-
PDF
- Split View
-
Views
-
Cite
Cite
Andrej Nikolovski, Ana Lazarova, Dino Mojsilovic, Gligor Ristovski, Ivan Argirov, Cemal Ulusoy, Spontaneous omental infarction in an obese young female patient treated with laparoscopy: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 6, June 2024, rjae392, https://doi.org/10.1093/jscr/rjae392
Close - Share Icon Share
Abstract
Partial infarction of the great omentum is a rare cause of abdominal pain and may present as a surgical emergency. Omental infarction might occur due to its torsion, but cases without obvious cause are reported. Risk factors related to this condition are overweight, obesity, abdominal trauma, recent abdominal surgery, hypercoagulability, postprandial vascular congestion and an increase in intra-abdominal pressure. Because of the condition’s rarity, most patients are treated with surgery and the diagnosis is established intraoperatively. Preoperative diagnosis allows successful conservative treatment with analgesics and anti-inflammatory drugs. This case reports a young female patient with class III obesity presented with spontaneous partial infarction of the great omentum treated with laparoscopy.
Introduction
Partial omental infarction (OI) of the great omentum is an unusual and rare cause of acute abdominal pain that often mimics other abdominal emergencies. The right side of the omentum is mostly affected; thus, the condition might be mixed with acute appendicitis and acute cholecystitis [1]. Compared with acute appendicitis, omental infarction has an incidence of 0.0016–0.37%, equivalent to a ratio of less than 4 cases per 1000 cases of appendicitis [2]. OI occurs as a consequence of torsion of the omental vascular pedicle. However, cases with spontaneous OI (without torsion) are described [3]. In these patients, certain predisposing factors are reported. One of them is obesity [4–6]. Conservative and operative treatments are described, depending on the diagnostic accuracy [7]. We present a case of a young female patient with class III obesity and partial spontaneous omental infarction presented as acute appendicitis, treated with laparoscopy due to diagnostic uncertainty. Signed informed consent was obtained from the patient’s parent.
Case report
A 16-year-old female patient with obesity class III (body mass index of 41.5) presented to the emergency ward with abdominal pain for the last 48 h. No other comorbidities or previous abdominal surgery were reported. Physical examination was positive for lower right quadrant abdominal pain and for signs of local peritonism. The patient did not report loss of appetite, nausea, or vomiting. Laboratory analysis showed elevated serum levels of glycaemia of 6.48 mmol/l (normal range of 3.90–5.83 mmol/L) and C-reactive protein level of 63.30 mg/L (normal range of 0.00–5.00 mg/l). Abdominal ultrasonography failed to conclude the presence of intra-abdominal condition. Abdominal computerized tomography (CT) scan showed inflammation in the surrounding fat tissue of the pericecal region (Figs 1 and 2). No CT signs for acute appendicitis were present. Due to diagnostic uncertainty, an explorative laparoscopy was performed. Intraoperatively, a partial infarction of the right part of the great omentum was seen (Fig. 3). It was resected with a bipolar device (Video supplement S1) and appendectomy was performed additionally. Resected omentum and appendix were extracted via the umbilical port with minimal extension. The operative time was 65 min.
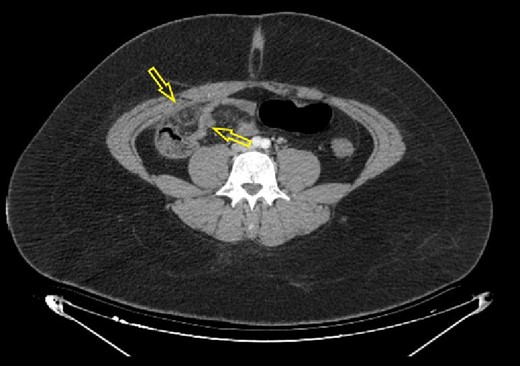
Axial abdominal CT scan (native series) showing intra-abdominal fat inflammation in the pericecal region (arrows).
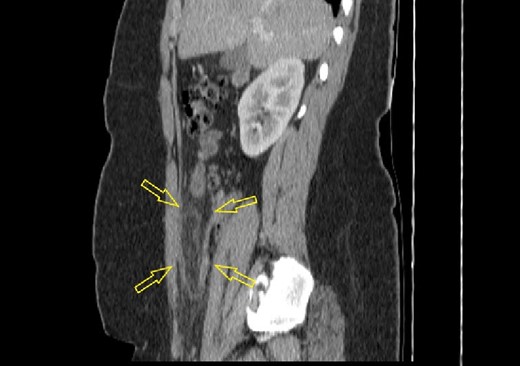
Sagittal abdominal CT scan (native series) showing intra-abdominal fat inflammation in the pericecal region (arrows).

Intraoperative finding of partial infarction of the right side of the great omentum.
In the postoperative period, there was an episode of febricity (second postoperative day) that subsided with antipyretics. The length of hospital stay was 3 days.
The pathology report confirmed the presence of hemorrhage and adipose tissue necrosis (Fig. 4A–D).
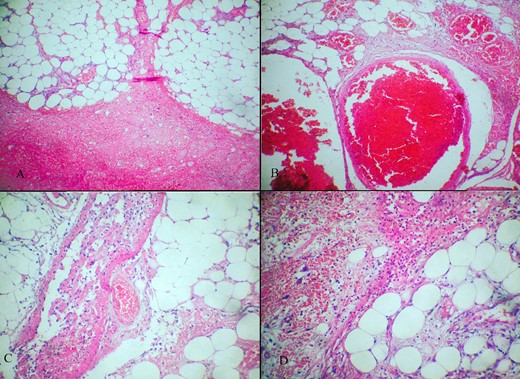
(A–D) Hematoxylin-eosin stain showing (A) adipose tissue with wide hemorrhage; (B) marked vascular congestion; (C) thrombosis in certain vessels; (D) bleeding, adipose necrosis and reactive inflammation.
Discussion
Omental infarction was initially described by Bush in 1896 as a ‘case of hemorrhage into the great omentum’ [8]. Its reported incidence is 0.3% with male gender predomination and a mean age of 45.7 years [1, 2]. Reported predisposing factors related to this condition include obesity, abdominal trauma, recent abdominal surgery, hypercoagulability, postprandial vascular congestion and an increase in intra-abdominal pressure. Segmental infarction of the great omentum is classified as whether it is torsion-related or not [9]. In this report, class III obesity was the only recognized factor to be related to the patient’s condition and no torsion of the great omentum was noted during laparoscopy.
In more than 90% of cases with OI, the right side of the great omentum is affected most likely due to its greater length and the tendency to twist along its long axis [10]. This leads to clinical presentation mimicking acute cholecystitis or appendicitis as in this case.
The main symptom of the OI is abdominal pain. It may be accompanied by fever and inflammatory markers elevation [1].
Diagnosis consists of a physical exam and blood count test fulfilled with abdominal ultrasound and abdominal computerized tomography scan. Abdominal ultrasound may reveal hyperechoic mass thus raising suspicion for possible OI existence. An abdominal CT scan can confirm the diagnosis. [11]. However, proper preoperative diagnosis is established in 5% of cases [10]. Improvement of the imaging modalities might lead to improvement in the diagnosis of OI and results with more cases treated without surgery in the future [2]. In this case, CT scan excluded acute appendicitis, but the radiology report was inconclusive for the OI existence, which resulted in the decision for exploratory laparoscopy.
Controversies on the OI treatment exist. Both conservative and operative options are reported to result in success. Conservative treatment reported to be successful consists of oral analgesia and anti-inflammatory drugs [9, 11]. Surgery comprehends partial resection of the infarcted great omentum and is usually done laparoscopically [3, 12, 13].
In the systematic review of Medina-Gallardo et al., conservative treatment was conducted in the majority of cases (73.3%) with a symptom resolution in 84.1% [1]. The failure of the conservative treatment has been reported in 15.6% of the cases and laparoscopic resection was performed as an alternative treatment option [9]. In the case of failed conservative treatment, patients treated with laparoscopy were converted to open laparotomy in 27.2%. In contrast, no conversion in the group of patients initially treated with surgery occurred. The only factor associated with conservative treatment failure reported was younger age (mean 37.9 ± 15.1 standard deviation). In terms of the hospital stay length, patients treated with surgery had significantly shorter stays [1].
This case presents a young female patient with class III obesity and spontaneous partial OI. Due to the diagnostic uncertainty, the patient was successfully treated with laparoscopic exploration and partial omental resection.
Conflict of interest statement
None declared.
Funding
None declared.



