-
PDF
- Split View
-
Views
-
Cite
Cite
Kathleen S. Beebe, Joseph A. Ippolito, Desmoplastic fibroma of the distal radius: an interesting case and a review of the literature and therapeutic implications, Journal of Surgical Case Reports, Volume 2016, Issue 1, January 2016, rjv171, https://doi.org/10.1093/jscr/rjv171
Close - Share Icon Share
Abstract
Desmoplastic fibromas are rare, benign, locally aggressive bone tumors, which arise primarily in patients younger than 30 years old. Historically, even with greater functional loss, en bloc or wide resection of the tumors to prevent local recurrence has been the method of choice in treatment. This article discusses the presentation of a 10-year-old male who presented with a mass in the distal forearm, after reporting difficulty in pronation and supination. The patient was ultimately treated with wide resection and allo-arthrodesis with allograft. Post-operatively, the patient has exhibited excellent recovery, including normal range of motion at the shoulder and elbow, and ability to perform all activities of daily livings despite reduced grip strength compared with the contralateral side.
INTRODUCTION
Desmoplastic fibromas are benign but locally aggressive bone tumors first described by Jaffe in 1958 [1]. Desmoplastic fibromas are quite rare, accounting for 0.06% of all bone tumors and 0.3% of benign bone tumors, typically in patients younger than 30 years, involving the metaphysis or diametaphysis of long bones in >50% of cases, with no reported cases of metastases in the literature [2–4]. Radiography of desmoplastic fibromas is typically lytic, expansile and well demarcated, with low signal intensity on both T1- and T2-weighted magnetic resonance imaging (MRI) [5]. En bloc or wide resection of the tumors to prevent local recurrence has historically been the method of choice for treatment [3]. Some recent case reports with limited follow-up duration have advocated use of curettage with adjunctive therapy and bone grafting rather than wide resection to minimize functional loss [6, 7]. However, recurrence rates following curettage, excision and wide resection have been shown to be 55, 72 and 17%, respectively [8]. The authors have obtained the guardian or patient's informed written consent for print and electronic publication of the case report.
CASE REPORT
A 10-year-old male was referred to our office after being seen by a pediatric orthopedic surgeon for a distal left forearm mass with block in pronation and supination. The patient's past medical history is significant for a distal radius fracture 2 years prior to his aforementioned office visit. Follow-up radiographs after fracture union at that time showed no evidence of disease (Fig. 1). Radiographs taken at the time of presentation 2 years after fracture healing revealed a 6.5 cm long lesion in the distal syndesmosis arising from the radius. The lesion resulted in pressure erosions upon the distal radius and ulna, causing a slight splaying of the bones (Fig. 2).
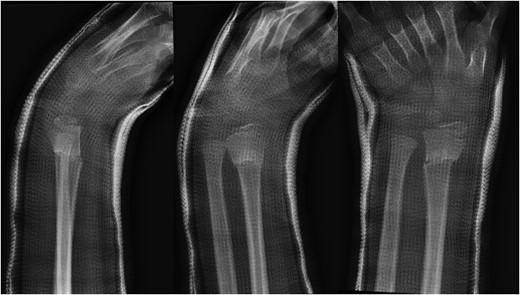
Lateral, oblique and anteroposterior (AP) views of distal radius fracture 2 years prior to presentation of desmoplastic fibroma.

AP and lateral radiographs of the left forearm showing 6.5 cm long lesion in the region of the distal syndesmosis between the radius and ulna.
The differential diagnosis included primary benign and malignant bone tumors, and thus preoperative staging studies were performed. A triple-phase bone scan was administered and demonstrated increased uptake in the distal shaft of the left radius and left ulna, as well as in the distal physis of the left radius (Fig. 3). Subsequently, acquired SPECT images demonstrated similar findings of increased uptake.
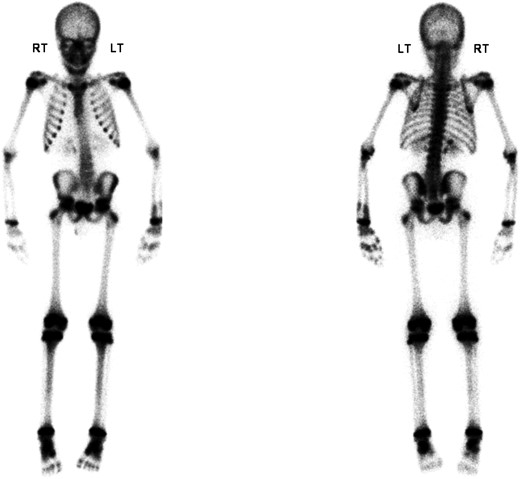
Triple-phase bone scan revealing moderately increased radiotracer uptake in the distal shaft of the left radius and left ulna, as well as in the distal physis of the left radius.
A MRI images revealed a large mass at the level of the distal radial and ulnar metadiaphyses, measuring ∼6 cm craniocaudad, 3.7 cm AP and 3 cm transverse (Fig. 4).
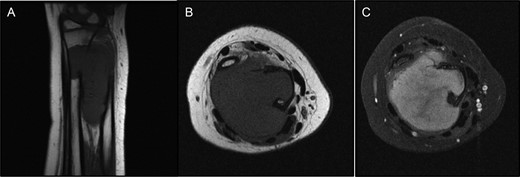
(A and B) T1 MRI showing mass iso-intense to muscle. (C) T2 MRI axial view with overall increased signal intensity, but with a central area of decreased signal.
After initial imaging, a fluoroscopy-guided biopsy was performed. Positive B-Catenin nuclear immunostaining, along with histology showing fibrous tissue, supported a diagnosis of desmoplastic fibroma.
Upon confirmation of desmoplastic fibroma, a discussion with the patient's mother was held, explaining the rarity of the tumor, and the likelihood that the patient would require radical resection to decrease risk of local recurrence, which would lead to a vast reduction in wrist motion. Additionally, as the tumor extended to the distal radius, resection of the joint surface would be necessary. Subsequently, a conversation about reconstructive options was held, including options for use of the fibula, allograft and allo-arthrodesis of the wrist joint. Ultimately, the patient's mother decided to pursue allo-arthrodesis with allograft, with plans to pursue future reconstruction with use of the fibula if this surgery was unsuccessful.
Upon removal of the mass, the distal halves of the right ulna and radius were resected. Dorsal plate fixation was used to stabilize the allograft, which extended from the native proximal radius to the proximal carpal row, effectively creating a single-bone forearm (Fig. 5).
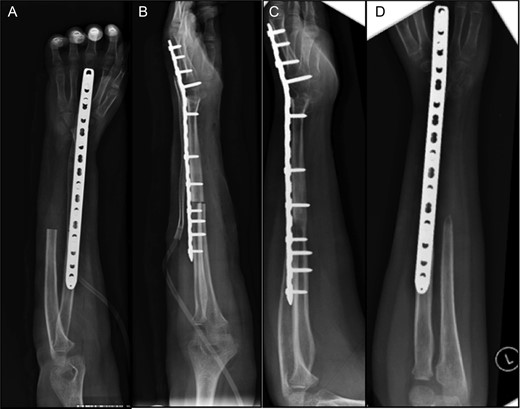
(A and B) Post-operative radiographs of allo-arthrodesis with dorsal plate fixation. (C and D) Follow-up radiographs at 7 months post-op.
Post-operatively, the patient began occupational therapy 1 week after surgery, completing 13 sessions over several months, with a progressive increase in strength, range of motion and coordination of the left upper extremity. At 8 weeks, the patient was able to employ pincer grasp to pick up small marbles and make a fist at 10 lbs of force, with minimal pain on palpation as well as during therapy exercises. At the request of the patient's family, they were given a hand-strengthening routine to continue at home. At 12 months follow-up, the patient has exhibited excellent recovery, including normal range of motion at the shoulder and elbow and ability to perform all activities of daily livings despite reduced grip strength. On all follow-up imaging, the allograft has fully incorporated, with no hardware failure or loosening.
DISCUSSION
Although some recent literature has explored the possibility of utilizing intralesional curettage with adjuvant therapy with the intention of sparing maximum limb function, the level of invasion of the tumor and thus increased risk of recurrence in this patient made radical resection a more favorable surgical option. In the largest review of desmoplastic fibroma cases to date, recurrence rates were 38% higher following curettage than radical resection, further strengthening a decision to pursue radical resection [8].
Muramatsu reported a case of a young man with desmoplastic fibroma of the distal radius treated successfully with excision of the radius and fibular graft, free of tumor for 7 years as per last reported follow-up, with good range of motion at elbow and wrist [9]. Kesani reported a case of a 15-year-old male with recurrent desmoplastic fibroma of the radius and ulna treated successfully with distal radius allograft with radiocarpal, partial intercarpal and third metacarpal capitate arthrodesis osteosynthesis to the proximal ulna [10]. In this particular case, the advantages of wide resection, including a substantial decrease in the rate of local recurrence, outweighed the drawbacks of the procedure, including reduced limb function. Factors such as tumor size and location, as well as age and activity of the patient, must be considered in each case. Previously, the senior author had a patient with a similar case which was treated with more conservative curettage several times, and ultimately required an above the elbow amputation to control extensive recurrent disease, fracture and hardware failure. This experience encouraged the author to advocate for more aggressive treatment on this patient's behalf. This case highlights the importance of extensive discussion with parents of the child and detailed follow-up with the surgeon and physical therapists to ensure maximal limb function recovery and monitoring for recurrence of disease.
CONFLICT OF INTEREST STATEMENT
None declared.



