-
PDF
- Split View
-
Views
-
Cite
Cite
Akiko Sakakibara, Hiroaki Suzuki, Atsuya Yamashita, Takumi Hasegawa, Tsutomu Minamikawa, Shungo Furudoi, Takahide Komori, Facial emphysema after sinus lift, Journal of Surgical Case Reports, Volume 2015, Issue 6, June 2015, rjv067, https://doi.org/10.1093/jscr/rjv067
Close - Share Icon Share
Abstract
An 80-year-old man with a history of en bloc resection of squamous cell carcinoma of the hard palate (T4aN0M0) was performed a lateral-window sinus lift of the edentulous area of the left maxillary molar region to facilitate future placement of dental implants.
Two hours after the surgery, the patient complained of sudden malar swelling. Marked swelling was present from the left infraorbital region to the buccal region. The swelling was associated with air pockets at the alar base and in the angulus oculi medialis region and subcutaneous malar tissue. Emphysema appeared after the patient blew his nose. Therefore, the mucous membrane of the maxillary sinus might have had a small hole, and air might have entered the subcutaneous tissue via the bone window when the air pressure in the maxillary sinus increased with nose blowing. It is important to advise patients to avoid increasing the intraoral pressure after sinus-lift procedure.
INTRODUCTION
Air-blowing equipment is often used in dentistry and oral surgery, and there are many reports of subcutaneous or mediastinal emphysema with the use of these machines. Furthermore, emphysema has been reported with jaw corrective surgery, injuries and alternating washes in root-canal therapy. However, there are no previous reports of subcutaneous emphysema after the maxillary sinus-lift procedure. Here, we report a case of malar subcutaneous emphysema after sinus lift.
CASE REPORT
An 80-year-old man with a history of en bloc resection of squamous cell carcinoma of the hard palate (T4aN0M0) complained of mastication difficulties due to the maxillary defect, and water and air leakage into the maxillary sinus. Maxillary segmentectomy included resection of the alveolar ridge from the left central incisor to the right pterygoid process of the sphenoid bone (Fig. 1). The resection site was reconstructed with a forearm flap, and the maxillary sinus was completely closed.
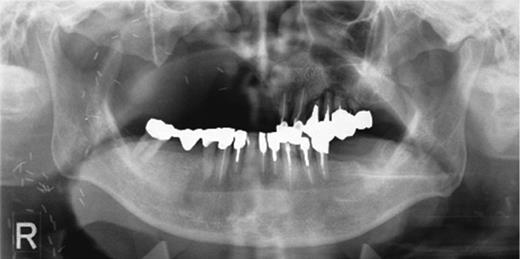
Preoperative orthopantomography. Molar teeth on the left side had been previously extracted because of severe periodontitis.
The patient used a jaw prosthesis with clasps over the remaining left maxillary teeth. However, these teeth were not strong enough to support a large jaw prosthesis that would cover the right maxillary defect, and residual teeth were missing. The patient sought implant treatment in the left maxillary molar region. However, computed tomography (CT) revealed that the bone mass of the left molar region was inadequate for implantation of these fixtures (Fig. 2). We performed the sinus-lift procedure under local anesthesia. The soft tissue from the canine region to the molar tooth region was incised and elevated to expose the underlying lateral wall of the left maxillary sinus. A 12 × 5 mm window was created in the bone of the maxillary sinus anterior wall with a piezoelectric instrument to expose the underlying Schneiderian membrane, which is the lining of the maxillary sinus cavity. Through careful instrumentation, the membrane was carefully peeled from the inner aspect of the sinus cavity (Fig. 3a). No damage to the membrane of the maxillary sinus was present. The newly formed space within the bony cavity of the sinus inferior to the intact membrane was grafted with artificial bone, and artificial bone was placed on the alveolar crest to raise the alveolar crest (Fig. 3b). The gingival flap was replaced and sutured to complete the sinus-lift procedure. There was minimal hemorrhage during the operation, and hemostasis was adequate. There was insignificant facial swelling immediately after the operation.
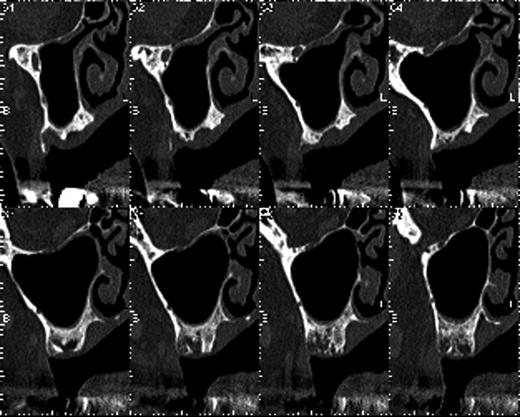
The bone mass in the left molar region was inadequate for implantation of fixtures.
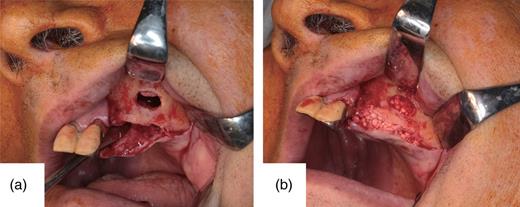
(a) The sinus cavity. A 12 × 5 mm section of bone has been removed at the maxillary sinus anterior wall with a piezoelectric instrument. There is no apparent damage of the membrane of the maxillary sinus. (b) Artificial bone has been grafted in the formed sinus cavity and placed on the alveolar bone.
Two hours after the surgery, the patient complained of sudden malar swelling (Fig. 4). Marked swelling was present from the left infraorbital region to the buccal region, and we suspected postoperative bleeding. Thus, we considered hemostasis treatment necessary and reopened the wound under local anesthesia. There were a few hematomas in the wound, but an apparent bleeding point was absent. We removed a hematoma and closed the wound. The CT images revealed that the artificial bone grafted inferior to the membrane had not leaked into the maxillary sinus, and there was no apparent damage of the maxillary sinus membrane. However, the marked malar swelling was associated with air pockets at the alar base and in the angulus oculi medialis region and subcutaneous malar tissue, and no hematoma was evident (Fig. 5a and b). We made a diagnosis of subcutaneous emphysema and administered an intravenous drip containing antibiotics to the patient for 3 days. The swelling improved day by day. We confirmed emphysematous improvement and the graft situation of the artificial bone on the CT images at 12 days postoperatively.

After sinus-lift surgery, marked swelling is obvious from the left buccal region to the angulus oculi medialis.
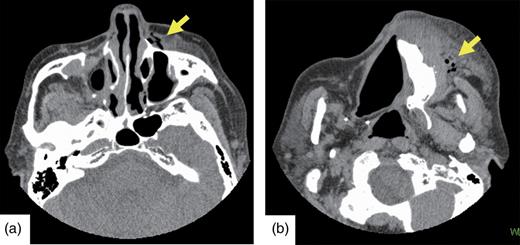
(a and b) Postoperative CT. Emphysema (indicated by arrows) is visible from the left buccal region to the angulus oculi medialis.
DISCUSSION
Emphysema of the maxillofacial region caused by dental treatment, oral surgical procedures or trauma is frequently reported [1]. Emphysema of the patient appeared after the patient blew his nose. Therefore, the mucous membrane of the maxillary sinus might have had a small hole, and air might have entered the subcutaneous tissue via the bone window when the air pressure in the maxillary sinus increased with nose blowing.
One of the complications of the sinus lift is damage of the maxillary sinus membrane, and perforation of the sinus membrane occurs in 10–35% of sinus-lift procedures [2], although membrane perforation is reduced to 7% when osteotomy is performed using the piezoelectric technique [3]. The thickness of the sinus membrane is <1 mm, so the membrane is easily damaged, and a small hole may not be apparent during the operation. The maxillary sinus is sometimes perforated by the extraction of teeth in contact with the maxillary sinus floor. Perforation is common with the presence of a maxillary sinus septum or a history of surgery in the sinus region [4]. Rhymes reported that if the vertical section of the attached gingiva reaches the infraversion, then, during tooth extraction, it is easy to cause emphysema because air readily invades the loose tissue [5]. Furthermore, an inflow of air from the gap is reported to occur easily because of the texture when the periosteum or fascia is torn [6]. Emphysema may occur when soft tissue is incised or ablated. To prevent emphysema, surgeons should take care not to tear the periosteum during periosteum detachment in mucoperiosteal flap creation.
Emphysema with sinus lift has not previously been reported and may not be anticipated with this procedure. Patients are usually requested not to blow their noses after extraction of teeth in contact with the maxillary sinus or palatal closure of a fistula. However, we did not consider this precaution necessary with the sinus-lift procedure. It is important to advise patients to avoid increasing the intraoral pressure, for example, by blowing the nose vigorously or playing musical instruments, as these activities could cause introduction of more air [7]. Therefore, it is important to warn patients about nose blowing, coughing, sneezing and mucous plugging during the postinjury and postoperative periods [8, 9]. Special attention should be paid to postoperative supportive care to avoid increased subcutaneous air diffusion in patients who have undergone open surgery [10].
The emphysema in this case was localized and not severe. However, it is necessary for oral surgeons to consider the possibility of postoperative subcutaneous emphysema after a maxillary sinus lift and to inform patients accordingly.
CONFLICT OF INTEREST STATEMENT
None declared.



