-
PDF
- Split View
-
Views
-
Cite
Cite
Ebunoluwa Ajadi, Julie Dueber, Reese W Randle, Cortney Y Lee, Unexpected arteriovenous malformation of the thyroid resulting in significant intraoperative blood loss, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa277, https://doi.org/10.1093/jscr/rjaa277
Close - Share Icon Share
Abstract
A 49-year-old morbidly obese woman with metastatic endometrial carcinoma was referred for evaluation of an incidentally identified large right thyroid nodule found on computed tomography performed for cancer evaluation. Ultrasound revealed a 9.7 cm solid isoechoic homogeneous right thyroid nodule. Fine needle aspiration was benign. Given size, resection was recommended following completion of chemotherapy and radiation. At the time of right thyroid lobectomy, extremely large vessels were encountered, and the procedure was complicated by estimated blood loss of 2 L. Final pathology revealed a large, benign adenomatous nodule and vascular features consistent with arteriovenous malformation (AVM). Unlike previously reported cases, the diagnosis of a thyroid AVM was not known preoperatively.
INTRODUCTION
Arteriovenous malformations (AVMs) are a subset of vascular anomalies characterized by abnormal communications between arteries and veins without an intervening capillary segment. These malformations are most often observed in the central nervous system but have been well described in other locations [1–3]. AVMs of the thyroid are rare—to date, only five cases have been reported. These lesions are commonly congenital, however, associations with cancer and other states marked by angiogenic stimulation have been highlighted [4, 5].
We highlight the case of a 49-year-old woman diagnosed with a thyroid AVM following surgery for a large goiter. Unlike previously described cases, this AVM was not identified before the operation. Also, in contrast to previously described cases, this patient lacked evidence of metastatic disease to the thyroid, an underlying angioproliferative disease state or a predisposing genetic condition. This case highlights the technical challenges that arise when performing a lobectomy in the setting of an unsuspected, nonembolized thyroid AVM.
CASE REPORT
A 48-year-old morbidly obese woman with a history of metastatic endometrial carcinoma who was status post-total abdominal hysterectomy and bilateral salpingo-oophorectomy presented for evaluation of a large right-sided goiter found incidentally on computed tomography (CT) performed as part of her metastatic cancer evaluation. CT revealed a 10 cm right thyroid mass with extension deep to the right clavicle and associated tracheal compression (Fig. 1). Positron emission tomography revealed no evidence of metastatic disease but displayed diffuse thyroid hypermetabolism.
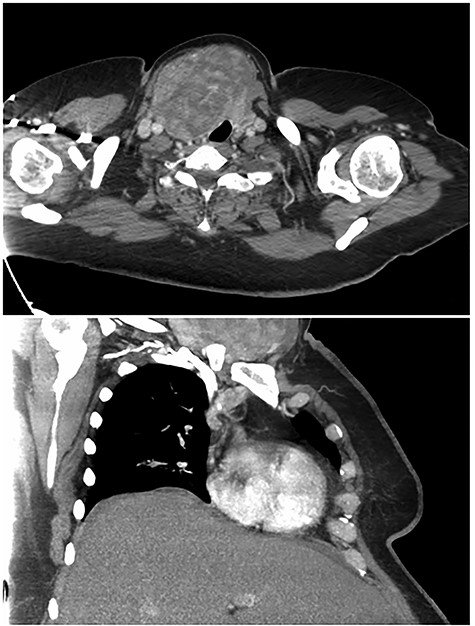
Preoperative computed tomography images highlighting large right thyroid nodule with tracheal compression.
At initial presentation, she was undergoing chemotherapy but recently discontinued one of the agents due to thrombocytopenia. Initial work-up included thyroid-stimulating hormone and free T4 which were within normal limits. A surgeon performed thyroid ultrasound revealed a large 8.9 × 5.0 × 9.7 cm solid, isoechoic, homogeneous nodule without calcifications encompassing the right thyroid lobe and extending into the substernal/subclavicular location (Fig. 2). Fine needle aspiration of the large nodule revealed colloid and follicular groups consistent with colloid nodule or goiter. Given the large size and associated decreased diagnostic accuracy as well as tracheal deviation, excision was recommended after completion of her course of chemotherapy.
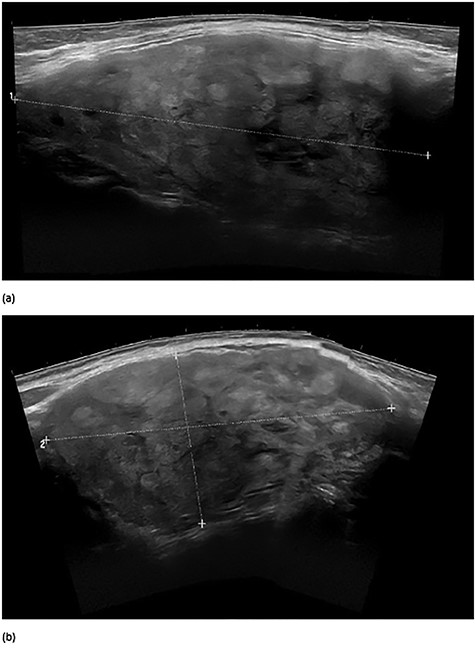
Preoperative surgeon performed right thyroid ultrasound images in longitudinal axis (a) and in transverse view (b). The large nodule measured 8.9 × 5.0 × 9.7 cm.
Approximately 7 months after the initial evaluation, the patient returned to clinic to discuss surgery since recent completion of chemotherapy. Repeat surgeon performed thyroid ultrasound revealed slight growth of the large right nodule, measuring 9.4 × 5.2 × 9.9 cm. Her platelets were 50 000.
An experienced, high-volume endocrine surgeon proceeded with right thyroid lobectomy using intraoperative nerve monitoring. On the morning of the case, her platelets were 62 000, an acceptable preoperative level per well-established preoperative guidelines [6, 7]. As the strap muscles were swept off the right thyroid lobe, extremely large vessels (approximately the size of normal internal jugular veins) were encountered coursing through the thyroid capsule. The middle thyroid vein was at least 1.5 cm in diameter and the superior thyroid artery measured >0.5 cm in diameter. Tedious dissection and mobilization of the lobe proceeded for 2 hours without blood loss. However, the nodule was not able to be elevated or delivered to expose the recurrent laryngeal nerve (RLN). The non-nodular isthmus was divided to allow for additional medial to lateral mobilization. On the first spread with the dissecting instrument in the (typically) avascular pretracheal plane, considerable bleeding was encountered. The isthmus was divided with the ultrasonic dissector, and direct pressure was applied. The bleeding originated from a high-pressure arterial tracheal perforator that was flush with the tracheal surface. There was no vessel or soft tissue to grasp/ligate, and the bleeding was too significant for electrocautery. A second faculty endocrine surgeon scrubbed to assist. Bleeding was slowed and hemostasis eventually achieved using multiple figure-of-eight prolene sutures on the tracheal surface. Bleeding from additional vessels in the thyroid bed and from the right lobe remained problematic but not high volume. The additional mobilization allowed for successful completion of the right thyroid lobectomy. While visual identification of the RLN is standard for the operating surgeon, identification was not possible due to the degree and pace of blood loss. A meticulous capsular dissection technique was used to prevent inadvertent injury to the unidentified RLN. Once the lobe was removed, the vagus nerve was identified and it stimulated appropriately, indicating appropriate RLN function.
Estimated blood loss was unprecedented at 2 L. Notably, all the bleeding encountered during the case was surgical in nature and all bleeding stopped following lobectomy (no concern for platelet-based oozing). The patient preemptively received a six-pack of platelets in the operating room when significant bleeding was encountered. The patient remained hemodynamically stable, requiring no other blood products. She recovered from surgery without incident.
Pathologic examination of the right thyroid lobe revealed a dominant adenomatous nodule with Hürthle cell and degenerative changes. A proliferation of large arterial and venous structures was seen predominantly at the periphery of the nodule and in the adjacent soft tissue (Fig. 3). The findings were consistent with an AVM. Consultation with an institutional expert on AVM syndromes resulted in recommendation for vascular imaging of the head and neck to evaluate for other possible associated AVMs. Follow-up imaging revealed no additional head or neck AVMs.
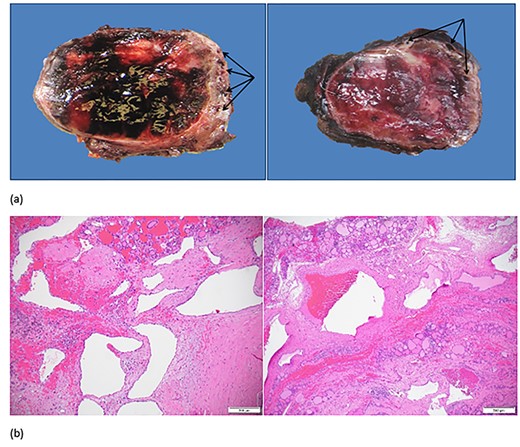
(a) Right thyroid gland with enlarged vessels (arrows) and hemorrhagic parenchyma on gross examination. (b) Large arterial and venous structures with background adenomatous and degenerative changes in the thyroid on microscopic examination.
DISCUSSION
This case highlights the intraoperative difficulty that exists when the diagnosis is not made on preoperative imaging and highlights the importance of obtaining the assistance of a second attending-level operating surgeon when unusual intraoperative challenges occur.
Thyroid surgery boasts overall favorable outcomes for patients with large nodules [8]. Although outcomes are overall favorable, previous studies have highlighted superior outcomes when performed by high-volume surgeons [9, 10]. The case was performed by an experienced, high-volume endocrine surgeon, who performs ~200 thyroid and parathyroid surgeries annually. Although the patient underwent an extensive work-up with standard imaging before surgery, her unusual vasculature could not be predicted. The patient’s morbid obesity, large nodule and complicated medical history would have made for a challenging case without the AVM and unexpected intraoperative bleeding. When difficult cases with unexpected, life-threatening intraoperative findings are encountered differences in outcome become driven by experience and technical ability—both of which result from large case volumes. This case provides an illustrative example.



