-
PDF
- Split View
-
Views
-
Cite
Cite
Evan A Thomas, Adam S Harris, Peritoneal invagination hernia in the virgin abdomen, Journal of Surgical Case Reports, Volume 2024, Issue 10, October 2024, rjae666, https://doi.org/10.1093/jscr/rjae666
Close - Share Icon Share
Abstract
Hernias are a common cause of small bowel obstruction. Many different classifications of hernias exist, all differing by location throughout the abdomen and hernia contents. We present a case report that describes a unique hernia—a peritoneal invagination hernia—which may lead to small bowel obstruction. The peritoneal invagination hernia is a defect in the peritoneum, in this case located on the right anterolateral abdominal wall, allowing small bowel to enter and become incarcerated. In our patient, the peritoneal defect was circular with smooth, rolled borders. The defect contained intact peritoneum overlying intact transversalis fascia. The patient had no prior abdominal surgeries. This hernia differs by location and etiology from preperitoneal interparietal hernias, which are found in the inguinal and femoral regions. This case describes a newly characterized abdominal hernia which is hypothesized to be due to a prior intra-abdominal inflammatory process.
Introduction
Hernias are a common pathology seen in General Surgery and are the second most common cause of small bowel obstruction (SBO) in the United States, behind intra-abdominal adhesions. Abdominal hernias, by definition, are a protrusion of intra-abdominal contents through an abnormal opening. The three main classifications are internal, external and interparietal hernias, all of which are further subdivided based on different characteristics [1]. In this case report, we present a newly described hernia, referred to as a peritoneal invagination hernia, which led to small bowel incarceration and obstruction. The peritoneal lining of the abdomen formed a peritoneal invagination overlying intact transversalis fascia, which ultimately led to SBO. This unique hernia occurred anterior to the cecum on the right anterolateral abdominal wall in a patient with no prior surgical history.
Case report
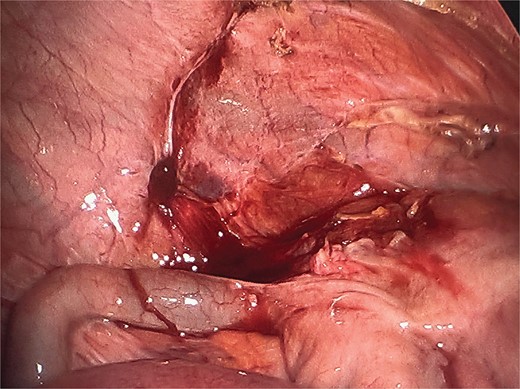
We present a case of an 88-year-old male with a past medical history significant for atrial fibrillation status post ablation taking Apixaban, coronary artery disease status post coronary stent, hypertension, hyperlipidemia, hypothyroidism, gastroesophageal reflux disease, benign prostatic hyperplasia, multiple myeloma and no prior abdominal surgeries who presented to the Emergency Department with severe abdominal pain for 2 days. He developed nausea and bilious emesis the day prior to presentation. He had not had a bowel movement in 4 days but was passing flatus. This was the first reported episode with these symptoms. Review of systems was negative for fever, chills, chest pain, or shortness of breath. CT scan showed mechanical, partial small bowel obstruction secondary to a transition point in the right lower quadrant with decompressed small bowel distally, fluid distended small bowel proximally, gastric distension with stool and gas in the colon. No portal venous gas, pneumatosis, free air, free fluid or mesenteric swirling was noted. Nasogastric tube decompression was performed with roughly 1 L bilious output. Gastrograffin small bowel follow-through performed after adequate decompression showed incomplete passage of contrast consistent with moderate to high grade SBO. The following day, the patient was taken to the operating room for diagnostic laparoscopy, revealing a loop of small bowel protruding into the abdominal wall slightly anterior to the cecum. The bowel was gently reduced with traction and appeared indurated but viable. Upon further inspection, there were adhesions tethering the cecum to the abdominal side wall. Just anterior to these adhesions, the peritoneum appeared to invaginate, creating a pocket with intact peritoneum at its base (Fig. 1) where the small bowel entered causing the SBO. The transversalis fascia was intact. Using the HARMONIC scalpel device, the cecum was carefully freed from the abdominal wall and the peritoneal pocket was incised in an oblique manner, establishing normal anatomy (Fig. 2). The appendix appeared grossly normal. The bowel was run from the terminal ileum to the ligament of Treitz – no other abnormalities were identified. The incarcerated portion of small bowel was reevaluated and was viable. Postoperatively, the patient had near immediate return of bowel function. The nasogastric tube was removed, and diet was advanced appropriately. He was discharged home in stable condition on postoperative Day 2 and has remained without complication since discharge.
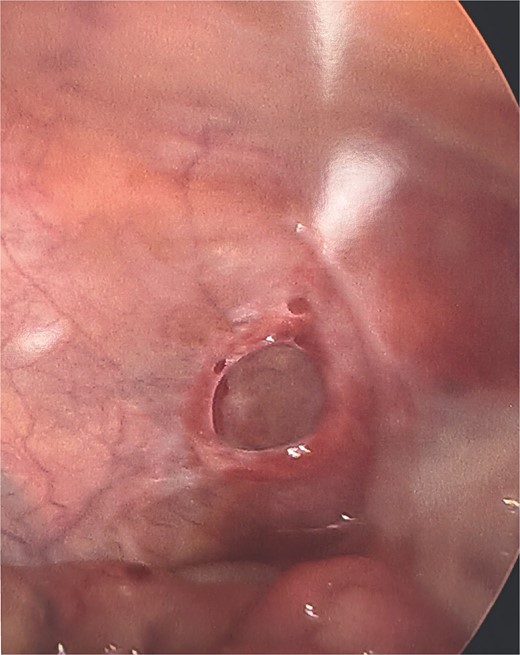
Intact peritoneum at the base of the peritoneal invagination hernia after incising the peritoneum.
Discussion
A peritoneal invagination hernia is distinct from all hernias previously described in the surgical literature. Hernias are classified and subdivided into three main groups - internal, external, and interparietal hernias. Internal hernias are those isolated to the peritoneal cavity. External hernias protrude through all layers of the abdominal wall. Interparietal hernias are hernias that protrude into specific layers of the abdominal wall [2]. Interparietal hernias are further classified into superficial, interstitial and preperitoneal. Superficial interparietal hernias are located between the external oblique and skin. Interstitial interparietal hernias are located between the transversalis fascia and transversus abdominis, internal oblique or external oblique muscles. Preperitoneal interparietal hernias are located between the peritoneum and transversalis fascia [3].
The preperitoneal interparietal hernia, a rare entity, is most closely related to the peritoneal invagination hernia. Interparietal hernias make up only 0.01%–1.6% of all hernias, with the preperitoneal subtype making up 20% of that number [3]. Lower et al. were some of the first to describe and publish case reports of interparietal hernias. The preperitoneal subtype has been seen in inguinal and femoral hernias [3], incisional hernias and after preperitoneal dissection during hernia repair with failure to close the peritoneum – known as peritoneal pocket hernias [4].
The location, anatomy and etiology of preperitoneal interparietal hernias differ from the case presented. There have been no case reports to date describing SBO secondary to a hernia formed by peritoneal invagination outside of the inguinal region or in a patient with no prior surgical history. This defect is, therefore, distinct from peritoneal pocket hernias and incisional hernias. In the case of the peritoneal invagination hernia, the peritoneum appears to invaginate but remain intact at its base, allowing for entrance of intra-abdominal contents. There is no defect present in the peritoneal lining and no transversalis fascia defect. This is a unique hernia with an unknown etiology but is hypothesized to be secondary to a prior intra-abdominal inflammatory process, given the finding of cecal adhesions to the lateral abdominal wall just posterior to the site of herniation.
The defect was addressed via laparoscopy, and the small bowel was reduced easily through manual traction using a laparoscopic grasper. The repair was simple and only required transection of the rolled edges of the peritoneal invagination using the HARMONIC scalpel. The peritoneum was observed to lay flat once the borders were transected. The base of the peritoneum and the transversalis fascia both remained intact; therefore, a formal hernia closure and repair was not necessary.
This case describes a peritoneal invagination hernia, a distinct variant of the preperitoneal interparietal hernia. The peritoneal defect led to small bowel herniation and obstruction, requiring operative repair in a patient with no prior abdominal surgical history or trauma. The peritoneal invagination was located just anterior to the cecum on the anterolateral abdominal wall. The cecum was adhered to the anterolateral abdominal wall posterior to the peritoneal invagination, prompting the suspicion of an inflammatory etiology. No formal hernia repair is required in the case of the peritoneal invagination hernia.
Conflict of interest statement
None declared.
Funding
None declared



