-
PDF
- Split View
-
Views
-
Cite
Cite
Patrick Tomasetti, Johannes Kuttenberger, Renzo Bassetti, Distinct subcutaneous emphysema following surgical wisdom tooth extraction in a patient suffering from ‘Gilles de la Tourette syndrome’, Journal of Surgical Case Reports, Volume 2015, Issue 6, June 2015, rjv068, https://doi.org/10.1093/jscr/rjv068
Close - Share Icon Share
Abstract
Subcutaneous emphysema is a rare complication in oral surgery. In most cases, it resolves spontaneously. However, air might disperse into deeper facial spaces causing life-threatening complications such as compression of the tracheobronchial tree or the development of pneumomediastinum. Moreover, microorganisms might spread from the oral cavity into deeper spaces. Hence, rapid diagnosis of subcutaneous emphysema is important. Characteristic signs are both a shiftable swelling and crepitation. In this case report, a 30-year-old man, suffering from the Gilles de la Tourette Syndrome, with a distinct subcutaneous emphysema after bilateral surgical wisdom tooth extraction is presented. Induced by a specific motor tic, air accumulated from the periorbital through to the parapharyngeal region. Applying a 10-cm-long Redon drainage tube as air valve, 10 days after wisdom teeth extraction, the patient was asymptomatic with complete resolution of the emphysema.
INTRODUCTION
Subcutaneous emphysema is a rare complication following dental treatments. It mainly occurs when air is injected powerfully into the connective tissue. Frequently, the introduced air is limited to the subcutaneous space and leads to local swelling and crepitus in the absence of any signs of inflammation such as erythema, edema, tenderness or lymphadenopathy [1, 2]. However, there is a potential risk that the air disperses along the facial planes to the periorbital and mediastinal spaces [2]. In the literature, the most common causes of subcutaneous emphysema are the use of air turbine handpieces [2, 3] and air syringes [2, 3]. In addition, subcutaneous emphysema can be caused by coughing, blowing, smoking, vomiting and using straws after a dental treatment [2].
Gilles de la Tourette Syndrome (GTS) is a disorder that is characterized by multiple motor tics, especially affecting cranial and upper limb muscles and vocal tics. Furthermore, GTS patients often exhibit manifest psychiatric disturbances [4]. Although several GTS patients can temporarily suppress their tics to some extent, tic emergence is rather random and intrusive [5]. Action inhibition is essential for successful goal-directed motor behavior [5]. Therefore, it has been suggested that tics in GTS patients are associated with an insufficient inhibitor motor control [6, 7].
To the best of our knowledge, the development of a subcutaneous emphysema in the context of the presence of GTS has not been described yet. In this case report, a patient with GTS who developed a subcutaneous emphysema following surgical wisdom tooth extraction is presented.
CASE REPORT
A 30-year-old man was referred to the Department of Oral and Maxillofacial Surgery because of a soft tissue swelling in the facial area. This diffuse facial swelling had developed after bilateral surgical wisdom tooth extraction in the mandible in local anesthesia on the same day in a private dental office.
The patient was suffering from GTS since childhood. Apart from this, the general anamnesis of the patient was normal. GTS is characterized by repeated, quick movements or sounds, which cannot be controlled by the patients. This patient permanently repeated Valsalva maneuvers and pressed air against his closed lips.
At admission, the patient was hemodynamically stable, afebrile and the function of the facial and trigeminal nerves were normal. In addition, no general malaise was existing, and the C-reactive protein (CRP) level was within normal ranges. Clinically, an extensive diffuse swelling in the whole facial area was visible, and the patient had difficulty in opening his eyes (Figs 1 and 2). Mouth opening was slightly limited (cutting edge inter-incisor distance: 36 mm). On palpation, there was a manifest crepitus of the periorbital region, the cheek and the supraclavicular fossa. Intraorally, the extraction sockets were not closed but appeared nonirritated. The floor of the mouth and the pharyngeal region were unaffected, and the patient was able to swallow but showed commencing respiratory distress.

Clinical appearance of the patient with distinct swelling in the periorbital, cheek and supraclavicular region after bilateral wisdom tooth removal.

Computed tomography (CT) of the head and neck region revealed a bilaterally located subcutaneous air collection in the area of the periorbital, temporal, paramandibular and supraclavicular region (Figs 3–5). There were no signs or symptoms of severe complications such as pneumothorax or pneumomediastinum.

CT scan (coronal section in the first premolar region) showing multiple air inclusions within the facial soft tissue.
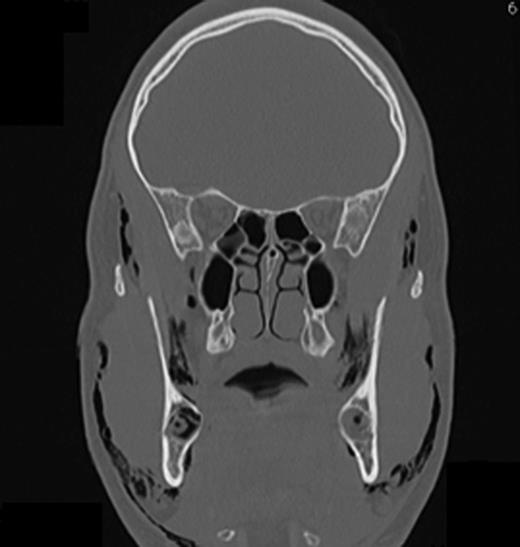
The frontal CT scan of the head and neck region (section in the retromolar region) illustrates bilaterally trapped air into the soft tissue reaching from the temporal fascia through to the supraclavicular region.
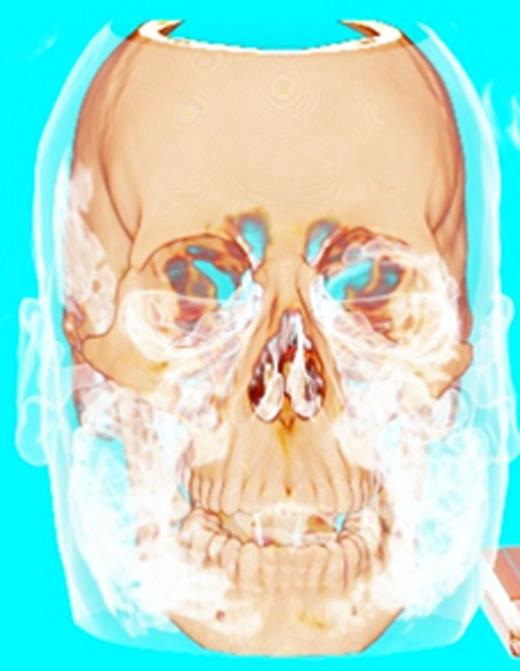
Three-dimensional reconstruction of the CT scan showing the trapped air in the head and neck region.
Because of the extensive emphysema, the patient was admitted for an inpatient monitoring. In order to avoid an infection, intravenous antibiotic prophylaxis was given (amoxicillin/clavulanic acid, 2.2 gr iv. 3x/d; Augmentin, Galaxosmithkline, Vienna, Austria). In addition, corticosteroids (Solu-Medrol 250 mg iv. 2x/d for 2 days, Pfizer AG, Zürich, Switzerland) were prescribed. In order to prevent the tic-induced powerful injection of air into the soft tissue, caused by the repetitive Valsalva maneuvers, a 10-cm-long small tube (Redon drainage tube cut in shape) was given to the patient, and the correct handling was instructed. By applying this tube, the building-up air pressure within the patient's oral cavity was prevented (Fig. 6).

The patient after 3 days with tube in place, which served as a valve to avoid air pressure within the oral cavity.
After 3 days, the facial swelling was reduced approximately by half, and the subcutaneous crepitus was almost undetectable, and so the patient could leave the hospital. Oral antibiotic prophylaxis was continued for 7 days (amoxicillin/clavulanic acid, 875/125 mg tid; Augmentin). At that time, the emphysema had completely resolved.
This case report was submitted and approved by the Ethics Committee of Northwest and Central Switzerland (EKNZ).
DISCUSSION
Subcutaneous emphysema following dental procedures, albeit rare, might cause severe complications including pneumomediastinum and mediastinitis. Hence, rapid diagnosis of a subcutaneous emphysema is of paramount importance. Spreading air in subcutaneous tissue increases the risk of subsequent connective tissue infections. Due to the communication of the facial spaces with the mediastinum, there is an increased risk for spreading of bacteria and the development of life-threatening infections of the retropharyngeal space and the mediastinum [2, 8, 9].
In principle, two factors are prerequisite for the formation of a subcutaneous emphysema: (i) air forced under pressure and (ii) a communication between the oral cavity and the subcutaneous tissue [2].
In this case, the combination of bilateral surgical wisdom tooth extraction in the mandible and the presence of the motor tic to press air against the resistance of the closed lips caused by GTS led to the distinct subcutaneous emphysema. The formation mechanism in this specific case is comparable with the first published case of a subcutaneous emphysema more than 100 years ago: A horn blower, who played his instrument immediately after a tooth extraction [10]. As motor tics of GTS patients can hardly be controlled, the usage of a Redon drainage was instructed in order to prevent the patient from elevating pressure within the oral cavity.
The diagnostic work-up of a patient with suspected subcutaneous emphysema includes a clinical examination, laboratory analysis (CRP levels) and a CT of the affected region. Following the exclusion of potentially life-threatening complications, antibiotic prophylaxis to avoid infections is recommended [2].
Concluding, a sudden swelling occurring after tooth extraction might be due to a subcutaneous emphysema. A thorough clinical examination has to be performed, and the patient should be referred to a specialized maxillofacial clinic.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflict of interest.



