-
PDF
- Split View
-
Views
-
Cite
Cite
Umit Gorkem, Tunay Efeturk, I. Tayfun Sahiner, Yılmaz Bas, Mete Dolapcı, Tayfun Gungor, A rare case of paratubal cystadenoma during pregnancy, Journal of Surgical Case Reports, Volume 2016, Issue 1, January 2016, rjv169, https://doi.org/10.1093/jscr/rjv169
Close - Share Icon Share
Abstract
Paratubal cysts (PTCs) are generally incidentally detected in pregnancy. However, paratubal cystadenomas in pregnant women are very rare cases who are reported individually. An unusually giant case of paratubal cystadenoma in a pregnant woman is presented here. A 27-year-old woman presented to our department for a routine pregnancy checkup. A giant cystic mass accompanying a 17-week gestation was detected on examination. During laparotomy, a huge right-sided PTC was resected. Histopathological evaluation revealed a benign cystadenoma originating in the ipsilateral paratubal space. PTCs are often denoted as being benign. Neoplastic transformation or malign potential will change the course of follow-up and the patients' prognosis. Treatment with surgical excision in the second trimester can safely prevent such associated adverse conditions. In conclusion, gynecologists should be careful for causes of adnexal masses in a woman with an intrauterine pregnancy. PTCs also tend to show accelerated growth patterns during pregnancy.
INTRODUCTION
Adnexal masses are detectable in ∼1–4% of all pregnancies [1, 2]. Among the causes of adnexal masses in pregnancy, paratubal cysts (PTC) are seen in <5% of cases [3]. PTCs derive from the broad ligament between the ovary and the fallopian tube [4]. They may be classified as either non-neoplastic simple cysts or cysts of neoplastic origin [5]. The simple PTCs are considered to originate from the mesothelium of embryonic remnants of the Müllerian and Wolffian duct, or from the invagination of the Fallopian tube's serosa [6]. Neoplastic PTCs like benign ovarian tumors (i.e. cystadenomas or cystadenofibromas) originate from the neoplastic transformation of a simple PTC or from adjacent ovarian tissue. We report here a rare case of paratubal cystadenoma in a 17-week pregnant woman.
CASE REPORT
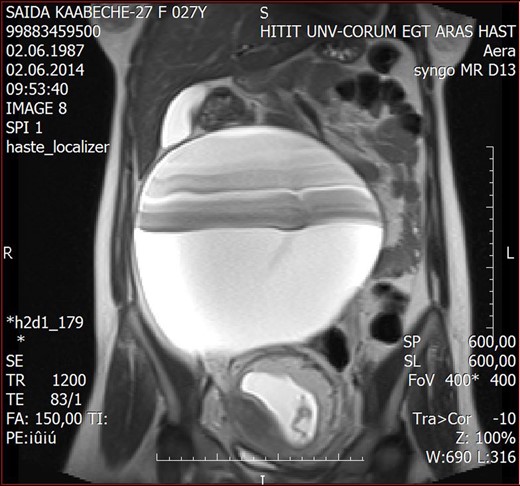
A 27-year-old female presented to the Hitit University Training Hospital for her routine pregnancy checkup. She was asymptomatic and was 17 weeks pregnant according to her last menstrual period. Her medical, surgical, and obstetric background was unremarkable, and she had considered her pregnancy up to this day unexceptional. On abdominal examination, a smooth painless mass arising from the right hemi-pelvis, extended up to a level just 10 cm above the umbilicus. An ultrasound scan confirmed the presence of a live 17-week gestation accompanied by an incidental cystic mass measuring ∼210 × 180 × 120 mm. Blood samples for serum tumor markers were drawn and the results were within normal limits (Ca-125: 8.6 U/ml, alpha-fetoprotein: 25.4 ng/ml). Magnetic resonance imaging (MRI) reported a 203 × 210 mm cystic mass, while all other pelvic structures were denoted as being within normal limits (Fig. 1).
To arrive at a definitive diagnosis, laparotomy was scheduled. Laparotomy was performed via a 15-cm midline incision. Upon entering the abdominal cavity, a small sample of intra-abdominal fluid (3 mL) was obtained and sent for cytological examination. Exploration of the pelvis revealed minimal abdominal liquor, a gravid uterus and a left-sided adnexia of normal morphology. However, the right adnexial area comprised a 220 × 200 × 100 mm smooth surfaced cystic mass, originating from the right mesosalpinx. The mass was independent of the right ovary and was connected to the right Fallopian tube with a pedincle ∼8 cm in length (Fig. 2). Following resection of the cyst, it was sent to our Department of Pathology for a frozen histology evaluation. Cytological examination of the intra-abdominal fluid ruled out malignancy, and the mass was reported as a giant PTC. The patient's postoperative follow-up was uneventful, yet close monitorization of the fetus was carried out to reassure the mother. The patient was later discharged from hospital 5 days after the procedure without any signs of maternal or fetal complication.

The smooth surfaced cystic mass, originating from the right mesosalpinx.
Definitive histopathological examination confirmed a paratubal cystadenoma of the right Fallopian tube (Fig. 3). The cystic mass involved the entirety of the right tube. The thick fibrocollagenized wall of the cystic mass, adjacent to the serosa of the tube, was lined with a single layer of ciliary columnar epithelium. Immunohistological examination revealed a p53-negative lining epithelium.
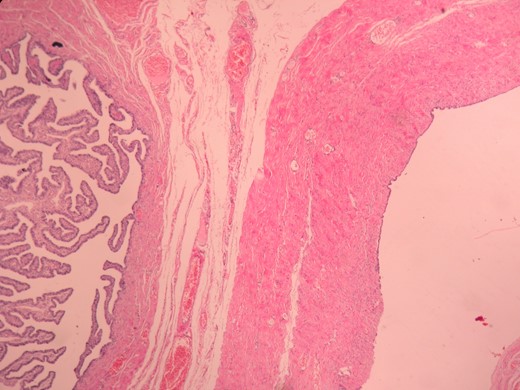
The thick fibrocollagenized wall of the cystic mass, lined with stratified and complex epithelium, H&E, ×200.
DISCUSSION
PTCs are generally asymptomatic, but they may rarely cause clinical conditions such as hemorrhage, torsion, rupture, infection or malignant transformation [7]. In 1909, the very earliest report of a pregnancy complicated by a PTC, described the excision of a torted PTC in an emergency setting. Histopathologically, PTCs are usually simple cysts. Neoplastic features of these cysts (i.e. cystadenomas) are so rare that they have previously been reported as individual case reports [8]. Differential diagnosis should include hydatid cysts of Morgagni and hydrosalpinx. Typically cystadenomas have a thick collagenized wall, and basically are lined with stratified and complex epithelium especially in focal areas [9]. PTCs are mostly 1–8 cm in diameter. It is emphasized that they may reach larger sizes under the influence of hormonal factors [7].
When deciding on an appropriate management and treatment plan, the nature of the mass is crucial. Small, unilocular, simple cysts are managed expectantly while persistent, thick-walled cysts involving papillary projections or masses showing signs of complications such as torsion or hemorrhagia are managed surgically. Surgery may be performed laparoscopically or via open surgery. The size of the mass may be a limiting factor for laparoscopic intervention. If elective surgery is considered, this should be performed after 14 weeks gestation to minimize obstetric complications, although this risk is minimal [10].
In conclusion, gynecologists should be careful for causes of adnexal masses in a woman with an intrauterine pregnancy, and should consider such cases in a multidisciplinary fashion. In this case, the patient was surgically evaluated in collaboration with our Department of General Surgery. The resection of a giant paratubal cystadenoma in the second trimester was undertaken without peroperative maternal or fetal complications and may have also prevented potential future obstetric dilemmas associated with rapid enlargement of the cyst.
If PTCs are correctly identified, and definitely discerned from ovarian lesions, they are often denoted as being benign. Hence, the patient is informed of a pelvic lesion with ‘mere importance’. In addition to the previously mentioned complications, acknowledgement of neoplastic transformation or malignant potential will definitely change the course of follow-up and the patients' prognosis. That PTCs tend to show accelerated growth patterns during pregnancy should be beared in mind and therefore should not be overlooked as insignificant lesions. This case is a unique demonstration for this feature.
CONFLICT OF INTEREST STATEMENT
None declared.



