-
PDF
- Split View
-
Views
-
Cite
Cite
Emilie Joyeux, Anne-Sophie Gobenceaux, Théophile Hoyek, Patrick Dellinger, Paul Sagot, Intestinal malrotation complicated by an occlusive syndrome involving internal hernia in a pregnant woman, Journal of Surgical Case Reports, Volume 2016, Issue 7, July 2016, rjw113, https://doi.org/10.1093/jscr/rjw113
Close - Share Icon Share
Abstract
We present the case of a 33-year-old female who presented intestinal obstruction at the 7th month of pregnancy. She was complaining of abdominal pain with paroxysms, nausea and vomiting. When the symptoms worsened, we performed a CT-scan, which revealed suspected intestinal obstruction in a context of intestinal malrotation (IM). Conservative therapy failed and she required emergency laparotomy beginning with a caesarean section. The surgery revealed a peritoneal defect due to the IM through which the jejunum and ileum were incarcerated and strangulated. The incarcerated bowel was reduced and intestinal colour quickly returned to normal. Primary closure of the peritoneal defect was thus performed and the post-operative course was uneventful for the mother and the baby, who was admitted to the neonatal intensive care unit.
Obstruction syndromes in pregnant woman are rare, between 1 per 5000 and 1 per 66 000 [1]. The frequent causes are band adhesions (58%), volvulus (24%) and intestinal invagination (5%) [1]. Internal hernias account for 1% of occlusive syndromes; they are therefore extremely rare. In obstruction syndromes during pregnancy, maternal mortality is 6% and foetal mortality is 26% [1].
Clinical Case
We report the case of a pregnant patient at 32 WA. She had no surgical history and presented with paroxysmal periumbilical abdominal pain, accompanied by nausea and vomiting. The abdomen was tender overall with reduced bowel sounds. The uterus was contractile with a closed cervix. Foetal heart rate was variable oscille. Biological examinations showed leucocytes at 17 040 and C-reactive protein at 9.2. Urine cytology examinations and the vaginal swab were sterile.
The patient was treated with tocolysis with parenteral nicardipine, corticotherapy with intramuscular betamethasone and anti-biotherapy with amoxicillin and gentamicine. The digestive symptoms worsened over the following 48 hours with the absence of stools or gas emissions and refractory faecal vomiting.
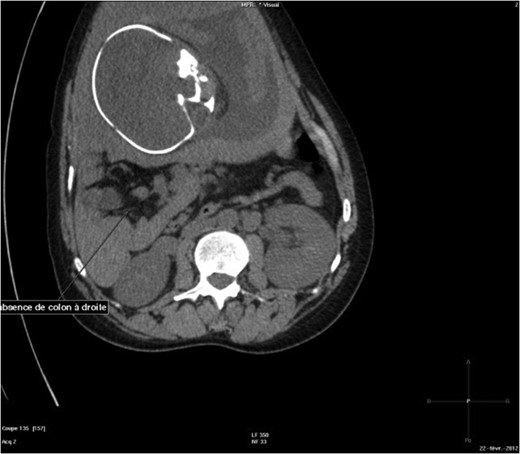
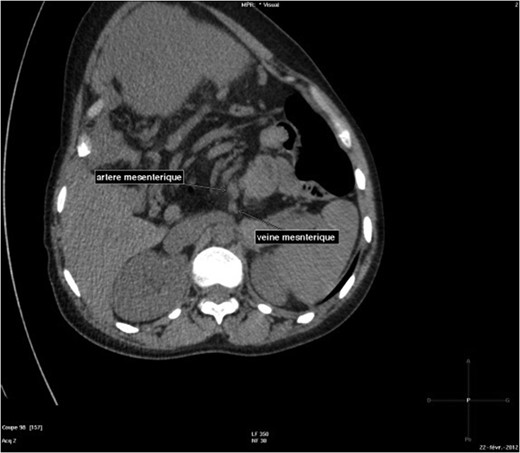
The abdominal-pelvic CT-scan showed a pre-splenic left position of the caecum and right colon, with no part of the colon on the right. The radiologist concluded that the patient was suffering from a complication of intestinal malrotation (IM) (Figs 1, 2, 3).

Abdominal-Pelvic CT-scan, non-contrast enhanced, in the sagittal plan, tenth dorsal vertebra level.
Abdominal-Pelvic CT-scan, non-contrast enhanced, in the sagittal plan, eleventh dorsal vertebra level.
Abdominal-pelvic CT-scan, non-contrast enhanced, in the sagittal plane.
Emergency median laparotomy was performed with extraction of the foetus using caesarean section. Exploration revealed incomplete IM and Ladd's bands with internal hernia of the whole small intestine. Treatment of the hernia consisted in extracting the small intestine from the hernial sac, and then resection of the hernial sac by electrocoagulation followed by repositioning of the intestines. There were no post-surgery complications for either the mother or the infant.
Discussion
Cases of obstruction syndromes during pregnancy are rare and a major difficulty in such cases is diagnosis. The risks of obstruction increase from 16 to 24 WA, with passage of the uterus to the abdominal-pelvic position at 36 WA, the descent of the foetus into the pelvis and in the post-partum period during uterine involution [2]. The more advanced into the pregnancy, the greater the risk of obstruction: 6% of obstructions occur during the first trimester, 27% during the second, 44% during the third and 21% post-partum [3]. The usual symptoms of obstruction can be confused with pregnancy-related pain. Other symptoms like the absence of stools and gas emissions, the intensity of the abdominal pain and refractory vomiting should alert the practitioner.
Two principal etiologies of obstruction stand out in our case and in cases in the literature: obstruction of the small intestine due to adhesions, and volvulus of the sigmoid (Tables 1 and 2). Among obstruction syndromes, the prognosis in volvulus of the sigmoid is more severe, with numerous foetal deaths, necrosis of the sigmoid, often two-step surgery (colostomy) and hospitalization in intensive care for severe sepsis [2, 4–6] (Table 2).
| Article . | Number of cases . | Term . | Type occlusion . | Treatment . | Maternal complications . | Outcomes foetus . |
|---|---|---|---|---|---|---|
| Meyerson et al. [4] | Nine cases | Second trimester = 4, 3eme trimester = 4, post-partum = 1 | Adhesion | Adhesiolysis | One case of intestinal necrosis | Three foetal deaths |
| Najih et al. [5] | Three cases | 17 WA | Adhesion | Adhesiolysis | _ | Vaginal delivery at term |
| 35 WA | Adhesion | Adhesiolysis | _ | Caesarean 35 WA | ||
| 35 WA | Adhesion | Adhesiolysis | _ | Caesarean 35 WA |
| Article . | Number of cases . | Term . | Type occlusion . | Treatment . | Maternal complications . | Outcomes foetus . |
|---|---|---|---|---|---|---|
| Meyerson et al. [4] | Nine cases | Second trimester = 4, 3eme trimester = 4, post-partum = 1 | Adhesion | Adhesiolysis | One case of intestinal necrosis | Three foetal deaths |
| Najih et al. [5] | Three cases | 17 WA | Adhesion | Adhesiolysis | _ | Vaginal delivery at term |
| 35 WA | Adhesion | Adhesiolysis | _ | Caesarean 35 WA | ||
| 35 WA | Adhesion | Adhesiolysis | _ | Caesarean 35 WA |
| Article . | Number of cases . | Term . | Type occlusion . | Treatment . | Maternal complications . | Outcomes foetus . |
|---|---|---|---|---|---|---|
| Meyerson et al. [4] | Nine cases | Second trimester = 4, 3eme trimester = 4, post-partum = 1 | Adhesion | Adhesiolysis | One case of intestinal necrosis | Three foetal deaths |
| Najih et al. [5] | Three cases | 17 WA | Adhesion | Adhesiolysis | _ | Vaginal delivery at term |
| 35 WA | Adhesion | Adhesiolysis | _ | Caesarean 35 WA | ||
| 35 WA | Adhesion | Adhesiolysis | _ | Caesarean 35 WA |
| Article . | Number of cases . | Term . | Type occlusion . | Treatment . | Maternal complications . | Outcomes foetus . |
|---|---|---|---|---|---|---|
| Meyerson et al. [4] | Nine cases | Second trimester = 4, 3eme trimester = 4, post-partum = 1 | Adhesion | Adhesiolysis | One case of intestinal necrosis | Three foetal deaths |
| Najih et al. [5] | Three cases | 17 WA | Adhesion | Adhesiolysis | _ | Vaginal delivery at term |
| 35 WA | Adhesion | Adhesiolysis | _ | Caesarean 35 WA | ||
| 35 WA | Adhesion | Adhesiolysis | _ | Caesarean 35 WA |
| Article . | Number of cases . | Term . | Type of occlusion . | Treatment . | Maternal complications . | Outcomes foetus . |
|---|---|---|---|---|---|---|
| Narjis [3] | One case | 24 WA | Volvulus of the sigmoid | Resection of the sigmoid and colostomy | Necrosis of the sigmoid | In utero foetal death at 24 WA |
| Kolusari et al. [2] | Four cases | 7 WA, 31 WA, 32 WA, post-partum | Volvulus of the sigmoid | Resection of the sigmoid with colostomy, and anastomosis in the case at 7 WA | One death, four cases of necrosis of the sigmoid | In utero foetal death at 31 WA |
| Ribeiro Nascimento et al. [10] | One case | 33 WA | Volvulus of the sigmoid | Left colectomy and colostomy | Peritonitis with septic shock following necrosis of the sigmoid + haemorrhage of the after birth with hysterectomy for haemostasis | In utero foetal death, Caesarean à 33 WA |
| Khan and Rehman [6] | One case | 30 WA | Volvulus of the sigmoid | Colectomy and ileostomy | Maternal death due to necrosis of the sigmoid and post-operative septic shock | In utero foetal death at 30 WA |
| Najih et al. [5] | Two cases | 16 WA | Tumour of the colon | Colostomy | _ | Caesarean at 40 WA |
| 37 WA | Volvulus of the sigmoid | Resection of the sigmoid and double ostomy | Necrosis of the sigmoid | In utero foetal death |
| Article . | Number of cases . | Term . | Type of occlusion . | Treatment . | Maternal complications . | Outcomes foetus . |
|---|---|---|---|---|---|---|
| Narjis [3] | One case | 24 WA | Volvulus of the sigmoid | Resection of the sigmoid and colostomy | Necrosis of the sigmoid | In utero foetal death at 24 WA |
| Kolusari et al. [2] | Four cases | 7 WA, 31 WA, 32 WA, post-partum | Volvulus of the sigmoid | Resection of the sigmoid with colostomy, and anastomosis in the case at 7 WA | One death, four cases of necrosis of the sigmoid | In utero foetal death at 31 WA |
| Ribeiro Nascimento et al. [10] | One case | 33 WA | Volvulus of the sigmoid | Left colectomy and colostomy | Peritonitis with septic shock following necrosis of the sigmoid + haemorrhage of the after birth with hysterectomy for haemostasis | In utero foetal death, Caesarean à 33 WA |
| Khan and Rehman [6] | One case | 30 WA | Volvulus of the sigmoid | Colectomy and ileostomy | Maternal death due to necrosis of the sigmoid and post-operative septic shock | In utero foetal death at 30 WA |
| Najih et al. [5] | Two cases | 16 WA | Tumour of the colon | Colostomy | _ | Caesarean at 40 WA |
| 37 WA | Volvulus of the sigmoid | Resection of the sigmoid and double ostomy | Necrosis of the sigmoid | In utero foetal death |
| Article . | Number of cases . | Term . | Type of occlusion . | Treatment . | Maternal complications . | Outcomes foetus . |
|---|---|---|---|---|---|---|
| Narjis [3] | One case | 24 WA | Volvulus of the sigmoid | Resection of the sigmoid and colostomy | Necrosis of the sigmoid | In utero foetal death at 24 WA |
| Kolusari et al. [2] | Four cases | 7 WA, 31 WA, 32 WA, post-partum | Volvulus of the sigmoid | Resection of the sigmoid with colostomy, and anastomosis in the case at 7 WA | One death, four cases of necrosis of the sigmoid | In utero foetal death at 31 WA |
| Ribeiro Nascimento et al. [10] | One case | 33 WA | Volvulus of the sigmoid | Left colectomy and colostomy | Peritonitis with septic shock following necrosis of the sigmoid + haemorrhage of the after birth with hysterectomy for haemostasis | In utero foetal death, Caesarean à 33 WA |
| Khan and Rehman [6] | One case | 30 WA | Volvulus of the sigmoid | Colectomy and ileostomy | Maternal death due to necrosis of the sigmoid and post-operative septic shock | In utero foetal death at 30 WA |
| Najih et al. [5] | Two cases | 16 WA | Tumour of the colon | Colostomy | _ | Caesarean at 40 WA |
| 37 WA | Volvulus of the sigmoid | Resection of the sigmoid and double ostomy | Necrosis of the sigmoid | In utero foetal death |
| Article . | Number of cases . | Term . | Type of occlusion . | Treatment . | Maternal complications . | Outcomes foetus . |
|---|---|---|---|---|---|---|
| Narjis [3] | One case | 24 WA | Volvulus of the sigmoid | Resection of the sigmoid and colostomy | Necrosis of the sigmoid | In utero foetal death at 24 WA |
| Kolusari et al. [2] | Four cases | 7 WA, 31 WA, 32 WA, post-partum | Volvulus of the sigmoid | Resection of the sigmoid with colostomy, and anastomosis in the case at 7 WA | One death, four cases of necrosis of the sigmoid | In utero foetal death at 31 WA |
| Ribeiro Nascimento et al. [10] | One case | 33 WA | Volvulus of the sigmoid | Left colectomy and colostomy | Peritonitis with septic shock following necrosis of the sigmoid + haemorrhage of the after birth with hysterectomy for haemostasis | In utero foetal death, Caesarean à 33 WA |
| Khan and Rehman [6] | One case | 30 WA | Volvulus of the sigmoid | Colectomy and ileostomy | Maternal death due to necrosis of the sigmoid and post-operative septic shock | In utero foetal death at 30 WA |
| Najih et al. [5] | Two cases | 16 WA | Tumour of the colon | Colostomy | _ | Caesarean at 40 WA |
| 37 WA | Volvulus of the sigmoid | Resection of the sigmoid and double ostomy | Necrosis of the sigmoid | In utero foetal death |
In our patient, it was an exceptional case of internal hernia in a context of IM. IM is an embryonic malformation due to the interruption of normal rotation of the primitive gut tube at 90° in the 4th week. The small intestine is therefore on the right and the colon in its entirety is on the left. It is extremely rare to discover IM in an adult: 0.2–0.5% of cases, in which the condition is asymptomatic and can be discovered on a volvulus of the small intestine.
Abdominal-pelvic ultrasonography is the first-line diagnostic examination as it is harmless, it provides useful information (dilation or signs of intestinal ischaemia, intraperitoneal effusion) and it rules out differential diagnoses (appendicitis, ovarian torsion). It can also rule out intestinal obstruction with sensitivity of 89% and specificity of 100% [7]. The use of a plain abdominal X-ray could have been discussed to search for hydroaeric levels. However, given the advanced term and the normal findings of the first abdominal US-scan, a CT-scan seemed to be the most useful examination. The abdominal-pelvic CT-scan is the gold-standard in the exploration of obstruction syndromes and can be used if the expected benefits outweigh the risks of foetal irradiation [3, 8].
MRI is an interesting examination in the diagnosis of obstruction syndromes in pregnant woman, because no ionizing radiation is used [9]. MRI, however, is still difficult to obtain in an emergency.
In our case, the obstruction was situated in the small intestine, in a hernial sac. The aetiology of IM could have been suspected given the absence of a surgical history. The intestine was not ischaemic and the clinical context allowed foetal pulmonary maturation at 32 WA and maintenance of normal haemodynamics in the mother [2, 5] (Table 1).
In cases of sub-obstruction, medical treatment via a nasogastric tube and the perfusion of analgesics may make it possible to avoid surgery and reduce the risk of foetal prematurity. When the clinical picture is serious, this is often insufficient. Laparotomy is often unavoidable to save the mother, whatever the term, because the maternal-foetal prognosis depends on the speed of the surgery. Before 28 WA, the objective is to treat the obstruction while maintaining the pregnancy. Between 28 and 32 WA, the balance between the benefits and risk must be considered; the mother's clinical condition and the risks associated with induction of a highly premature delivery must be taken into account. From 32 WA onwards, extraction of the foetus before the digestive surgery must be considered whenever possible, after pulmonary maturation, depending on the clinical picture of the mother and foetus [10].
Obstruction syndromes in pregnant women are difficult to diagnose, and the difficulty increases with the term. Persistent symptoms after symptomatic treatment should raise the alarm. Plain abdominal X-ray and US-scans must be used in cases of doubt. The surgery, performed by a double team, must be done as soon as possible after the diagnosis to improve maternal-foetal survival and to diminish complications.
CONFLICT OF INTEREST STATEMENT
None declared.
References
- pregnancy
- abdominal pain
- computed tomography
- cesarean section
- color
- hernias
- infant
- neonatal intensive care units
- intestinal obstruction
- intestines
- laparotomy
- mothers
- surgical procedures, operative
- ileum
- jejunum
- peritoneum
- nausea and vomiting
- malrotation, congenital
- conservative treatment
- intestinal entrapment



