-
PDF
- Split View
-
Views
-
Cite
Cite
Alvaro Ducas, Paula Lopez, Beatriz Figueroa, Emiliano G Manueli Laos, Alberto Mangano, Chandra Hassan, Challenges in the surgical treatment and management of the patient with super super obesity, Journal of Surgical Case Reports, Volume 2024, Issue 4, April 2024, rjae208, https://doi.org/10.1093/jscr/rjae208
Close - Share Icon Share
Abstract
Obesity is defined by the Body Mass Index (BMI) which is derived by the weight and height of a person (BMI > 30). Furthermore, obesity is classified as super-obesity (BMI >50 kg/m2) and super-super obesity (BMI >60 kg/m2) by the International Bariatric Surgery Registry (Renquist K. Obesity classification. Obes Surg 1997;7:523). Patients with super-super obesity have a greater incidence of comorbid diseases and are at greater risk of postoperative morbidity and mortality and longer length of hospital stay (LOS). Soong et al. described short-term outcomes after weight loss surgery comparing a group of patients with super-obesity with another group of patients with super-super obesity. The authors concluded that experienced surgeons could achieve comparable outcomes in both groups. However, higher BMI is associated with longer operative time, longer LOS, and delayed discharge to chronic care facilities (Soong TC, Lee MH, Lee WJ, et al. Long-term efficacy of bariatric surgery for the treatment of super-obesity: comparison of SG, RYGB, and OAGB. Obes Surg. 2021;31:3391–99. https://doi.org/10.1007/s11695-021-05464-0). The following paradigmatic case report aims at showing the complex management of a patient with super-super obesity, with BMI of 141.2 kg/m2 and associated multiple comorbidities.
Introduction
Obesity (BMI > 30) is classified as super-obesity (BMI >50 kg/m2) and super-super obesity (BMI >60 kg/m2) by the International Bariatric Surgery Registry [1]. Patients with super-super obesity have a greater incidence of comorbid diseases and are at greater risk of postoperative morbidity and mortality and longer length of hospital stay (LOS). Soong et al. described short-term outcomes after weight loss surgery comparing a group of patients with super-obesity with another group of patients with super-super obesity. The authors concluded that experienced surgeons could achieve comparable outcomes in both groups. However, higher BMI is associated with longer operative time, longer LOS, and delayed discharge to chronic care facilities [2].
The following paradigmatic case report aims at showing the complex management of a patient with super-super obesity, with BMI of 141.2 kg/m2 and associated multiple comorbidities.
Case report
The patient is a 33-year-old male with BMI 141.2 kg/m2 (396.7 kg– 167.6 cm), bed-bound since June 2019, came to the emergency department on a bariatric bed presenting with pain in the legs, fever, and bilateral lower extremity cellulitis. His medical history included: end stage renal disease, deep venous thrombosis, and pulmonary embolism (which was at the time in treatment with Warfarin 10.5 mg daily), obstructive sleep apnea, pulmonary hypertension, and permanent tracheostomy (with O2 at 40% 6 L), type 2 diabetes mellitus.
The patient underwent an initial treatment with Vancomycin 1.25 g, Meropenem 1 g for 7 days. The clinical presentation entailed multiple episodes of fever, tachycardia with worsening respiratory symptoms and acidosis. Severe anemia was also present with hemoglobin of 6 that required multiple blood transfusions. The case was managed in a multidisciplinary way, involving professionals from the following specialties: family medicine, cardiology, pulmonology, gastroenterology, nephrology, infectious disease, hematology, wound care, pharmacology, and ethics. During the 28th day of stay, the general surgery department was consulted for the evaluation of a bariatric treatment. Clinical ethics was involved as well, and the decision was to prepare the patient and hospital environment for a robotic assisted sleeve gastrectomy procedure.
The patient started a liquid diet which was maintained for 3 weeks. The team had to be prepared for the surgical procedure. Transportation, operation table and footrest had to be set up for the patient (Fig. 1). Measurement of abdominal wall thickness was carried out using portable ultrasound.

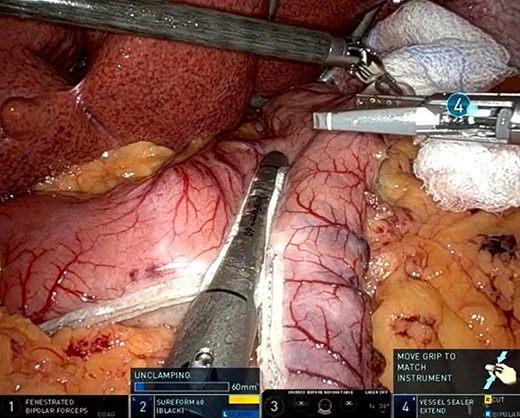
At the time when the robotic assisted sleeve gastrectomy was performed the patient’s weight was 322 kg. A 5 mm supraumbilical incision was made left of the midline. OptiView™ trocar was used for direct vision insertion of a 5 mm 0° angle camera. Both 8 and 12-mm ports were inserted in the right upper quadrant and an 8 mm trocar was placed, under direct vision, in the left upper quadrant. Then, a 5 mm incision was made in the epigastric area, followed by insertion of the Nathanson retractor which was used to pull up the left hepatic lobe. The patient was found to have a very large liver, as well as enlarged spleen extending to the subcostal border. The sleeve gastrectomy was started at ~6 cm proximal from the pylorus, by firing a 60 mm black Da Vinci stapler cartridge with seam guard reinforcement. Black, green, and blue loads were used to perform the sleeve gastrectomy (Fig. 2). In this case, it was particularly difficult to dissect the posterior fundus and control the short gastric vessels at the gastro splenic ligament secondary to limited space because of enlarged liver and central obesity. An additional port was required for assistance in the retraction (Fig. 3).
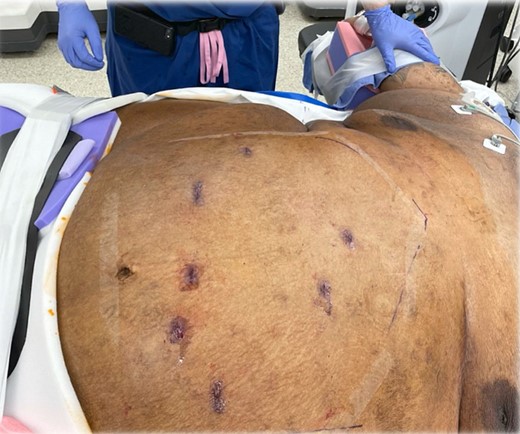
The patient was briefly monitored in the surgical Intensive Care Unit (ICU) and then went back on the floor. The diet slowly advanced and no surgical complications were recorded, but the patient had a long recovery in the hospital due to several comorbidities. Discharge was tried many times, but it was not achieved as planned due to social reasons. After 7 months of recovery, and multiple soft tissue and skin infections, it was possible to discharge the patient to a rehabilitation facility which was necessary because the patient was not able to sit up and move by himself.
At the last follow up, the BMI was 77.3 kg/m2 (217 kg) with a percent excess body weight loss of 54.9% and a percent weight loss of 45.2%.
Discussion
The number of obese patients and super-super obesity is increasing each year, especially in the United States. According to the Centers for Disease Control and Preventions (CDC) the obesity prevalence in the US is 41.9% [3]. Morbidity and mortality rate are related to the comorbid disease of the patient and not only to the BMI. When treating patients with super-super obesity, the scenario is complex and needs to be planned in advance, also specialized surgeons will promote better outcomes and a multidisciplinary team will make the difference.
Soong et al. compared outcomes between one anastomosis gastric bypass (OAGB), sleeve gastrectomy (SG) and Roux-en-Y gastric bypass (RYGB) concluding that OAGB and SG have a similar safety profile but safer than RYGB. Also, RYGB has no better weight loss results in the long-term follow up compared to SG. Although RYGB has a better anti-metabolic effect the other two procedures, the conclusion shows that SG has lower revision rates [2].
Conflict of interest statement
All the authors have no conflict of interest to declare in relation to the present publication.
Funding
None declared.



