-
PDF
- Split View
-
Views
-
Cite
Cite
Takao Miki, Satoshi Ohki, Ryo Yamaguchi, Ayako Nagasawa, Shuichi Okonogi, Kiyomitsu Yasuhara, Tamiyuki Obayashi, Successful surgical treatment of a right atrial myxoma with hypothermic circulatory arrest and venous cannulation in pulmonary artery, Journal of Surgical Case Reports, Volume 2024, Issue 10, October 2024, rjae677, https://doi.org/10.1093/jscr/rjae677
Close - Share Icon Share
Abstract
Myxomas are the most common type of benign cardiac tumors, and the right atrium is the second most common location among them, with an incidence ranging from 8.6% to 20% of all cardiac myxomas. Herein, we described a rare case of right atrial myxoma originating from the inferior vena cava orifice. In this case, main pulmonary artery cannulation and moderate hypothermic circulatory arrest were helpful to obtain a clear and simple view of the operative field without blood, which led to complete resection of the tumor with safety and better outcomes with no future recurrence.
Introduction
Most of myxomas, which are the most common in benign cardiac tumors, are located in the left atrium [1, 2]. Right atrial myxomas (RAMs) account for only 10%–20% of all cardiac myxomas [2, 3]. In addition, few cases have been reported to have a stalk on the orifice of the inferior vena cava (IVC) [2], while most of them usually attach to the free atrial wall or interatrial septum [2–4]. Herein, we report a rare case of an asymptomatic RAM originating from the IVC orifice and discuss the efficacy of venous cannulation in the main pulmonary artery, not in the IVC, and hypothermic circulatory arrest for complete tumor resection.
Case report
A 72-year-old male was consulted to our section for the management of a cardiac mass approximately 40 mm in diameter in the right atrium. On admission, he was in stable condition and had no symptoms. His chest X-ray showed a clear lung field and normal cardiothoracic ratio. His laboratory data were within normal limits. His transesophageal echocardiography demonstrated a mass of 42 × 28 mm in size, located in the inferior cavity of the right atrium. The mass was multiple lobulated, pedunculated, and had high mobility (Fig. 1a). In addition, its stalk was attached to the endocardium of the IVC orifice in a narrow range, as was similar to his preoperative coronary computed tomography (CT) scan (Fig. 1b). There were no signs of pulmonary thromboembolization. The mass had no relation to the tricuspid valve. Thus, we decided to surgically remove the tumor to prevent pulmonary embolization. The operation was performed via median sternotomy, followed by harvesting the autologous pericardium. Then, two venous cannulas in size of 28 Fr were inserted: the one was in the superior vena cava directly, and the other one was in the main pulmonary artery, respectively. We avoided usual IVC cannulation through the right atrium, which could have a considerable risk of fragmentation of the tumor during manipulation. Cardiopulmonary bypass was then started, and the core temperature was reduced to 20°C. Circulatory arrest was induced after cardioplegic heart arrest. Through a lateral right-atriotomy, there existed a lobulated, gelatinous, and smooth surfaced tumor in size of 43 × 38 × 25 mm in the inferior cavity of the right atrium (Fig. 2a). The tumor was completely resected successfully, including its stalk and the small lesion of the endocardiu of the IVC orifice. The deficit of the endocardium was closed with autologous pericardium (Fig. 2b). The circulatory arrest time was 19 min. The postoperative course was uneventful. Histopathological examination revealed the tumor, including the endocardium attached to its base, was completely resected (Fig. 3), and diagnosed it as a myxoma. A transthoracic echocardiography 3 years after surgery showed no signs of recurrence.
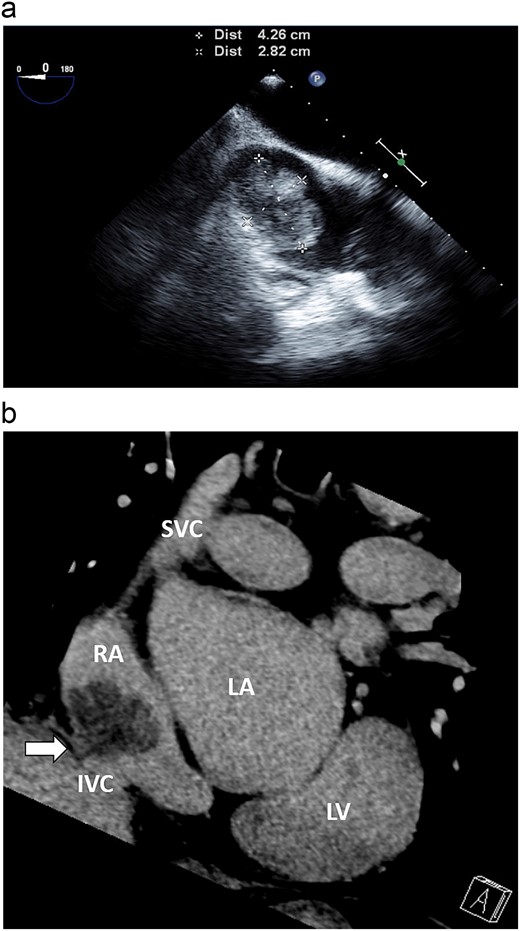
(a) Transesophageal echocardiography demonstrated that the mass was 42 × 28 mm in size, located in the inferior cavity of the right atrium, and was multi-lobulated, pedunculated, and highly mobile. (b) Coronary CT revealed a stalk on the endocardium of the IVC orifice (white arrow).
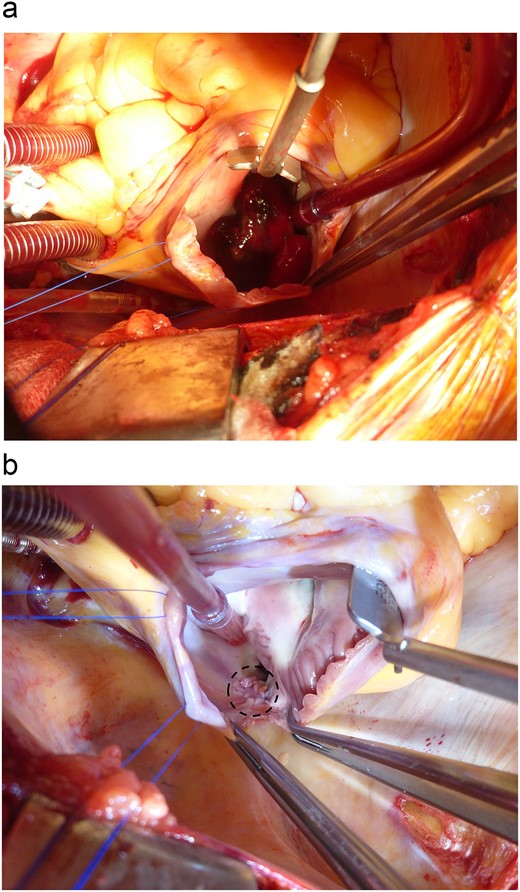
Intraoperative findings. (a) With two venous cannulas both in the superior vena cava and the main pulmonary artery, cardiopulmonary bypass was started. Through a lateral right atriotomy, a lobulated, gelatinous, and smooth surfaced tumor, 43 × 38 mm in diameter, was found. (b) The deficit of the endocardium (black dot circle) was closed with autologous pericardium.
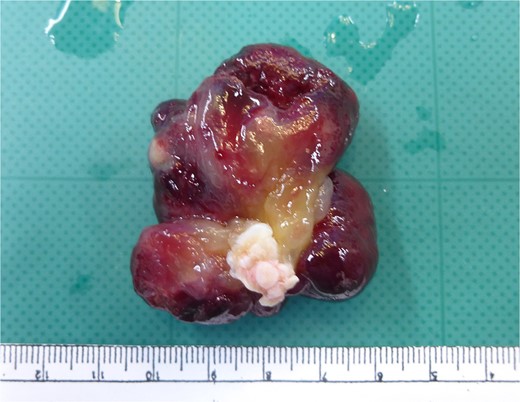
The tumor was completely resected including the endocardium attached to its base.
Discussion
RAMs are relatively rare, which account for only 15%–20% of all cardiac myxomas [1–3]. As widely known, the standard treatment of them is surgical removal [1–8]. To achieve the better outcomes of RAMs, it is essential to avoid tumor fragmentation during manipulation of venous cannulation, especially [3–5]. As the tumor was located in the inferior cavity of the right atrium in our case, we considered that the usual venous cannulation in the IVC through the right atrium free wall was dangerous because of the risk of iatrogenic pulmonary artery embolization due to tumor fragmentation induced by the venous cannula itself. Besides, the venous cannula in the IVC could disturb the operative field and make it difficult to remove the mass with safety, which could lead to the incomplete resection of the mass. That is why we placed another venous cannula in the main pulmonary artery without thrombus. As a result, our patient had no signs of pulmonary embolization after surgery.
Hypothermic circulatory arrest is also helpful for complete tumor resection [4–7]. According to the several reports, very few RAMs had their stalk in the IVC, and in such cases, complete tumor resection were accomplished under a clear operative field without blood due to circulatory arrest [2–7] and a simple view without venous cannula in the IVC [5, 6]. Bortolloti et al. reported a case of RAM originating from the IVC, in which cardiopulmonary bypass was instituted by bi-caval venous cannulation through the right atrium at first [7]. However, they finally removed the IVC cannula temporarily under moderate hypothermic low-flow circulation in order to get better exposure of the tumor [7]. Consequently, we assume that venous cannulation in the main pulmonary artery and hypothermic circulatory arrest were feasible for complete resection of a RAM originating from the IVC, as in our case. Because myxomas are reported to have a certain degree of recurrence [2, 8], a careful continuous follow-up is essential.
In conclusion, we experienced a rare case of right atrial myxoma originating from the IVC orifice. In this case, venous cannulation in the main pulmonary artery and moderate hypothermic circulatory arrest were effective in getting a clear and simple view of the operative field without blood and venous cannula in the IVC, which contributed to complete resection of the tumor with safety and better outcomes with no future recurrence.
Conflict of interest statement
All authors declare that they have no potential conflicting interests with respect to the research, authorship, or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Ethics approval and consent to participate
The institutional review board in our hospital approved this case study and gave the consent to participate. Consent for publication was obtained from the patient.



