculopathy | GTR | Improved | No (22 months) | Psammoma bodies, bone marrow, hematopoiesis | |
| Xia and Tian, 2016 [27] | 90/M | 1 | Ossified | T10–11 | Dorsal | Spinal cord injury after fall | GTR | NA | NA | Psammoma bodies, bone trabeculae | |
| Prakash et al., 2018 [29] | 60/F | 1 | Ossified | T7–8 | Dorsolateral | Myelopathy | GTR | Improved (6 month) | NA | Psammoma bodies, immature bony trabeculae | |
| Sakamoto et al., 2018 [38] | 57/F | 1 | Ossified | C7 | Ventrolaterodorsal | Myelopathy | STR | Improved | NA | Osseous core, fibrous | |
| Murakami et al., 2019 [4] | 29/F | 1 | Ossified | T12 | Lateral | Back pain, leg numbness | GTR + dura | Unchanged (12 months) | NA | Psammoma bodies, mature bone tissue | |
| Taha et al., 2019 [30] | 22/F | 1 | Ossified | T4–5 | Dorsal | Myelopathy | GTR | Improved (6 month) | NA | Psammoma bodies, bone trabeculae | |
| Wang et al., 2019 [31] | 52/F | 1 | Ossified | T4 | Dorsal | Back pain | GTR | Improved | No (2.5 years) | Psammoma bodies, immature trabecular bone, hematopoiesis | |
| Xu et al., 2020 [32] | 85/F | 1 | Ossified | T11 | Lateral | Back pain, leg pain | GTR + dura | Improved | No (1 year) | Psammoma bodies | |
| Buchanan et al., 2021 [33] | 64/M | 1 | Ossified | T4 | Dorsal | Myelopathy | GTR + dura | Improved (6 month) | NA | Psammoma bodies, bone formation, osseous metaplasia | |
| Wong et al., 2021 [34] | 75/F | 1 | Ossified | T10- T11 | NA | Myelopathy | GTR + dura | Not improved (6 months) | NA | Psammoma bodies, immature trabeculae bone | |
| Thakur et al., 2021 [35] | 74/F | 1 | Ossified | T8 | Ventrolateral | Tingling paresthesia | GTR + dura | Improved | NA | Psammoma bodies, bony hard-tissue fragments | |
| Dong et al., 2022 [36] | 76/F | 5 | Ossified | T7–12 | Dorsal | Myelopathy | GTR + dura | Improved | No | Psammoma bodies, trabecular bone, hematopoiesis | |
| Xu et al., 2023 [39] | 68/F | 1 | Ossified | T10 | Dorsal | Paresthesia, gait disturbance | GTR | Improved | No | meningioma with diffused psammomatous bodies | |
| Taha et al., 2024 (present) | 80/F | 1 | Ossified,calcified | T10–11 | Dorsal | Lower limb weakness | GTR | Improved | No | classical psammoma bodies, characterized by calcium deposits |
| Study (Year) . | Age/ Gender . | . | Tumor number . | Ossified . | Level . | Location . | Symptoms . | Treatment . | Clinical outcomes . | Recurrence . | Histological characteristics . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Roger et al., 1928 [5] | 16/F | 1 | Ossified | T9 | Lateral | Myelopathy | GTR | Improved (3 months) | No | Psammoma bodies, bone cells | |
| Freidberg et al., 1972 [6] | 69/F | 1 | Ossified | T1–2 | Ventral | Myelopathy | GTR + dura | Improved (6 weeks) | NA | Psammoma bodies, mature cancellous bone | |
| Kandel et al., 1989 [7] | 17/F | 1 | Ossified | T8 | Dorsal | Myelopathy | GTR | NA | No | Meningotheliomatous, psammoma bodies, bone spicule | |
| Niijima et al., 1993 [8] | 75/F | 1 | Ossified | T8–9 | Dorsolateral | Myelopathy | GTR + dura | Improved (14 months) | NA | Psammoma bodies, bone spicule | |
| Kitagawa et al., 1994 [9] | 75/F | 1 | Ossified | T9–10 | NA | Myelopathy | NA | NA | NA | Psammoma bodies, bone tissue | |
| 60/F | 1 | Ossified | T6–8 | NA | Myelopathy | NA | NA | NA | Psammoma bodies, bone tissue | ||
| Nakayama et al., 1996 [10] | 74/F | 1 | Ossified | T9 | Dorsal | Myelopathy | GTR | NA | NA | Matured lamellar bone tissue | |
| 45/M | 1 | Ossified | C1–3 | Ventral | Myelopathy | GTR | NA | NA | Matured bone tissue | ||
| Huang et al., 1999 [11] | 73/F | 1 | Ossified | T5 | Lateral | Myelopathy | GTR | Improved | NA | Psammoma bodies, bone marrow | |
| Saito et al., 2001 [12] | 54/F | 1 | Ossified | T11 | Dorsal | NA | GTR + dura | Improved | No | Metaplastic (osseous) | |
| Naderi et al., 2001 [13] | 15/M | 1 | Ossified | T4 | Dorsal | Myelopathy | GTR + dura | Improved (3 months) | NA | Psammoma bodies, mature bone tissue | |
| Liu et al., 2006 [14] | 70/F | 1 | Ossified | T11 | Dorsolateral | Myelopathy | GTR | Improved (2 years) | No | Psammoma bodies, woven bone | |
| Hirabayashi et al., 2009 [15] | 82/F | 1 | Partially ossified | L3 | Dorsolateral | Cauda equina syndrome | GTR | Improved | No (5 years) | Osseous | |
| Tahir et al., 2009 [16] | 40/F | 1 | Partially ossified | T6 | Dorsolateral | Myelopathy | GTR | Improved (8 months) | No | Mineralized bone | |
| Uchida et al., 2009 [17] | 40/F | 2 | Ossified | T8 and T12 | Dorsal, dorsolateral | Myelopathy | GTR + dura | Improved | No (2 years) | Psammoma bodies, mature bone | |
| Licci et al., 2010 [18] | 58/F | 1 | Ossified | T6 | Dorsal | Myelopathy | GTR | Improved (1 year) | NA | Psammoma bodies, lamellar bone tissue, hematopoiesis | |
| Chotai et al., 2013 [19] | 61/F | 1 | Ossified | T4–5 | Dorsal | Myelopathy | GTR + dura | Improved (1 month) | NA | Psammoma bodies, mature lamellar bone, hematopoiesis | |
| Study (Year) | Age/Gender | Tumor number | Ossified | Level | Location | Symptoms | Treatment | Clinical outcomes | Recurrence | Histological characteristics | |
| Ju et al., 2013 [20] | 61/F | 1 | Ossified | T9–10 | Lateral | Myelopathy | GTR + dura | Improved (1 month) | NA | Heterotopic ossification | |
| Taneoka et al., 2013 [21] | 78/F | 1 | Ossified | T9 | Dorsal | Myelopathy | GTR + dura | Improved | NA | Psammoma bodies, mature bone, hematopoiesis | |
| Yamane et al., 2014 [22] | 61/F | 1 | Ossified | T12 | Ventrolateral | Myelopathy | GTR | Improved | No (2 years) | Psammoma bodies, cancellous bone with bone marrow | |
| Chan et al., 2014 [23] | 64/F | 1 | Ossified | T9–10 | Dorsal | Myelopathy | GTR | Improved (6 month) | NA | Psammoma bodies, bone marrow, hematopoiesis | |
| Alafaci et al., 2015 [24] | 45/M | 1 | Ossified | T2–3 | Ventral 4, lateral 1, dorsal 4 | Myelopathy | GTR | Improved | No | Seven cases of osseous component in association with psammoma bodies, two cases of immature bone trabeculae | |
| 75/F | 1 | Ossified | T3–4 | Myelopathy | GTR | Improved | No | ||||
| 86/F | 1 | Ossified | T3–4 | Myelopathy | GTR | Improved | No | ||||
| 65/F | 1 | Ossified | T7 | Myelopathy | GTR | Improved | No | ||||
| 72/F | 1 | Ossified | C7 | Myelopathy | STR | Improved | No | ||||
| 40/F | 1 | Ossified | T1–2 | Myelopathy | STR | Improved | No | ||||
| 65/F | 1 | Ossified | T7–8 | Myelopathy | GTR | Improved | No | ||||
| 40/F | 1 | Ossified | C7 | Myelopathy | GTR | Improved | No | ||||
| 41/F | 1 | Ossified | T2–3 | Myelopathy | GTR | Improved | No | ||||
| Kim et al., 2016 [28] | 51/F | 1 | Ossified | T4 | Dorsal | Myelopathy | GTR | Improved | No | Psammoma bodies | |
| 77/F | 1 | Ossified | T9 | Dorsal | Myelopathy | GTR | Improved | No | Psammoma bodies | ||
| Demir et al., 2016 [25] | 26/F | 1 | Ossified- calcified | T9–11 | Dorsal | Myelopathy | GTR | NA | NA | Psammoma bodies | |
| Cochran et al., 2016 [26] | 47/F | 1 | Ossified | T8 | Ventral | Radiculopathy | GTR | Improved | No (22 months) | Psammoma bodies, bone marrow, hematopoiesis | |
| Xia and Tian, 2016 [27] | 90/M | 1 | Ossified | T10–11 | Dorsal | Spinal cord injury after fall | GTR | NA | NA | Psammoma bodies, bone trabeculae | |
| Prakash et al., 2018 [29] | 60/F | 1 | Ossified | T7–8 | Dorsolateral | Myelopathy | GTR | Improved (6 month) | NA | Psammoma bodies, immature bony trabeculae | |
| Sakamoto et al., 2018 [38] | 57/F | 1 | Ossified | C7 | Ventrolaterodorsal | Myelopathy | STR | Improved | NA | Osseous core, fibrous | |
| Murakami et al., 2019 [4] | 29/F | 1 | Ossified | T12 | Lateral | Back pain, leg numbness | GTR + dura | Unchanged (12 months) | NA | Psammoma bodies, mature bone tissue | |
| Taha et al., 2019 [30] | 22/F | 1 | Ossified | T4–5 | Dorsal | Myelopathy | GTR | Improved (6 month) | NA | Psammoma bodies, bone trabeculae | |
| Wang et al., 2019 [31] | 52/F | 1 | Ossified | T4 | Dorsal | Back pain | GTR | Improved | No (2.5 years) | Psammoma bodies, immature trabecular bone, hematopoiesis | |
| Xu et al., 2020 [32] | 85/F | 1 | Ossified | T11 | Lateral | Back pain, leg pain | GTR + dura | Improved | No (1 year) | Psammoma bodies | |
| Buchanan et al., 2021 [33] | 64/M | 1 | Ossified | T4 | Dorsal | Myelopathy | GTR + dura | Improved (6 month) | NA | Psammoma bodies, bone formation, osseous metaplasia | |
| Wong et al., 2021 [34] | 75/F | 1 | Ossified | T10- T11 | NA | Myelopathy | GTR + dura | Not improved (6 months) | NA | Psammoma bodies, immature trabeculae bone | |
| Thakur et al., 2021 [35] | 74/F | 1 | Ossified | T8 | Ventrolateral | Tingling paresthesia | GTR + dura | Improved | NA | Psammoma bodies, bony hard-tissue fragments | |
| Dong et al., 2022 [36] | 76/F | 5 | Ossified | T7–12 | Dorsal | Myelopathy | GTR + dura | Improved | No | Psammoma bodies, trabecular bone, hematopoiesis | |
| Xu et al., 2023 [39] | 68/F | 1 | Ossified | T10 | Dorsal | Paresthesia, gait disturbance | GTR | Improved | No | meningioma with diffused psammomatous bodies | |
| Taha et al., 2024 (present) | 80/F | 1 | Ossified,calcified | T10–11 | Dorsal | Lower limb weakness | GTR | Improved | No | classical psammoma bodies, characterized by calcium deposits |
GTR, gross total resection; STR, subtotal resection.
| Study (Year) . | Age/ Gender . | . | Tumor number . | Ossified . | Level . | Location . | Symptoms . | Treatment . | Clinical outcomes . | Recurrence . | Histological characteristics . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Roger et al., 1928 [5] | 16/F | 1 | Ossified | T9 | Lateral | Myelopathy | GTR | Improved (3 months) | No | Psammoma bodies, bone cells | |
| Freidberg et al., 1972 [6] | 69/F | 1 | Ossified | T1–2 | Ventral | Myelopathy | GTR + dura | Improved (6 weeks) | NA | Psammoma bodies, mature cancellous bone | |
| Kandel et al., 1989 [7] | 17/F | 1 | Ossified | T8 | Dorsal | Myelopathy | GTR | NA | No | Meningotheliomatous, psammoma bodies, bone spicule | |
| Niijima et al., 1993 [8] | 75/F | 1 | Ossified | T8–9 | Dorsolateral | Myelopathy | GTR + dura | Improved (14 months) | NA | Psammoma bodies, bone spicule | |
| Kitagawa et al., 1994 [9] | 75/F | 1 | Ossified | T9–10 | NA | Myelopathy | NA | NA | NA | Psammoma bodies, bone tissue | |
| 60/F | 1 | Ossified | T6–8 | NA | Myelopathy | NA | NA | NA | Psammoma bodies, bone tissue | ||
| Nakayama et al., 1996 [10] | 74/F | 1 | Ossified | T9 | Dorsal | Myelopathy | GTR | NA | NA | Matured lamellar bone tissue | |
| 45/M | 1 | Ossified | C1–3 | Ventral | Myelopathy | GTR | NA | NA | Matured bone tissue | ||
| Huang et al., 1999 [11] | 73/F | 1 | Ossified | T5 | Lateral | Myelopathy | GTR | Improved | NA | Psammoma bodies, bone marrow | |
| Saito et al., 2001 [12] | 54/F | 1 | Ossified | T11 | Dorsal | NA | GTR + dura | Improved | No | Metaplastic (osseous) | |
| Naderi et al., 2001 [13] | 15/M | 1 | Ossified | T4 | Dorsal | Myelopathy | GTR + dura | Improved (3 months) | NA | Psammoma bodies, mature bone tissue | |
| Liu et al., 2006 [14] | 70/F | 1 | Ossified | T11 | Dorsolateral | Myelopathy | GTR | Improved (2 years) | No | Psammoma bodies, woven bone | |
| Hirabayashi et al., 2009 [15] | 82/F | 1 | Partially ossified | L3 | Dorsolateral | Cauda equina syndrome | GTR | Improved | No (5 years) | Osseous | |
| Tahir et al., 2009 [16] | 40/F | 1 | Partially ossified | T6 | Dorsolateral | Myelopathy | GTR | Improved (8 months) | No | Mineralized bone | |
| Uchida et al., 2009 [17] | 40/F | 2 | Ossified | T8 and T12 | Dorsal, dorsolateral | Myelopathy | GTR + dura | Improved | No (2 years) | Psammoma bodies, mature bone | |
| Licci et al., 2010 [18] | 58/F | 1 | Ossified | T6 | Dorsal | Myelopathy | GTR | Improved (1 year) | NA | Psammoma bodies, lamellar bone tissue, hematopoiesis | |
| Chotai et al., 2013 [19] | 61/F | 1 | Ossified | T4–5 | Dorsal | Myelopathy | GTR + dura | Improved (1 month) | NA | Psammoma bodies, mature lamellar bone, hematopoiesis | |
| Study (Year) | Age/Gender | Tumor number | Ossified | Level | Location | Symptoms | Treatment | Clinical outcomes | Recurrence | Histological characteristics | |
| Ju et al., 2013 [20] | 61/F | 1 | Ossified | T9–10 | Lateral | Myelopathy | GTR + dura | Improved (1 month) | NA | Heterotopic ossification | |
| Taneoka et al., 2013 [21] | 78/F | 1 | Ossified | T9 | Dorsal | Myelopathy | GTR + dura | Improved | NA | Psammoma bodies, mature bone, hematopoiesis | |
| Yamane et al., 2014 [22] | 61/F | 1 | Ossified | T12 | Ventrolateral | Myelopathy | GTR | Improved | No (2 years) | Psammoma bodies, cancellous bone with bone marrow | |
| Chan et al., 2014 [23] | 64/F | 1 | Ossified | T9–10 | Dorsal | Myelopathy | GTR | Improved (6 month) | NA | Psammoma bodies, bone marrow, hematopoiesis | |
| Alafaci et al., 2015 [24] | 45/M | 1 | Ossified | T2–3 | Ventral 4, lateral 1, dorsal 4 | Myelopathy | GTR | Improved | No | Seven cases of osseous component in association with psammoma bodies, two cases of immature bone trabeculae | |
| 75/F | 1 | Ossified | T3–4 | Myelopathy | GTR | Improved | No | ||||
| 86/F | 1 | Ossified | T3–4 | Myelopathy | GTR | Improved | No | ||||
| 65/F | 1 | Ossified | T7 | Myelopathy | GTR | Improved | No | ||||
| 72/F | 1 | Ossified | C7 | Myelopathy | STR | Improved | No | ||||
| 40/F | 1 | Ossified | T1–2 | Myelopathy | STR | Improved | No | ||||
| 65/F | 1 | Ossified | T7–8 | Myelopathy | GTR | Improved | No | ||||
| 40/F | 1 | Ossified | C7 | Myelopathy | GTR | Improved | No | ||||
| 41/F | 1 | Ossified | T2–3 | Myelopathy | GTR | Improved | No | ||||
| Kim et al., 2016 [28] | 51/F | 1 | Ossified | T4 | Dorsal | Myelopathy | GTR | Improved | No | Psammoma bodies | |
| 77/F | 1 | Ossified | T9 | Dorsal | Myelopathy | GTR | Improved | No | Psammoma bodies | ||
| Demir et al., 2016 [25] | 26/F | 1 | Ossified- calcified | T9–11 | Dorsal | Myelopathy | GTR | NA | NA | Psammoma bodies | |
| Cochran et al., 2016 [26] | 47/F | 1 | Ossified | T8 | Ventral | Radiculopathy | GTR | Improved | No (22 months) | Psammoma bodies, bone marrow, hematopoiesis | |
| Xia and Tian, 2016 [27] | 90/M | 1 | Ossified | T10–11 | Dorsal | Spinal cord injury after fall | GTR | NA | NA | Psammoma bodies, bone trabeculae | |
| Prakash et al., 2018 [29] | 60/F | 1 | Ossified | T7–8 | Dorsolateral | Myelopathy | GTR | Improved (6 month) | NA | Psammoma bodies, immature bony trabeculae | |
| Sakamoto et al., 2018 [38] | 57/F | 1 | Ossified | C7 | Ventrolaterodorsal | Myelopathy | STR | Improved | NA | Osseous core, fibrous | |
| Murakami et al., 2019 [4] | 29/F | 1 | Ossified | T12 | Lateral | Back pain, leg numbness | GTR + dura | Unchanged (12 months) | NA | Psammoma bodies, mature bone tissue | |
| Taha et al., 2019 [30] | 22/F | 1 | Ossified | T4–5 | Dorsal | Myelopathy | GTR | Improved (6 month) | NA | Psammoma bodies, bone trabeculae | |
| Wang et al., 2019 [31] | 52/F | 1 | Ossified | T4 | Dorsal | Back pain | GTR | Improved | No (2.5 years) | Psammoma bodies, immature trabecular bone, hematopoiesis | |
| Xu et al., 2020 [32] | 85/F | 1 | Ossified | T11 | Lateral | Back pain, leg pain | GTR + dura | Improved | No (1 year) | Psammoma bodies | |
| Buchanan et al., 2021 [33] | 64/M | 1 | Ossified | T4 | Dorsal | Myelopathy | GTR + dura | Improved (6 month) | NA | Psammoma bodies, bone formation, osseous metaplasia | |
| Wong et al., 2021 [34] | 75/F | 1 | Ossified | T10- T11 | NA | Myelopathy | GTR + dura | Not improved (6 months) | NA | Psammoma bodies, immature trabeculae bone | |
| Thakur et al., 2021 [35] | 74/F | 1 | Ossified | T8 | Ventrolateral | Tingling paresthesia | GTR + dura | Improved | NA | Psammoma bodies, bony hard-tissue fragments | |
| Dong et al., 2022 [36] | 76/F | 5 | Ossified | T7–12 | Dorsal | Myelopathy | GTR + dura | Improved | No | Psammoma bodies, trabecular bone, hematopoiesis | |
| Xu et al., 2023 [39] | 68/F | 1 | Ossified | T10 | Dorsal | Paresthesia, gait disturbance | GTR | Improved | No | meningioma with diffused psammomatous bodies | |
| Taha et al., 2024 (present) | 80/F | 1 | Ossified,calcified | T10–11 | Dorsal | Lower limb weakness | GTR | Improved | No | classical psammoma bodies, characterized by calcium deposits |
| Study (Year) . | Age/ Gender . | . | Tumor number . | Ossified . | Level . | Location . | Symptoms . | Treatment . | Clinical outcomes . | Recurrence . | Histological characteristics . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Roger et al., 1928 [5] | 16/F | 1 | Ossified | T9 | Lateral | Myelopathy | GTR | Improved (3 months) | No | Psammoma bodies, bone cells | |
| Freidberg et al., 1972 [6] | 69/F | 1 | Ossified | T1–2 | Ventral | Myelopathy | GTR + dura | Improved (6 weeks) | NA | Psammoma bodies, mature cancellous bone | |
| Kandel et al., 1989 [7] | 17/F | 1 | Ossified | T8 | Dorsal | Myelopathy | GTR | NA | No | Meningotheliomatous, psammoma bodies, bone spicule | |
| Niijima et al., 1993 [8] | 75/F | 1 | Ossified | T8–9 | Dorsolateral | Myelopathy | GTR + dura | Improved (14 months) | NA | Psammoma bodies, bone spicule | |
| Kitagawa et al., 1994 [9] | 75/F | 1 | Ossified | T9–10 | NA | Myelopathy | NA | NA | NA | Psammoma bodies, bone tissue | |
| 60/F | 1 | Ossified | T6–8 | NA | Myelopathy | NA | NA | NA | Psammoma bodies, bone tissue | ||
| Nakayama et al., 1996 [10] | 74/F | 1 | Ossified | T9 | Dorsal | Myelopathy | GTR | NA | NA | Matured lamellar bone tissue | |
| 45/M | 1 | Ossified | C1–3 | Ventral | Myelopathy | GTR | NA | NA | Matured bone tissue | ||
| Huang et al., 1999 [11] | 73/F | 1 | Ossified | T5 | Lateral | Myelopathy | GTR | Improved | NA | Psammoma bodies, bone marrow | |
| Saito et al., 2001 [12] | 54/F | 1 | Ossified | T11 | Dorsal | NA | GTR + dura | Improved | No | Metaplastic (osseous) | |
| Naderi et al., 2001 [13] | 15/M | 1 | Ossified | T4 | Dorsal | Myelopathy | GTR + dura | Improved (3 months) | NA | Psammoma bodies, mature bone tissue | |
| Liu et al., 2006 [14] | 70/F | 1 | Ossified | T11 | Dorsolateral | Myelopathy | GTR | Improved (2 years) | No | Psammoma bodies, woven bone | |
| Hirabayashi et al., 2009 [15] | 82/F | 1 | Partially ossified | L3 | Dorsolateral | Cauda equina syndrome | GTR | Improved | No (5 years) | Osseous | |
| Tahir et al., 2009 [16] | 40/F | 1 | Partially ossified | T6 | Dorsolateral | Myelopathy | GTR | Improved (8 months) | No | Mineralized bone | |
| Uchida et al., 2009 [17] | 40/F | 2 | Ossified | T8 and T12 | Dorsal, dorsolateral | Myelopathy | GTR + dura | Improved | No (2 years) | Psammoma bodies, mature bone | |
| Licci et al., 2010 [18] | 58/F | 1 | Ossified | T6 | Dorsal | Myelopathy | GTR | Improved (1 year) | NA | Psammoma bodies, lamellar bone tissue, hematopoiesis | |
| Chotai et al., 2013 [19] | 61/F | 1 | Ossified | T4–5 | Dorsal | Myelopathy | GTR + dura | Improved (1 month) | NA | Psammoma bodies, mature lamellar bone, hematopoiesis | |
| Study (Year) | Age/Gender | Tumor number | Ossified | Level | Location | Symptoms | Treatment | Clinical outcomes | Recurrence | Histological characteristics | |
| Ju et al., 2013 [20] | 61/F | 1 | Ossified | T9–10 | Lateral | Myelopathy | GTR + dura | Improved (1 month) | NA | Heterotopic ossification | |
| Taneoka et al., 2013 [21] | 78/F | 1 | Ossified | T9 | Dorsal | Myelopathy | GTR + dura | Improved | NA | Psammoma bodies, mature bone, hematopoiesis | |
| Yamane et al., 2014 [22] | 61/F | 1 | Ossified | T12 | Ventrolateral | Myelopathy | GTR | Improved | No (2 years) | Psammoma bodies, cancellous bone with bone marrow | |
| Chan et al., 2014 [23] | 64/F | 1 | Ossified | T9–10 | Dorsal | Myelopathy | GTR | Improved (6 month) | NA | Psammoma bodies, bone marrow, hematopoiesis | |
| Alafaci et al., 2015 [24] | 45/M | 1 | Ossified | T2–3 | Ventral 4, lateral 1, dorsal 4 | Myelopathy | GTR | Improved | No | Seven cases of osseous component in association with psammoma bodies, two cases of immature bone trabeculae | |
| 75/F | 1 | Ossified | T3–4 | Myelopathy | GTR | Improved | No | ||||
| 86/F | 1 | Ossified | T3–4 | Myelopathy | GTR | Improved | No | ||||
| 65/F | 1 | Ossified | T7 | Myelopathy | GTR | Improved | No | ||||
| 72/F | 1 | Ossified | C7 | Myelopathy | STR | Improved | No | ||||
| 40/F | 1 | Ossified | T1–2 | Myelopathy | STR | Improved | No | ||||
| 65/F | 1 | Ossified | T7–8 | Myelopathy | GTR | Improved | No | ||||
| 40/F | 1 | Ossified | C7 | Myelopathy | GTR | Improved | No | ||||
| 41/F | 1 | Ossified | T2–3 | Myelopathy | GTR | Improved | No | ||||
| Kim et al., 2016 [28] | 51/F | 1 | Ossified | T4 | Dorsal | Myelopathy | GTR | Improved | No | Psammoma bodies | |
| 77/F | 1 | Ossified | T9 | Dorsal | Myelopathy | GTR | Improved | No | Psammoma bodies | ||
| Demir et al., 2016 [25] | 26/F | 1 | Ossified- calcified | T9–11 | Dorsal | Myelopathy | GTR | NA | NA | Psammoma bodies | |
| Cochran et al., 2016 [26] | 47/F | 1 | Ossified | T8 | Ventral | Radiculopathy | GTR | Improved | No (22 months) | Psammoma bodies, bone marrow, hematopoiesis | |
| Xia and Tian, 2016 [27] | 90/M | 1 | Ossified | T10–11 | Dorsal | Spinal cord injury after fall | GTR | NA | NA | Psammoma bodies, bone trabeculae | |
| Prakash et al., 2018 [29] | 60/F | 1 | Ossified | T7–8 | Dorsolateral | Myelopathy | GTR | Improved (6 month) | NA | Psammoma bodies, immature bony trabeculae | |
| Sakamoto et al., 2018 [38] | 57/F | 1 | Ossified | C7 | Ventrolaterodorsal | Myelopathy | STR | Improved | NA | Osseous core, fibrous | |
| Murakami et al., 2019 [4] | 29/F | 1 | Ossified | T12 | Lateral | Back pain, leg numbness | GTR + dura | Unchanged (12 months) | NA | Psammoma bodies, mature bone tissue | |
| Taha et al., 2019 [30] | 22/F | 1 | Ossified | T4–5 | Dorsal | Myelopathy | GTR | Improved (6 month) | NA | Psammoma bodies, bone trabeculae | |
| Wang et al., 2019 [31] | 52/F | 1 | Ossified | T4 | Dorsal | Back pain | GTR | Improved | No (2.5 years) | Psammoma bodies, immature trabecular bone, hematopoiesis | |
| Xu et al., 2020 [32] | 85/F | 1 | Ossified | T11 | Lateral | Back pain, leg pain | GTR + dura | Improved | No (1 year) | Psammoma bodies | |
| Buchanan et al., 2021 [33] | 64/M | 1 | Ossified | T4 | Dorsal | Myelopathy | GTR + dura | Improved (6 month) | NA | Psammoma bodies, bone formation, osseous metaplasia | |
| Wong et al., 2021 [34] | 75/F | 1 | Ossified | T10- T11 | NA | Myelopathy | GTR + dura | Not improved (6 months) | NA | Psammoma bodies, immature trabeculae bone | |
| Thakur et al., 2021 [35] | 74/F | 1 | Ossified | T8 | Ventrolateral | Tingling paresthesia | GTR + dura | Improved | NA | Psammoma bodies, bony hard-tissue fragments | |
| Dong et al., 2022 [36] | 76/F | 5 | Ossified | T7–12 | Dorsal | Myelopathy | GTR + dura | Improved | No | Psammoma bodies, trabecular bone, hematopoiesis | |
| Xu et al., 2023 [39] | 68/F | 1 | Ossified | T10 | Dorsal | Paresthesia, gait disturbance | GTR | Improved | No | meningioma with diffused psammomatous bodies | |
| Taha et al., 2024 (present) | 80/F | 1 | Ossified,calcified | T10–11 | Dorsal | Lower limb weakness | GTR | Improved | No | classical psammoma bodies, characterized by calcium deposits |
GTR, gross total resection; STR, subtotal resection.
Our analysis indicates that while ossified spinal meningioma exhibits a higher prevalence among females, no substantiated correlation between this condition and sex hormones has been identified [40].
While CT scans offer superior diagnostic capabilities for spinal tumors compared to MRI, differentiation between calcification and ossification necessitates histopathologic examination [33]. The mechanism underlying the ossification of spinal meningiomas remains unclear, though several theories have been proposed. Kubota et al. [37] suggested that ossification occurs as an advanced stage of psammomatous calcification of meningioma as part of the neoplastic process. However, this theory does not account for all cases of ossified spinal meningioma documented in the literature, as ossification can occur without preceding psammomatous calcification [3]. Another theory proposed by Uchida et al. [17] implicates genetic predispositions, such as osteoblast transcription factors SOX9 and Runx-2, although this may not be applicable to all patients. Genetic analysis is not routinely indicated for such tumor cases.
Surgical intervention remains the cornerstone of treatment for spinal meningiomas, whether calcified or completely ossified. Computed tomography (CT) plays a crucial role in preoperative planning and identifying the ossified component of the tumor. Dense calcifications serve as a guide for intraoperative tumor localization using fluoroscopy or O-arm imaging. Surgical resection of ossified spinal meningioma can be challenging due to tumor adherence to adjacent neural elements and dural invasion. This adherence may result in an unclear dissection plane, potentially impacting postoperative outcomes and hindering gross total tumor resection, with subsequent risks of spinal cord trauma or injury [13, 24]. Nonetheless, reported literature indicates minimal postoperative complications thus far.
Conclusion
Ossified meningiomas represent benign yet exceedingly rare spinal tumors. Across the documented literature, clinical presentations vary widely but exhibit common patterns. There is a notable predominance of female patients, with lesions commonly observed in the thoracic spine. Surgical excision remains the cornerstone of treatment, necessitating careful consideration to mitigate potential complications.
Conflict of interest statement
None declared.
Funding
None declared.
Ethical approval
Ethics clearance was not necessary since the University waives ethics approval for publication of case reports involving no patients’ images, and the case report is not containing any personal information. The ethical approval is obligatory for research that involve human or animal experiments.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.



