-
PDF
- Split View
-
Views
-
Cite
Cite
Mishank Jain, Laura Atherton, Vikas Acharya, Neel Sengupta, Marco Barreca, Incidental oesophageal leiomyoma during laparoscopic Roux-en-Y gastric bypass: finding the unexpected does not affect outcomes, Journal of Surgical Case Reports, Volume 2015, Issue 5, May 2015, rjv054, https://doi.org/10.1093/jscr/rjv054
Close - Share Icon Share
Abstract
Most bariatric procedures are now performed laparoscopically. Here, we describe a case of incidental oesophageal leiomyoma found during laparoscopic Roux-en-Y gastric bypass (LRYGB). To our knowledge, this is the first such case reported. Our patient was admitted for an elective LRYGB. She had no upper gastrointestinal symptoms, and therefore did not undergo preoperative oesophagogastroduodenoscopy (OGD). During surgery, a hiatus hernia and an incidental oesophageal leiomyoma were found and treated with hernia repair and enucleation. The end outcome was unaffected. We were able to concomitantly treat the unexpected finding of an oesophageal leiomyoma and a hiatus hernia during the LRYGB. The routine use of OGD prior to bariatric surgery is still controversial. While surgeons should be prepared for unexpected pathologies, when performing laparoscopic bariatric surgery, a routine OGD prior to LRYGB is probably not necessary in asymptomatic patients. Laparoscopic enucleation of oesophageal leiomyoma during LRYGB is feasible and safe.
INTRODUCTION
Obesity is on the rise worldwide with a projected 65 million more obese adults in the USA and 11 million more obese adults in the UK by 2030. This will lead to an additional 6–8.5 million cases of diabetes, 5.7–7.3 million cases of heart disease and stroke, 492 000–669 000 additional cases of cancer and 26–55 million quality-adjusted life years lost for USA and UK combined [1].
With the increasing prevalence of morbid obesity, the number of bariatric procedures performed has also risen. Laparoscopy now represents the main approach for all bariatric procedures [2]. Coincidental findings of unexpected pathology are not uncommon, especially if preoperative investigations are not indicated by the patients’ history [3]. This study describes a case of an incidental oesophageal leiomyoma and a hiatus hernia found during laparoscopic Roux-en-Y gastric bypass (LRYGB).
CASE REPORT
A 58-year-old woman was admitted for an elective LRYGB. Her medical history included obstructive sleep apnoea (on regular continuous positive airway pressure ventilator), hypertension, hypercholesterolaemia, psoriatic arthritis and previous endometrial cancer (treated by hysterectomy). Her preoperative BMI was 40 and she was American Society of Anaesthesiologists physical status classification 3. There was no history of any upper gastrointestinal symptoms prior to admission or during pre-assessment.
The patient underwent an LRYGB during which an incidental hiatus hernia and a 40 × 30 × 20 mm stromal lesion extending from the distal oesophagus to the gastro-oesophageal junction became evident. These were coincidental finding prior to the definitive bariatric procedure being undertaken, and were both managed concomitantly.
Preoperative assessment included routine bloods and thyroid function tests, ECG and echocardiogram; all of which were within normal limits. This patient was asymptomatic and as per the departmental protocol for LRYGB, did not undergo preoperative oesophagogastroduodenoscopy (OGD; i.e. if the patient was undergoing a gastric sleeve operation, she would have had preoperative OGD to exclude Barrett's oesophagus).
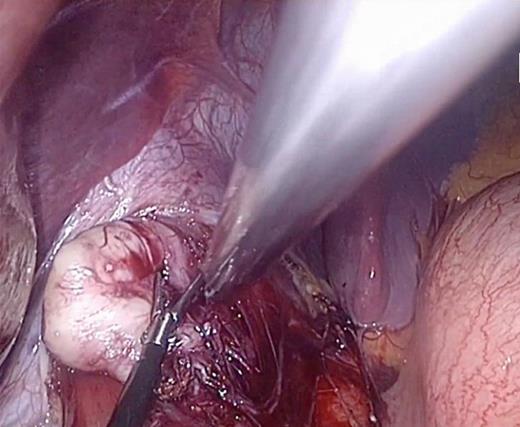
After dissection of the oesophago-gastric ligament and reduction of herniated stomach into the abdomen, the lesion in the distal oesophagus was identified (Fig. 1). It was enucleated leaving the oesophageal and gastric mucosa intact. The remainder of the procedure then continued as planned and was uneventful. The patient had no concerns postoperatively and was discharged home within 24 h. The lesion was sent for histopathological analysis and a plan for follow-up was organized.
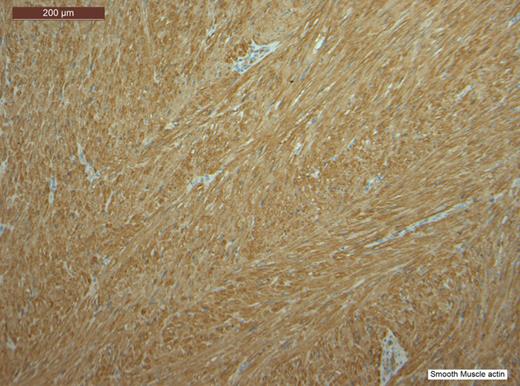
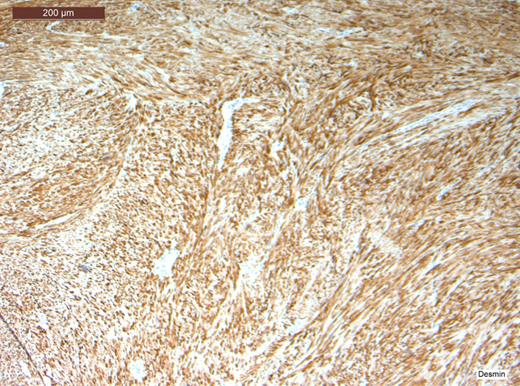
Histopathological analysis of the lesion, including immunohistochemical profiling, revealed a well-circumscribed nodular tumour composed of smooth muscle cells with eosinophilic cytoplasm and spindle-shaped nuclei. The cells were arranged in interlacing fascicles with evidence of perinuclear vacuoles using haematoxylin and eosin staining. There was no evidence of necrosis, mitosis or significant nuclear pleomorphism. The specimen was negative for CD117 staining, hence excluding the possibility of a gastrointestinal stromal tumour. It was also negative for S100. However, stain was positive for smooth muscle actin (SMA) and desmin, which confirmed that specimen was of muscular origin. The histology therefore identified the lesion as a leiomyoma (Figs 2–6).
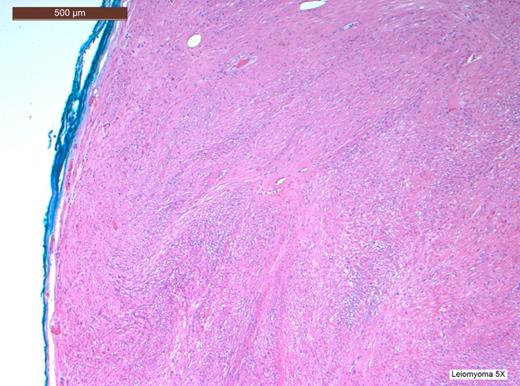
H&E stain at low power view revealing a tumour with a well-circumscribed edge with fascicles of spindle-shaped cells.
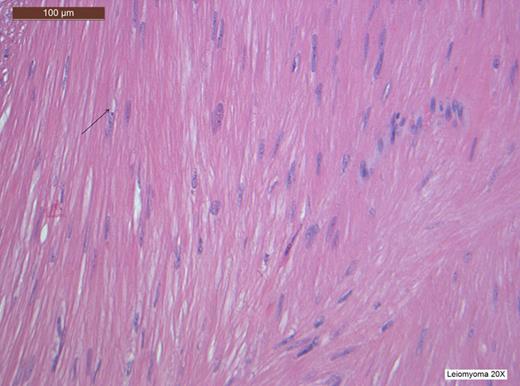
H&E stain at high power view showing spindle-shaped cells and perinuclear vacuoles, a characteristic finding of leiomyomas.
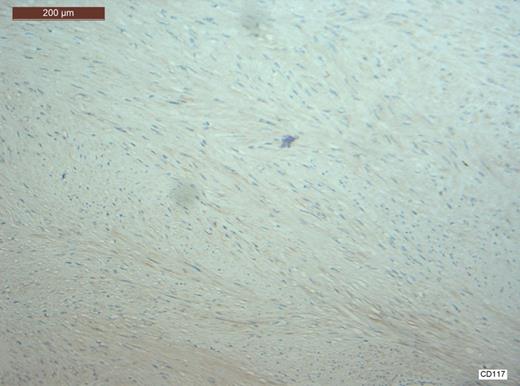
CD117 staining is negative hence excluding any possibility that this was a gastrointestinal stromal tumour (GIST).
The patient was reviewed 6 weeks, 3 and 6 months postoperatively, and was making excellent progress. She had lost 33 kg in weight. There were no new or concerning upper gastrointestinal symptoms.
DISCUSSION
Benign tumours of the oesophagus are rare lesions. They constitute <1% of oesophageal neoplasms, with leiomyomas making up nearly two-third of these [4]. They are most common in individuals between the ages of 20 and 50 years [4]. A leiomyoma is a benign mesenchymal tumour, which arises from smooth muscle cells. They are well dermarcated by adjacent tissue due to a smooth connective tissue capsule, and usually develop intramurally, most commonly in the distal two-third of the oesophagus [4]. Most leiomyomas cause no signs or symptoms and are discovered incidentally during an operative procedure or on postmortem [4]. Symptoms are dependent on the tumour size, location and subsequent arising complications, for example, bleeding or ulceration [5]. The most common presenting symptoms are bleeding (acute or chronic), abdominal pain and discomfort, nausea, weight loss and intestinal obstruction [5]. Our patient was asymptomatic, with no history of gastro-oesophageal reflux disease or dysphagia.
The case for OGD in routine work-up prior to bariatric surgery remains a matter of debate [6, 7]. Numerous studies have looked into the outcomes of such preoperative assessments and evaluated their worth. They all suggest that even when abnormalities are found on OGD, very few will result in a change in the surgical outcome or approach taken [8–10]. It has consistently been found that the most common finding on OGD prior to bariatric surgery is the presence of a hiatus hernia [8, 10]. This is also a common incidental finding in our centre with an estimated 15% of bariatric patients being diagnosed with hiatus hernias at the time of the operation. The presence of a hiatus hernia in our experience does not compromise our management or approach used. Other common findings include oesophagitis, peptic ulcers and gastritis, but less likely in asymptomatic patients [8–10]. In our institution, we have adopted a selective use of gastroscopy in the work-up of patients undergoing bariatric surgery, performing gastroscopy only in patients with a clinical history positive for upper gastrointestinal symptoms.
Cases of leiomyomas found on OGD prior to bariatric surgery have previously been reported; however, there are no reports of incidental oesophageal leiyomyomas found and excised during LRYGB.
The absence of a preoperative OGD did not change the end outcome for this patient and there were no associated complications. Hence, while it is important to be aware about the possibility of the presence of abnormal pathology when performing the operation, a routine OGD prior to gastric bypass surgery is not always necessary. The decision needs to be made using clinical judgement based on other indicative factors during preoperative assessment.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- upper gastrointestinal endoscopy
- hernia, hiatal
- laparoscopy
- preoperative care
- surgical procedures, operative
- surgery specialty
- leiomyoma of esophagus
- cellular enucleation
- bariatric surgery
- gastric bypass, roux-en-y, laparoscopic
- hernia repair
- upper gastrointestinal symptoms
- laparoscopic bariatric surgery
- enucleation procedure



