-
PDF
- Split View
-
Views
-
Cite
Cite
Akihiro Hoshino, Yasuyuki Kawachi, Susumu Takamatsu, Hiroto Nagano, Syunro Ohtsukasa, Syunsuke Kato, Hiroshi Maruyama, Reduction en masse can be treated using pure laparoscopic transabdominal preperitoneal hernioplasty following early CT diagnosis: report of a case, Journal of Surgical Case Reports, Volume 2015, Issue 5, May 2015, rjv055, https://doi.org/10.1093/jscr/rjv055
Close - Share Icon Share
Abstract
Reduction en masse refers to the rare occurrence of an incarcerated inguinal hernia arising from the manual reduction of a hernia. Such a condition constitutes a medical emergency because the hernia contents, such as the small bowel, remain strangulated in the preperitoneal space. Therefore, an early and accurate diagnosis, with early treatment, is important. A 61-year-old Japanese man presented with an irreducible lump over his left groin, leading to the reduction of an incarcerated inguinal hernia by a doctor at another hospital. Later, he was admitted to our hospital with vomiting and abdominal pain. Computed tomography showed a ball-like lesion containing an incarcerated bowel loop over his left pelvis. The patient was diagnosed with an incarcerated small bowel obstruction due to a reduction en masse; a laparoscopic transabdominal preperitoneal (TAPP) hernioplasty was performed. TAPP hernioplasty is a safe method for treating reductions en masse that allows confirmation of bowel viability.
INTRODUCTION
Reduction en masse of an inguinal hernia is a rare condition, most often arising from the manual reduction of the hernia. The hernia contents remain in the hernia sac, and also in the preperitoneal space. Because of continued incarceration, accurate preoperative diagnosis of an inguinal hernia reduction en masse is important, and surgery must be quickly performed to prevent potential complications. We report a case in which accurate preoperative diagnosis was performed using computed tomography (CT), and a pure laparoscopic transabdominal preperitoneal (TAPP) hernioplasty was performed to immediately treat the patient.
CASE REPORT
A 61-year-old Japanese man presented with an irreducible lump over his left groin, leading to the reduction of an incarcerated inguinal hernia by a doctor at another hospital. Later, he was admitted to our hospital with vomiting and abdominal pain. A physical examination revealed a soft abdomen, with some distension. Some tenderness was also noted over the lower abdomen, but there was no longer a lump over his left groin. CT showed a ball-like lesion containing an incarcerated bowel loop over his left pelvis (Fig. 1a and b). The patient was diagnosed with an incarcerated small bowel obstruction due to an inguinal hernia reduction en masse; a laparoscopic TAPP hernioplasty was performed.
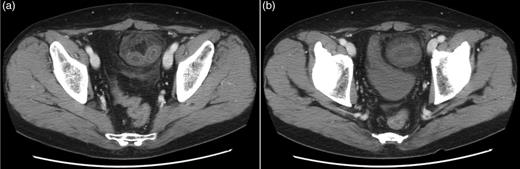
(a) Contrast axial CT shows a closed bowel loop with surrounding preperitoneal fat. (b) CT scans at the inguinal levels show the hernia sac and its contents compressing the urinary bladder, so that it shows a beak-like deformity.
A 12-mm trocar was inserted, via a minilaparotomy in the umbilicus, to create an artificial pneumoperitoneum and to introduce a flexible laparoscope, under general anesthesia. Two, 5 mm trocars were inserted along the mammary line of the left umbilical region and right lower abdominal region. The incarcerated bowel was naturally released as a result of the combined effects of the muscle relaxant under general anesthesia, and hernia orifice dilatation during the induction of the artificial pneumoperitoneum for groin laparoscopy (Fig. 2a). Small intestine congestion was noted, but the small intestine was not strangulated (Fig. 2b). The hernia sac was resected and a wide range of the preperitoneal cavity was dissected (Fig. 2c). The myopectineal orifice was then covered with a 14 × 10 cm polyester mesh (Parietex™ Folding Mesh; Covidien, Mansfield, MA, USA; Fig. 2d). Absorbable staple fixation devices (Absorba Tack™; Covidien) were used to secure the mesh, and the peritoneal flap was closed with continuous suturing. Finally, the viability of the incarcerated small intestine was confirmed. The operative time was 79 min. The patient's postoperative course was uneventful, and he was discharged 4 days after surgery. At the 23-month follow-up, the patient's clinical condition was satisfactory and there was no evidence of recurrence.
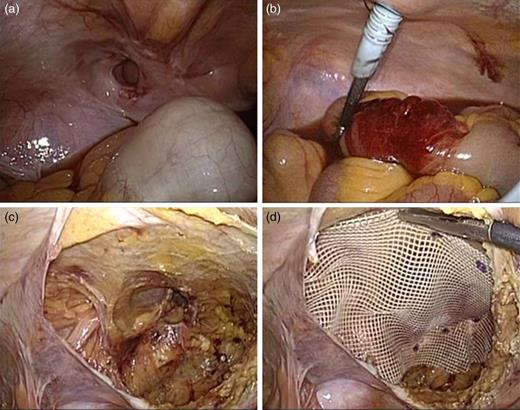
(a) Intraoperative photograph showing the hernia sac surrounded by a thickened peritoneum, extending into the preperitoneal space. The incarcerated bowel was released from the hernia sac naturally, after creating an artificial pneumoperitoneum under general anesthesia. (b) The viability of the incarcerated small intestine is confirmed, laparoscopically. (c) After the preperitoneal space was dissected, a hernia was detected in the left inguinal region; no concomitant hernia was observed. (d) The myopectineal orifice was covered with a 14 × 10 cm polyester mesh in the left inguinal region.
DISCUSSION
Reduction en masse of an inguinal hernia is a condition in which the incarcerated hernia contents are reduced into the preperitoneal cavity along with the hernia sac [1]. This condition is estimated to occur in ∼1 of the 13 000 hernias [2]. If abdominal pain and ileus appear after reduction of an incarcerated inguinal hernia, reduction en masse of an inguinal hernia should be considered. However, a delay in preoperative diagnosis is not infrequent because the hernia is clinically reduced.
CT and an accurate clinical history are useful for making an accurate preoperative diagnosis. Kitami et al. [3] reported the CT findings of reduction en masse to include (i) a closed-loop obstruction with a ball-like bowel loop, (ii) a location adjacent to the inguinal fossa, (iii) a circular funicular structure at the obstruction point, (iv) a beak of the bladder along the closed loop and (v) a prominent unilateral inguinal soft tissue. Because a reduction en masse involves continued incarceration, prolonging the time to surgery increases the risk of complications and may be fatal. In our case, the characteristic CT findings were observed, allowing easy diagnosis of a reduction en masse and facilitating immediate corrective surgery.
During treatment of an incarcerated hernia, including reduction en masse, the confirmation of incarcerated bowel viability is important to determine whether bowel resection is needed and whether mesh is used. The laparoscopic and open laparotomy methods for confirming bowel viability have been previously reported [1, 4, 5]. Open laparotomy is highly invasive and results in a high risk of complications and prolonged hospitalization [6]. However, checking bowel viability, after reducing an incarcerated hernia, is not necessarily easy using a laparoscope inserted from the hernia sac if the bowel is hidden on the dorsal side of another bowel loop. Recently, the usefulness of TAPP hernioplasty for incarcerated inguinal hernias has been reported [7, 8]. TAPP allows simple and definite exploration of the abdominal cavity for concomitant defects, easily relieves the incarcerated bowel, and allows for the determination of the bowel viability. Because bowel viability can be determined after the hernioplasty, unnecessary bowel resections can be avoided. We have performed TAPP hernioplasties for incarcerated femoral hernias, obtaining good outcomes [9]; therefore, we chose a laparoscopic TAPP hernioplasty for the current reduction en masse. Reports of laparoscopic TAPP hernioplasties for the treatment of reduction en masse defects are very rare, with only one previous case having been reported [10].
In conclusion, reductions en masse are rare, but early diagnosis is possible, if the characteristic CT findings are known. TAPP hernioplasty is a safe and useful method for treating reductions en masse, and also permits confirmation of bowel viability.
CONFLICT OF INTEREST STATEMENT
None declared.



