-
PDF
- Split View
-
Views
-
Cite
Cite
Santiago A Endara, Gerardo A Dávalos, Ana G Finke, Veronica Ayala, Nelson A Montalvo, Santiago Munoz-Palomeque, Gabriel A Molina, Progressive dysphagia from an esophageal liposarcoma, a complex problem in a challenging setting, Journal of Surgical Case Reports, Volume 2024, Issue 10, October 2024, rjae670, https://doi.org/10.1093/jscr/rjae670
Close - Share Icon Share
Abstract
Esophageal lipomatous tumors are extremely rare, and due to their nonspecific clinical manifestations, distinguishing them is nearly impossible without the aid of histopathology, immunohistochemistry, and molecular analysis. Complete resection with clear margins is the treatment of choice to avert metastasis, improve prognosis, and prevent complex complications due to the polyp growth and location. We present the case of a 70-year-old male who presented in 2023 with dysphagia due to an esophageal polyp; surgery was recommended. However, he did not accept any treatment due to fear. One year later, and since his symptoms worsened, he finally decided to undergo endoscopic treatment at another medical institution. However, during that procedure, he suffered severe asphyxia, which caused a cardiopulmonary arrest. Once he partially recovered and because he continued with dysphagia, surgery was completed, and the polyp was removed. The final diagnosis was esophageal liposarcoma.
Introduction
Liposarcoma is one of the most frequent soft tissue sarcomas in adults, and it usually appears in the retroperitoneum, trunk, and lower extremities [1]. These tumors rarely affect the gastrointestinal tract and, even more infrequently, the esophagus [2, 3]. Esophageal liposarcomas is an extremely rare tumor (0.1%–5.8%) that grows as a polypoid mass within the esophagus and is usually asymptomatic until it reaches a large size or invades surrounding tissues [3]. Due to its rarity, its management and definitive treatment are still under research [1].
We present the case of a 70-year-old male who presented with dysphagia and weight loss due to an esophageal polyp. Surgery was recommended, but he refused this treatment; as his symptoms became severe, he sought an endoscopic procedure to remove the polyp. During that procedure, and before the polyp could be removed, he experienced severe asphyxia that led to a cardiopulmonary arrest and neurological sequelae. Since his polyp was not removed, his dysphagia continued to worsen. Once he partially recovered, surgery was completed, and the polyp was resected. Esophageal liposarcoma was the final diagnosis.
Case report
The patient is a 70-year-old male with a past medical history of prostate cancer. He presented with a two-year history of progressive dysphagia. At first, he complained of epigastric pain, nausea, and vomits. In the last three months, he found it increasingly difficult to eat anything solid, until he found it impossible to swallow. Due to this, an upper endoscopy and a contrast-enhanced chest computed tomography (CT) were done at that time, revealing a giant superior esophageal polyp (Fig. 1) 28 cm away from the dental arcade; therefore, surgical resection was recommended. Nonetheless, the patient refused any surgical management.
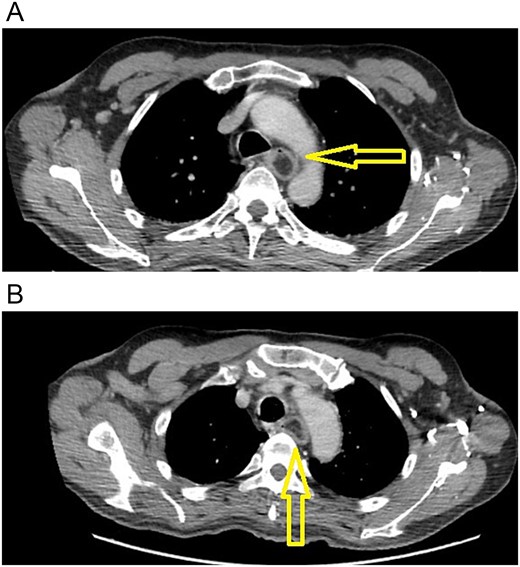
(A) CT scan: esophageal polyp is seen in the esophageal lumen. (B) CT scan: esophageal polyp completely obstructs but does not invade the esophagus.
One month later, as he was experiencing severe weight loss, he went to another medical center, where an endoscopic resection was offered. The patient and his family could not give us a complete record about what happened; yet, we know that during the initial part of the endoscopy, the patient suffered a sudden cardiorespiratory arrest, which was reversed. Afterward, he was transferred to an Intensive Care Unit and diagnosed with hypoxic–ischemic encephalopathy. During his stay, he remained unresponsive; therefore, a tracheostomy and an open gastrostomy were placed at that time to allow the patient to breathe and eat.
He partially recovered from the hemiplegia and neurologic sequelae, but he became completely care dependent. One thing that worsened during this time was his dysphagia; he did not have any neurogenic dysphagia; nevertheless, he was unable to drink anything, and it became so severe that he was unable to swallow saliva. Therefore, one year later, he presented to our office. A new endoscopy revealed that the giant polyp completely obstructed the lumen of the esophagus, and a new chest CT showed that the polyp grew but did not invade any surrounding structures (Fig. 2).
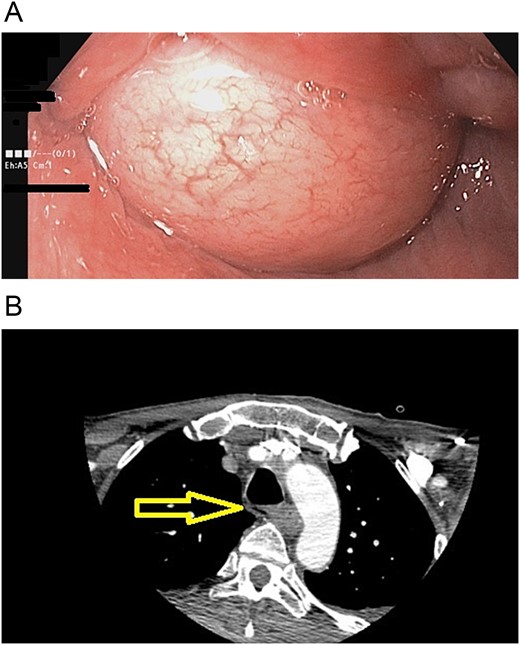
(A) Endoscopy, the polyp obstructs the esophagus's lumen. (B) CT scan: esophageal polyp size has increased in size over a year.
Upon admission, the patient was alert and partially obeyed motor commands. The patient had a tracheostomy and gastrostomy and was severely malnourished. (BMI was 17 kg/m2, and prealbumin levels were below 8 ml/dl) He was admitted to the hospital to improve his nutritional condition with supplements, and once the patient was in a more suitable condition, surgery was decided.
We performed an upper endoscopy that showed that the pedicle of the polyp was located on the right wall of the esophagus. Therefore, a cervicotomy was done. We then continued with the dissection and identified the mass in the esophagus. The 14 × 3 cm polyp was multilobulated, with a broad base that extended to the right pyriform sinus. Once the polyp was exposed through an esophagotomy, the resection was achieved using a 45-mm mechanical stapler (Ethicon, J&J New Jersey) and then reinforced with a 4–0 absorbable suture. Esophageal reconstruction was performed using another 4–0 absorbable suture (Ethicon, J&J New Jersey), and the esophagectomy suture line was reinforced with an omohyoid muscle flap. A drain was placed afterward, and the surgery was completed without complications (Fig. 3). A transoperative endoscopy revealed an intact larynx and no air leakage following the procedure.

(a) The polyp is seen being removed from the esophagus. (b) The complete 14 × 3-cm multilobulated esophageal polyp.
Pathology revealed a 14 × 3 cm grade 1, well-differentiated giant liposarcoma with an architectural pattern similar to the fibrovascular polyp of the esophagus. Its margins were free of tumor invasion, and no compromised lymph nodes were involved. pTNM staging was pT1, pN0, M0.
The patient had a favorable postoperative course and could finally swallow and drink liquids. A wound seroma was identified on the fifth postoperative day, which then revealed a surgical site infection that was successfully treated with open drainage, antibiotics, and a vacuum-assisted closure system. This improved the patient’s condition, and he was discharged without complications. The patient has drastically improved his nutritional status, and one year after his last surgery, he is feeling well and is undergoing regular follow-ups with periodic endoscopies.
Discussion
Esophageal lipomatous tumors are extremely rare tumors that account for less than 1% of all esophageal neoplasms [1, 2]. They tend to affect adult patients (median age 60–65 years) with a 2:1 male-to-female predominance [2]. Esophageal liposarcoma is an even rarer tumor (incidence of 0.1% to 5.8%) and since its first publication in 1983 by Mansour et al., less than 100 cases have been published in the English literature (Table 1) [1, 3]. This malignant tumor has many histopathological subtypes, from the most common variant, the well-differentiated type (68%), to the even rarer myxoid, dedifferentiated, and pleomorphic [2, 3].
| Authors . | Year . | Age . | Sex . | Size . | Main symptoms . | Management . |
|---|---|---|---|---|---|---|
| Ameet Kumar et al. | 2024 | 74 | Male | 25 cm | Dysphagia | Open approach |
| Theodore D. Liakakos et al. | 2006 | 72 | Male | 5 cm | Dysphagia | Open approach |
| Qingjiao Li et al. | 2023 | 46 | Male | 35 cm | Dysphagia | Open approach |
| Elzbieta Czekajska-Chehab et al. | 2009 | 56 | Female | 13 cm | Dyspnea | Open approach |
| G. B. Salis et al. | 1988 | 73 | Male | 15 cm | Vomits | Open approach |
| G. Coppet et al. | 1991 | 68 | Male | 7 cm | Dysphagia | Open approach |
| Yang et al. | 2006 | 49 | Male | 8 cm | Weight loss | Open approach |
| Inku Yo et al. | 2013 | 44 | Male | 15 cm | Dysphagia | Endoscopic approach |
| Jie Zhang et al. | 2020 | 43 | Male | 20 cm | Foreign body sensation in the throat | Open approach |
| Zhi-Chao Lin et al. | 2015 | 51 | Male | 15 cm | Dysphagia | Open approach |
| Y. Annalisa Ng et al. | 2019 | 54 | Male | 14 cm | Exertional Dyspnea | Open approach |
| Mohammad Sadeghi Hasanabadi et al. | 2011 | 68 | Male | N/A | Hoarseness | Endoscopic approach |
| Bréhant Olivier et al. | 2003 | 70 | Male | 20 cm | Dysphagia | Endoscopic failed/open approach |
| Faizan Boghani et al. | 2023 | 61 | Woman | 5 cm | Dysphagia | Endoscopic approach |
| Tomohiro Okura et al. | 2022 | 66 | Male | 23 cm | Dysphagia | Open approach |
| Jae Joon Chung et al. | 2003 | 56 | Male | N/A | Dysphagia | Open approach |
| Maurice A. Smith et al. | 2010 | 38 | Male | 17 cm | Shortness of breath | Open approach |
| Authors . | Year . | Age . | Sex . | Size . | Main symptoms . | Management . |
|---|---|---|---|---|---|---|
| Ameet Kumar et al. | 2024 | 74 | Male | 25 cm | Dysphagia | Open approach |
| Theodore D. Liakakos et al. | 2006 | 72 | Male | 5 cm | Dysphagia | Open approach |
| Qingjiao Li et al. | 2023 | 46 | Male | 35 cm | Dysphagia | Open approach |
| Elzbieta Czekajska-Chehab et al. | 2009 | 56 | Female | 13 cm | Dyspnea | Open approach |
| G. B. Salis et al. | 1988 | 73 | Male | 15 cm | Vomits | Open approach |
| G. Coppet et al. | 1991 | 68 | Male | 7 cm | Dysphagia | Open approach |
| Yang et al. | 2006 | 49 | Male | 8 cm | Weight loss | Open approach |
| Inku Yo et al. | 2013 | 44 | Male | 15 cm | Dysphagia | Endoscopic approach |
| Jie Zhang et al. | 2020 | 43 | Male | 20 cm | Foreign body sensation in the throat | Open approach |
| Zhi-Chao Lin et al. | 2015 | 51 | Male | 15 cm | Dysphagia | Open approach |
| Y. Annalisa Ng et al. | 2019 | 54 | Male | 14 cm | Exertional Dyspnea | Open approach |
| Mohammad Sadeghi Hasanabadi et al. | 2011 | 68 | Male | N/A | Hoarseness | Endoscopic approach |
| Bréhant Olivier et al. | 2003 | 70 | Male | 20 cm | Dysphagia | Endoscopic failed/open approach |
| Faizan Boghani et al. | 2023 | 61 | Woman | 5 cm | Dysphagia | Endoscopic approach |
| Tomohiro Okura et al. | 2022 | 66 | Male | 23 cm | Dysphagia | Open approach |
| Jae Joon Chung et al. | 2003 | 56 | Male | N/A | Dysphagia | Open approach |
| Maurice A. Smith et al. | 2010 | 38 | Male | 17 cm | Shortness of breath | Open approach |
| Authors . | Year . | Age . | Sex . | Size . | Main symptoms . | Management . |
|---|---|---|---|---|---|---|
| Ameet Kumar et al. | 2024 | 74 | Male | 25 cm | Dysphagia | Open approach |
| Theodore D. Liakakos et al. | 2006 | 72 | Male | 5 cm | Dysphagia | Open approach |
| Qingjiao Li et al. | 2023 | 46 | Male | 35 cm | Dysphagia | Open approach |
| Elzbieta Czekajska-Chehab et al. | 2009 | 56 | Female | 13 cm | Dyspnea | Open approach |
| G. B. Salis et al. | 1988 | 73 | Male | 15 cm | Vomits | Open approach |
| G. Coppet et al. | 1991 | 68 | Male | 7 cm | Dysphagia | Open approach |
| Yang et al. | 2006 | 49 | Male | 8 cm | Weight loss | Open approach |
| Inku Yo et al. | 2013 | 44 | Male | 15 cm | Dysphagia | Endoscopic approach |
| Jie Zhang et al. | 2020 | 43 | Male | 20 cm | Foreign body sensation in the throat | Open approach |
| Zhi-Chao Lin et al. | 2015 | 51 | Male | 15 cm | Dysphagia | Open approach |
| Y. Annalisa Ng et al. | 2019 | 54 | Male | 14 cm | Exertional Dyspnea | Open approach |
| Mohammad Sadeghi Hasanabadi et al. | 2011 | 68 | Male | N/A | Hoarseness | Endoscopic approach |
| Bréhant Olivier et al. | 2003 | 70 | Male | 20 cm | Dysphagia | Endoscopic failed/open approach |
| Faizan Boghani et al. | 2023 | 61 | Woman | 5 cm | Dysphagia | Endoscopic approach |
| Tomohiro Okura et al. | 2022 | 66 | Male | 23 cm | Dysphagia | Open approach |
| Jae Joon Chung et al. | 2003 | 56 | Male | N/A | Dysphagia | Open approach |
| Maurice A. Smith et al. | 2010 | 38 | Male | 17 cm | Shortness of breath | Open approach |
| Authors . | Year . | Age . | Sex . | Size . | Main symptoms . | Management . |
|---|---|---|---|---|---|---|
| Ameet Kumar et al. | 2024 | 74 | Male | 25 cm | Dysphagia | Open approach |
| Theodore D. Liakakos et al. | 2006 | 72 | Male | 5 cm | Dysphagia | Open approach |
| Qingjiao Li et al. | 2023 | 46 | Male | 35 cm | Dysphagia | Open approach |
| Elzbieta Czekajska-Chehab et al. | 2009 | 56 | Female | 13 cm | Dyspnea | Open approach |
| G. B. Salis et al. | 1988 | 73 | Male | 15 cm | Vomits | Open approach |
| G. Coppet et al. | 1991 | 68 | Male | 7 cm | Dysphagia | Open approach |
| Yang et al. | 2006 | 49 | Male | 8 cm | Weight loss | Open approach |
| Inku Yo et al. | 2013 | 44 | Male | 15 cm | Dysphagia | Endoscopic approach |
| Jie Zhang et al. | 2020 | 43 | Male | 20 cm | Foreign body sensation in the throat | Open approach |
| Zhi-Chao Lin et al. | 2015 | 51 | Male | 15 cm | Dysphagia | Open approach |
| Y. Annalisa Ng et al. | 2019 | 54 | Male | 14 cm | Exertional Dyspnea | Open approach |
| Mohammad Sadeghi Hasanabadi et al. | 2011 | 68 | Male | N/A | Hoarseness | Endoscopic approach |
| Bréhant Olivier et al. | 2003 | 70 | Male | 20 cm | Dysphagia | Endoscopic failed/open approach |
| Faizan Boghani et al. | 2023 | 61 | Woman | 5 cm | Dysphagia | Endoscopic approach |
| Tomohiro Okura et al. | 2022 | 66 | Male | 23 cm | Dysphagia | Open approach |
| Jae Joon Chung et al. | 2003 | 56 | Male | N/A | Dysphagia | Open approach |
| Maurice A. Smith et al. | 2010 | 38 | Male | 17 cm | Shortness of breath | Open approach |
Symptoms will depend on the location and size of the tumor [1]. Since these tumors tend to appear more in the cervical esophagus (87%) [3]. Once the tumor reaches 4 cm, most patients will develop dysphagia, polyp regurgitation, throat discomfort, and hoarseness [1, 4]. If left unchecked, the tumor can obstruct the esophagus, causing weight loss and severe respiratory symptoms (that range from a mild cough to pneumonia, asphyxia, and even sudden death) [1, 3, 4], as happened to our patient.
Still, due to their indolent growth pattern, most small tumors will be completely asymptomatic and clinically silent; therefore, most are only found incidentally [2].
Most of these tumors are intraluminal, with a long, narrow pedicle attached to the esophagus [2]. The pedicle can be pretty mobile, allowing the polyp to reach the stomach or cause regurgitation. They can also appear as an intramural submucosal mass [2, 3].
The differential diagnosis is challenging based solely on clinical features and can be confused with fibrovascular polyps, fibrolipomas, and angiolipoma, among others [2–4]. Therefore, pathology will play a decisive role in differentiating liposarcoma, as they can be distinguished by their ring chromosomes and the amplification of the MDM2 gene locus through immunohistochemistry [1, 5]. This allows us to differentiate these tumors and avoid misdiagnosis, as happened to our patient.
Diagnosis is made via an upper gastrointestinal endoscopy, barium esophagogram, and CT [1, 5]. They usually reveal a pedunculated intraluminal mass [1, 2]. Surgery is the treatment of choice, and excision of these tumors will depend on symptoms at presentation and the location [3, 5]. Excision can be performed extraluminally through an esophagotomy or endoluminally through an endoscopic approach [1, 6]. Endoscopy has become the first-line approach, especially if the stalk is visible and a snare device can be used [7]. When the snare technique is not possible due to the risk of incomplete resection, endoscopic submucosal dissection is another alternative [7, 8]. Due to the condition of our patient and the size of the tumor, surgery was completed and the tumor was resected.
After resection, a careful histopathological assessment of the polyp and its resection margin are advised, since local recurrence can appear in up to 10% of the cases [8, 9].
Esophageal liposarcoma is an extremely rare disease that should always be considered when approaching a patient with an esophageal mass; definitive diagnosis will depend on pathology and immunohistochemistry. Resection through surgery or an endoscopic approach is of paramount importance to prevent severe complications as our patient suffered.
Conclusion
Esophageal liposarcoma is a rare tumor that should be in the differential in a patient with dysphagia and an esophageal mass. This case highlights the need for prompt treatment in these delicate scenarios. Time is of the essence in medicine, any delay or mistake can be lethal. It is our duty as healthcare professionals to provide all the options to our patients to avoid such severe complications as this one.
Conflict of interest statement
None declared.
Funding
None declared.



