-
PDF
- Split View
-
Views
-
Cite
Cite
Howard H Y Tang, Daming Pan, Andrew Fitzdowse, Aaron Ow, Stephen Chan, Jason S C Tan, A rare case of appendiceal haemorrhage causing life-threatening haematochezia, Journal of Surgical Case Reports, Volume 2024, Issue 12, December 2024, rjae705, https://doi.org/10.1093/jscr/rjae705
Close - Share Icon Share
Abstract
Our case involved a 28-year-old man who presented with life-threatening haematochezia. Computed tomography angiogram revealed contrast extravasation from the appendix pooling in the caecum. Management via laparoscopic stapled partial caecectomy was successful. Histopathology revealed focal mild acute appendicitis with focal ulceration to submucosa.
Introduction
Large volume haematochezia is life threatening and necessitates urgent diagnosis and treatment. Commonest causes include diverticular bleed of the colon and anorectal disorders [1]. Appendiceal haemorrhage is rare. We hereby describe a case of significant lower gastrointestinal haemorrhage from the appendix.
Case presentation
A 28-year-old male of East Asian ethnicity presented with 1-day history of hematochezia of ~700 ml. His past medical history included gout, diet-controlled diabetes, oesophagitis and duodenal ulcer in 2016 that did not require endoscopic intervention. He had recently taken ibuprofen for headaches.
On admission, he was pale, tachycardic at 105 beats per minute with a blood pressure of 107/70 mmHg. Haemoglobin was 95 g/L (normal range 130–180 g/L), with a white cell count of 7.8 x109/L (normal range 3.6–11 x109/L), platelets count of 289 x109/L (normal range 140–400 x109/L) and mean corpuscular volume of 76 fL (normal range 80–100 fL). Computed tomography abdominal angiogram (CTA) demonstrated no active contrast blush or abnormality within the gastrointestinal tract. The patient was resuscitated and transfused two units of packed red blood cells, with plan for gastroscopy the next day to exclude upper gastrointestinal bleeding due to recurrent duodenal ulcers.
On Day 1 of admission, his haemoglobin count continued to drop to 89 g/L despite further transfusions and a normal gastroscopy. Repeat CTA performed at the time of another episode of large volume haematochezia demonstrated contrast extravasation arising from the appendix on the arterial phase, with pooling and spillage of contrast into the caecum on the subsequent phases, consistent with active haemorrhage within the appendix (Fig. 1). No overt appendiceal or caecal mass was seen. After discussion with the interventional radiologist, we decided not to pursue endovascular management. The patient was further resuscitated and preceded to a diagnostic laparoscopy. The appendix appeared healthy with neither overt masses nor signs of peritoneal disease. The appendiceal artery was controlled by endoclips, and the decision was made to perform a limited stapled caecectomy to incorporate the entire base of the appendix.

CT-angiogram, late arterial phase. Coronal CT slice showing contrast extravasation into the appendiceal lumen and spillage into the caecum.
Macroscopic examination of the specimen demonstrated a clot-filled appendiceal lumen and a minimal increase in darkness in the submucosa. Microscopic examination demonstrated focal mucosal ulceration of 2 mm depth, with inflammatory infiltration extending to the muscularis propria, interstitial haemorrhage, and fibrosis (Figs 2 and 3). There was no eosinophilia or significant microscopic inflammatory exudate. This was deemed the most likely origin of bleeding with the final histological diagnosis of focal mild acute appendicitis with focal ulceration to submucosa (Fig. 1).
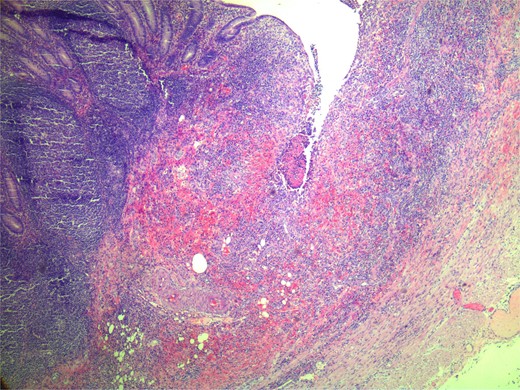
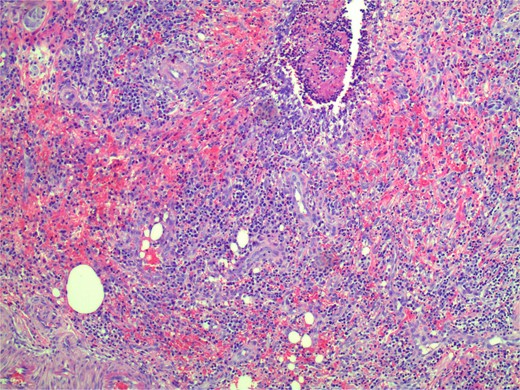
Microscopic zoomed in view of small ulceration measured to be 2 mm.
The patient had an uncomplicated post-operative course and was discharged 2 days after surgery with planned outpatient colonoscopy.
Discussion
Haematochezia is a common surgical presentation. Appendiceal haemorrhage, however, is rarely encountered, accounting for 0.014% of cases of gastrointestinal haemorrhage in a recent Chinese series [2]. Causes of appendiceal haemorrhage can be divided into neoplastic and non-neoplastic. Past case reports have described malignancy, vascular malformation, ulceration, and diverticular bleed as some of the causes, summarized in Table 1. Amongst these cases, the sources of bleeding were usually identified by CTA with contrast extravasation into the appendiceal lumen, or direct visualization of active bleeding from the appendiceal orifice on colonoscopy (Table 1).
Compilation of case reports with appendiceal lesions presenting with haematochezia
| Demographics . | Diagnosis . | Investigation and findings . | Treatment . | References . |
|---|---|---|---|---|
| Neoplastic causes | ||||
| 88 Male | Low grade mucinous neoplasm |
| Appendicectomy | Karatas 2022 [3] |
| 73 Male | Mucinous adenocarcinoma |
| Right hemicolectomy | Wijayaratne 2021 [4] |
| 81 Male | Primary adenocarcinoma |
| Right hemicolectomy | Sain 2021 [5] |
| Benign causes | ||||
| 41 Male | Mucosal erosion |
| Laparoscopic appendicectomy | Baek 2010 [6] |
| 72 Male | Angiodysplasia |
| Laparoscopic appendicectomy and wedge resection of caecum | Choi [7] |
| 37 Female | Endometriosis |
| Partial caecectomy | Ostiz Llanos [8] |
| 71 Male | Diverticular bleeding |
| Appendiceal orifice clipped during colonoscopy Laparoscopic appendicectomy | Nakashima [9] |
| 57 Male | Arteriovenous malformation of mesoappendix |
| Laparoscopic appendicectomy | Nguyen [10] |
| 32 Male | Dieulafoy’s lesion |
| Laparoscopic appendicectomy | Zhou [11] |
| Demographics . | Diagnosis . | Investigation and findings . | Treatment . | References . |
|---|---|---|---|---|
| Neoplastic causes | ||||
| 88 Male | Low grade mucinous neoplasm |
| Appendicectomy | Karatas 2022 [3] |
| 73 Male | Mucinous adenocarcinoma |
| Right hemicolectomy | Wijayaratne 2021 [4] |
| 81 Male | Primary adenocarcinoma |
| Right hemicolectomy | Sain 2021 [5] |
| Benign causes | ||||
| 41 Male | Mucosal erosion |
| Laparoscopic appendicectomy | Baek 2010 [6] |
| 72 Male | Angiodysplasia |
| Laparoscopic appendicectomy and wedge resection of caecum | Choi [7] |
| 37 Female | Endometriosis |
| Partial caecectomy | Ostiz Llanos [8] |
| 71 Male | Diverticular bleeding |
| Appendiceal orifice clipped during colonoscopy Laparoscopic appendicectomy | Nakashima [9] |
| 57 Male | Arteriovenous malformation of mesoappendix |
| Laparoscopic appendicectomy | Nguyen [10] |
| 32 Male | Dieulafoy’s lesion |
| Laparoscopic appendicectomy | Zhou [11] |
Compilation of case reports with appendiceal lesions presenting with haematochezia
| Demographics . | Diagnosis . | Investigation and findings . | Treatment . | References . |
|---|---|---|---|---|
| Neoplastic causes | ||||
| 88 Male | Low grade mucinous neoplasm |
| Appendicectomy | Karatas 2022 [3] |
| 73 Male | Mucinous adenocarcinoma |
| Right hemicolectomy | Wijayaratne 2021 [4] |
| 81 Male | Primary adenocarcinoma |
| Right hemicolectomy | Sain 2021 [5] |
| Benign causes | ||||
| 41 Male | Mucosal erosion |
| Laparoscopic appendicectomy | Baek 2010 [6] |
| 72 Male | Angiodysplasia |
| Laparoscopic appendicectomy and wedge resection of caecum | Choi [7] |
| 37 Female | Endometriosis |
| Partial caecectomy | Ostiz Llanos [8] |
| 71 Male | Diverticular bleeding |
| Appendiceal orifice clipped during colonoscopy Laparoscopic appendicectomy | Nakashima [9] |
| 57 Male | Arteriovenous malformation of mesoappendix |
| Laparoscopic appendicectomy | Nguyen [10] |
| 32 Male | Dieulafoy’s lesion |
| Laparoscopic appendicectomy | Zhou [11] |
| Demographics . | Diagnosis . | Investigation and findings . | Treatment . | References . |
|---|---|---|---|---|
| Neoplastic causes | ||||
| 88 Male | Low grade mucinous neoplasm |
| Appendicectomy | Karatas 2022 [3] |
| 73 Male | Mucinous adenocarcinoma |
| Right hemicolectomy | Wijayaratne 2021 [4] |
| 81 Male | Primary adenocarcinoma |
| Right hemicolectomy | Sain 2021 [5] |
| Benign causes | ||||
| 41 Male | Mucosal erosion |
| Laparoscopic appendicectomy | Baek 2010 [6] |
| 72 Male | Angiodysplasia |
| Laparoscopic appendicectomy and wedge resection of caecum | Choi [7] |
| 37 Female | Endometriosis |
| Partial caecectomy | Ostiz Llanos [8] |
| 71 Male | Diverticular bleeding |
| Appendiceal orifice clipped during colonoscopy Laparoscopic appendicectomy | Nakashima [9] |
| 57 Male | Arteriovenous malformation of mesoappendix |
| Laparoscopic appendicectomy | Nguyen [10] |
| 32 Male | Dieulafoy’s lesion |
| Laparoscopic appendicectomy | Zhou [11] |
After initial resuscitation, management should prioritize identifying and stopping the bleeding source. While digital subtraction angiography maybe useful in identification of the bleeding vessel, endovascular embolization of the appendiceal artery, an end artery, places the appendix at risk of ischaemia [12]. Smith et al. [12] reported using angioembolization as a temporizing measure for a patient who refused blood products, in which the appendix subsequently developed ischaemia and required appendicectomy. Colonoscopy is another modality to identify the source of bleeding amongst the reported cases, with most describing active bleeding from the appendiceal orifice. However due to the small size of the appendiceal lumen, visualization of the lesion and endoscopic treatments were limited.
The source of bleeding from the appendix was identified using a CTA in our case. As the source of bleeding had been identified, colonoscopy was also not performed to expedite definitive management. Given the proximal location of the bleed relative to the appendiceal base, and the concern of an occult neoplastic process near the base, the decision was made to perform a stapled wedge caecectomy to incorporate the base for a wider margin.
Conclusion
Appendiceal bleeding is a rare cause of haematochezia, and can be caused by neoplastic or benign processes. CTA is a useful tool to identify the source of bleeding and suspicion of the presence of a mass. Endovascular and endoscopic management options are limited due to the risk of ischaemia and the small size of the appendiceal lumen. In the case of a proximal bleeding point, a partial caecectomy can be considered to ensure adequate margins.
Conflict of interest statement
Written consent was obtained from the patient to publish this case report. The authors jointly declare no conflict of interest.
Funding
None declared.
Author contributions
Howard H.Y. Tang (Conceptualization; Writing – original draft, Writing – review & editing); Daming Pan: (Conceptualization; Writing – original draft, Writing – review & editing); Andrew Fitzdowse (Writing – review & editing), Aaron Ow (Writing – review & editing); Stephen Chan (Writing – review & editing), Jason S.C. Tan: (Writing – review and editing, Supervision).
References
Author notes
Howard Tang and Daming Pan contributed equally as co-first authors of the manuscript.



