-
PDF
- Split View
-
Views
-
Cite
Cite
Thomas E. Pennington, John Ozmen, Douglas Fenton-Lee, Torsion of omental fibrous pseudotumour mimicking acute appendicitis, Journal of Surgical Case Reports, Volume 2016, Issue 1, January 2016, rjv170, https://doi.org/10.1093/jscr/rjv170
Close - Share Icon Share
Abstract
Unusual pathologies are occasionally found at laparoscopy when appendicitis is suspected. We present a case of strangulated inflammatory fibrous pseudotumour of the omentum presenting in a similar fashion to appendicitis. The infarcted omentum was excised, facilitating prompt resolution of symptoms.
INTRODUCTION
Appendicitis is one of the few emergency abdominal presentations that may be diagnosed on clinical grounds alone. However, there is often some doubt as to the aetiology when symptomatology is not ‘classical’. While imaging modalities such as ultrasound and computed tomography may be helpful in confirming the diagnosis, they are sometimes not utilized if the diagnosis seems probable based on clinical grounds. Surgeons employing such a ‘selective’ approach may sometimes encounter different pathologies at operation, which can present challenging intraoperative management scenarios.
CASE REPORT
A 20-year-old woman presented to our institution with a 24-h history of right iliac fossa pain, fevers, leucocytosis (white cell count 11.3 × 109/l), and raised inflammatory marker (C-reactive protein 81.2 mg/l). On examination, there were signs of localized peritonitis at McBurney's point and in the suprapubic region. Gynaecological assessment was performed which excluded signs of pelvic inflammatory disease. There were no signs of urinary tract infection on mid-stream urinalysis. After obtaining the appropriate informed consent, the patient underwent diagnostic laparoscopy with a provisional diagnosis of acute appendicitis.
At operation, the appendix appeared macroscopically normal. On further examination, an inflammatory process was identified in the pelvis involving an omental inflammatory adhesion to the region of the distal sigmoid colon (Fig. 1a). The inflamed omentum was gently dissected off an adhered sigmoid appendix epiploica, which appeared secondarily inflamed (Fig. 1c). Once mobilized, the omentum demonstrated a thin projection that had torted and had subsequently become necrotic (Fig. 1b). The infarcted omentum was resected through the twisted omental ‘pedicle’ and delivered through the infra-umbilical port in an endoscopic retrieval bag (Endobag™ 5″ × 8″ Specimen Retrieval System, Covidien). Postoperative recovery was uneventful and the patient was discharged home day 1 postoperatively with complete resolution of symptoms.
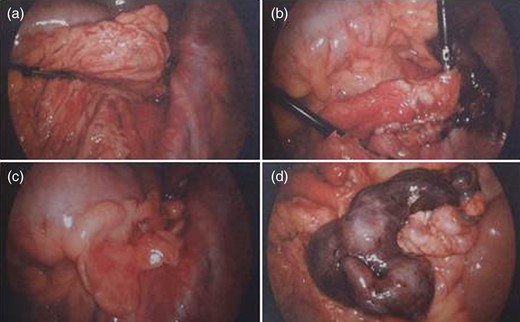
(a) Omentum adherent to sigmoid colon, (b) blunt dissection of inflamed omentum off underlying pathology, (c) sigmoid appendix epiploica appears secondarily inflamed and (d) underlying torted omentum displaying a sharp line of demarcation.
Histopathological examination revealed a necrotic piece of omentum containing several rounded, well-circumscribed, infarcted tumours. These tumours were hypocellular fibrous lesions with scattered chronic inflammatory cells and occasional neutrophils. There was no evidence of dysplasia or malignancy. These histological features are consistent with a fibrous pseudotumour of the omentum.
DISCUSSION
Fibrous pseudotumours are rare, benign masses arising in varied anatomical locations. They demonstrate dense hyalinized connective tissue interspersed with benign-appearing spindle cells and a variable, predominantly lymphoplasmacytic, infiltrate. When psammomatous or dystrophic calcifications are present, these tumours are referred to as calcifying fibrous pseudotumours [1]. It is postulated that these tumours may represent a late stage of inflammatory myofibroblastic tumour [2]. Fibrous pseudotumours have been reported to affect, among other sites, the tongue [3], scrotum [4], adrenal gland [5], extrahepatic bile ducts [6], stomach [7, 8], gallbladder [9] and omentum [10]. To our knowledge, this is the first report of omental fibrous pseudotumours presenting as an acute abdomen due to acute torsion and infarction. The present case highlights the varied intra-abdominal pathologies that may clinically mimic acute appendicitis and demonstrates the importance of the clinical acumen a surgeon must exhibit when dealing with unusual pathologies. The decision to proceed with definitive surgical excision of the infarcted omentum and the request for tissue diagnosis appeared to be reasonable management in this case.
CONFLICT OF INTEREST STATEMENT
T.E.P. has not received a research scholarship. The work has not been presented to a society or meeting before.



