-
PDF
- Split View
-
Views
-
Cite
Cite
Patrick Diener, Anna M Zentner, Jan Mengers, Bassey Enodien, Humeral head split fracture after epileptic seizure – a case report, Journal of Surgical Case Reports, Volume 2025, Issue 7, July 2025, rjaf568, https://doi.org/10.1093/jscr/rjaf568
Close - Share Icon Share
Abstract
Fractures during epileptic seizures without direct trauma are rare but can result in severe musculoskeletal injuries. Generalized tonic–clonic seizures can lead to complex fractures. A 30-year-old male with a history of grand-mal epilepsy and autism was delivered to our emergency room. He sustained a dislocated, multi-fragmented proximal humerus fracture with a head-split component following an unobserved seizure episode. Initial imaging confirmed a 4-part AO/OTA 11C3.1 fracture. Open reduction and internal fixation with a locking plate were performed, and postoperative rehabilitation was initiated. Radiological follow-ups confirmed progressive healing, with the patient regaining full functionality within 6 months. This case highlights the importance of thorough musculoskeletal assessment following seizure episodes, even in the absence of reported trauma. Given the lifelong fracture risk in epilepsy patients, preventive strategies, including osteoporosis management and antiepileptic medication optimization, should be considered.
Introduction
Although rare, fractures may occur after an episode of seizures in the absence of direct trauma. Forceful muscular contractions resulting from convulsive seizures can cause various types of fractures and dislocations. Overall a seizure-related injury is 2–6 time greater than in the general population [1]. With 33% the shoulder is the most common joint or bone fractured, followed by thoracic and lumbar vertebrae (29%), the skull and jaw (8%), and the femoral neck (6%) [2].
Regarding age, children, adolescents, and older adults are especially at risk for such injuries [3–7]. The risk of seizure-related injuries, including fractures, is particularly high during puberty. Whitney et al. found that children initiating ASM therapy around puberty (ages 11–13) had a significantly higher incidence of non-traumatic fractures compared to non-epileptic controls, with the risk peaking during mid-puberty [3]. In adults, the risk of seizure-related injuries remains elevated but varies with age and duration of epilepsy. Persson et al. reported that adults with epilepsy, particularly those aged 45 years or older, have a higher risk of extremity fractures, with the risk being significantly higher in the first 2 years after diagnosis. Additionally, de Almeida Fischer et al. noted that younger adults with a longer duration of epilepsy and higher seizure severity scores had a greater occurrence of injuries [4, 5]. The risk of seizure-related injuries is notably high in older adults with epilepsy. But Lees et al. found that falls, rather than seizures per se, are the dominant influence in the pathogenesis of fractures in older patients with epilepsy [6, 7].
The reason behind an elevated prevalence of fractures in patients with epilepsy is threefold. First a lesser bone density because of the antiepileptic drugs as a general risk factor of fracture occurrence. This is the result of a decrease in serum vitamin D and calcium absorption [8, 9]. While the higher risk of a direct trauma and thus fracture during a seizure is obvious, there are atraumatic fractures as well. Around 25% of seizure related fractures had its cause in the seizure alone [10]. The mechanical stress exerted during a seizure episode, particularly in cases of generalized seizures, can lead to significant musculoskeletal injuries, challenging both the diagnosis and management of such cases. These cases are extremely rare and the reports are mostly about spine fractures [11, 12]. Lastly there is higher risk of injury depending on the seizure type, whereas generalized tonic–clonic and myoclonic seizures are at higher risk [13].
This background sets the stage for the following case report.
Case report
A 30-year-old male patient, who is fully dependent and in need of full-time nursing care, suffering from grand-mal epilepsy and autism was presented to our emergency department after an episode of clonic–tonic seizure. It was unclear if there was direct trauma or not.
Upon arrival at the emergency department the patient displayed clear signs of shoulder deformity accompanied by pain and restricted movement. Peripheral motor function and circulation were intact.
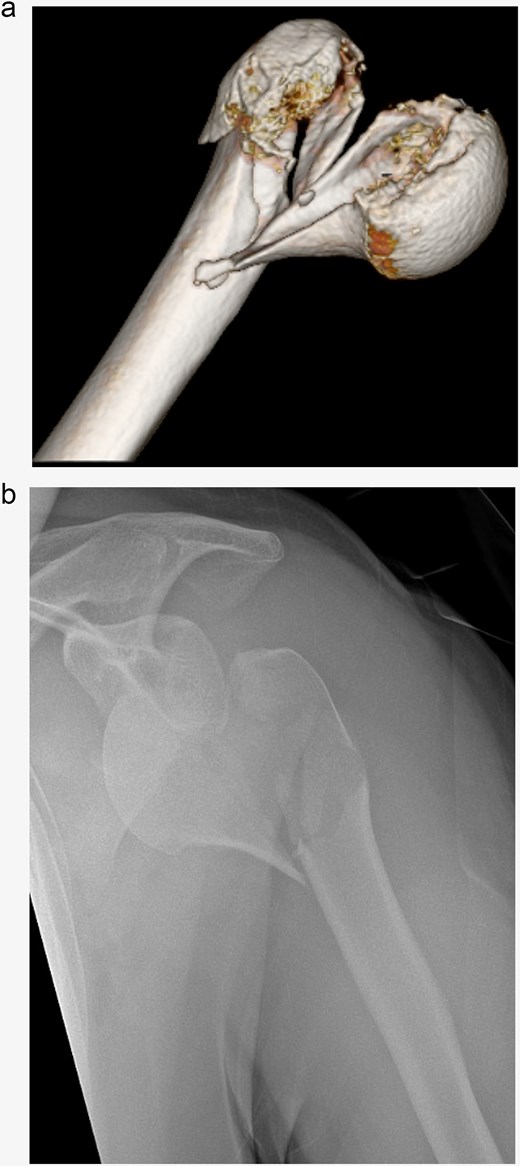
X-rays confirmed a dislocated 4-part proximal humerus fracture AO/OTA 11C3.1. The computer tomography scan demonstrated the presence of a Head-split component in the fracture (Fig. 1). Furthermore, it showed an anteroinferior dislocation of a larger articular surface-bearing fragment and avulsion of the greater tubercle. Neurological examination was intensified to ensure that the recent-onset epileptic seizure had not caused any neurological complications.
Open reduction and internal fixation with a locking plate was performed the following day. Following the deltopectoral approach, a reduction of the antero-inferiorly dislocated fragment through Kocher maneuvers and traction on the head fragment using a pointed reduction forceps were achieved. Subsequently, the head-split component was addressed by securing it with Ethibond sutures within the rotator cuff. The remaining fragments were then reduced and stabilized using a 5-hole anatomical locking compression plate along with a total of eight head and seven shaft screws, all performed under radiological guidance (Fig. 2).
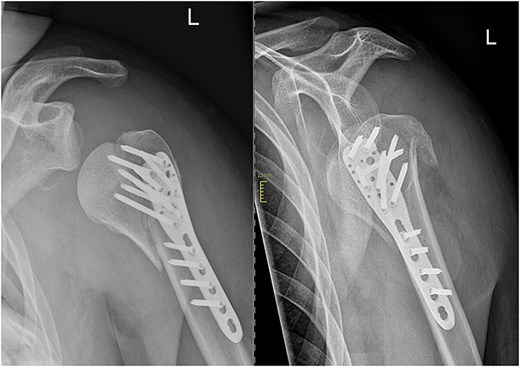
The initial postoperative therapy proceeded without complications and the patient was able to perform initial pendulum exercises under physiotherapeutically guidance. In the postoperative radiographic assessment of the fracture fragments exhibited an anatomically aligned position. However, it also showed a slight widening of the subacromial space. Antiepileptic therapy was again reviewed and adjusted in consultation with a neurologist to minimize the risk of future seizures.
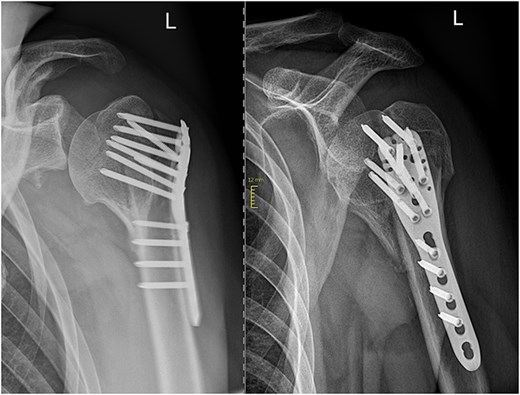
In subsequent clinical and radiological follow-ups at 2, 6, and 24 weeks postoperative, the humeral head depression showed regression, and the patient was able to progressively increase joint demands (Fig. 3). Training under physiotherapeutic supervision was difficult because of his secondary diagnoses. In the end after 6 Months he was unaffected in his daily living and painless.
Discussion
Seizure-related fractures are an uncommon yet significant complication in epilepsy patients, particularly when they occur without direct trauma. This case highlights the potential severity of musculoskeletal injuries resulting from generalized tonic–clonic seizures. The force of muscular contractions in convulsive seizures should not be underestimated and patients should be evaluated for severe fractures or dislocations after seizure episodes even without a direct trauma.
A major challenge in such cases is the initial diagnosis. And because these cases are extremely rare and research is scarce, a meticulous examination supported with radiological findings are needed in these cases [10, 13].
Patients with epilepsy are lifelong at risk for such injuries and thus need primary, secondary and tertiary prevention [1, 9, 13]. Especially regarding the treatment of osteoporosis [9]. There are recommendations for supplementation of vitamin D and calcium. Because of a lack of data, there are no such recommendations regarding bisphosphonate but the existing studies show a benefit of such a supplement [9]. There was no objectification regarding osteoporosis, and thus no prophylactic medication as mentioned above. But intraoperatively the bone quality was high.
Conclusion
This case underscores the importance of recognizing seizure-related fractures, even in the absence of direct trauma. This case highlights the need for comprehensive post-seizure assessments, especially in patients with limited communication abilities. Long-term strategies, including medication review and osteoporosis prevention, and an interdisciplinary collaboration are crucial in minimizing fracture risk and improving patient outcomes.
Conflict of interest statement
None declared.
Funding
None declared.



