-
PDF
- Split View
-
Views
-
Cite
Cite
Tsuyoshi Ozawa, Shinsuke Saito, Sohei Matsuura, Hirohisa Kishi, Mamoru Maeda, Toshiaki Watanabe, Thyroid gland metastasis of rectal cancer, Journal of Surgical Case Reports, Volume 2015, Issue 5, May 2015, rjv053, https://doi.org/10.1093/jscr/rjv053
Close - Share Icon Share
Abstract
A 72-year-old woman with a history of rectal cancer was admitted to our hospital to undergo thyroidectomy and left adrenalectomy. She had undergone low anterior resection and regional lymph node dissection for rectal cancer 52 months pre-admission (T3 N1 M0, stage IIIb according to International Union Against Cancer tumor-node-metastasis), and she had also undergone metastasectomy for lung metastases and right adrenal gland metastasis after the rectal surgery. Follow-up computed tomography scans detected nodules in the bilateral lobes of the thyroid gland and in the left adrenal gland. Subtotal thyroidectomy and left adrenalectomy were performed, and pathological examination revealed metastases of rectal cancer to the thyroid gland and left adrenal gland.
INTRODUCTION
The thyroid gland is rarely the site of metastasis of malignant tumors, and metastatic tumors are reported to represent only 2–3% of all malignant tumors of the thyroid gland [1]. Primary carcinomas that frequently metastasize to the thyroid gland include malignant melanomas, as well as breast, kidney and lung cancers [2]. On the other hand, colorectal cancer rarely metastasizes to the thyroid gland. Here, we report a case of a 72-year-old female with a history of rectal cancer, presenting with nodules in the thyroid gland incidentally detected on a computed tomography (CT) scan, who subsequently underwent surgical resection.
CASE REPORT
A 72-year-old-woman with a history of rectal cancer was admitted to the Doaikinen Hospital, Tokyo, Japan, in November 2013. She had undergone radical surgery for rectal cancer in July 2009. The pathological examination revealed a moderately differentiated adenocarcinoma with lymphatic and venous invasion, and the pathological grade was T3 N1 M0, stage IIIb, according to the International Union Against Cancer tumor-node-metastasis (TNM) 7th classification. She received adjuvant chemotherapy with capecitabine, but right lung metastasis was detected in October 2010 on follow-up CT scan. After subsequent chemotherapy of irinotecan with tegafur–gimeracil–oteracil potassium (IRIS), she underwent partial resection of the right lung in March 2011. She did not receive adjuvant chemotherapy post-operation, and right lung metastasis was detected again in January 2012. Chemotherapy of IRIS with panitumumab (Pmab) was initiated, but the lung metastasis progressed, and right adrenal gland metastasis appeared in August 2012. Both metastases were assessed to be surgically resectable, so partial resection of the right lung was performed in September 2012, and right adrenalectomy was performed in November 2012. Adjuvant chemotherapy of oxaliplatin with fluorouracil and folinic acid was introduced after the operation, but carcinoembryonic antigen and carbohydrate antigen levels gradually increased (Fig. 1). Follow-up CT scans detected nodules in the left adrenal gland and bilateral thyroid gland in October 2013 (Fig. 2a–c). The serum level of thyroid-stimulating hormone was 1.79 μU/ml, Free-T3 was 2.83 pg/ml, Free-T4 was 1.10 ng/dl and thyroglobulin was 101 ng/ml. Fine-needle aspiration was performed on the nodules of the thyroid gland, and metastasis of rectal cancer was highly suspected histologically. 18F-fludeoxyglucose positron emission tomography (18FDG-PET) scan revealed high uptake of 18FDG in the nodule of the left lobe of the thyroid gland, and in the left adrenal gland (Fig. 2d–f). No metastasis in the other organs was detected on the radiological findings, and hence we decided to perform surgical resection for the tumors of the thyroid gland and left adrenal gland.
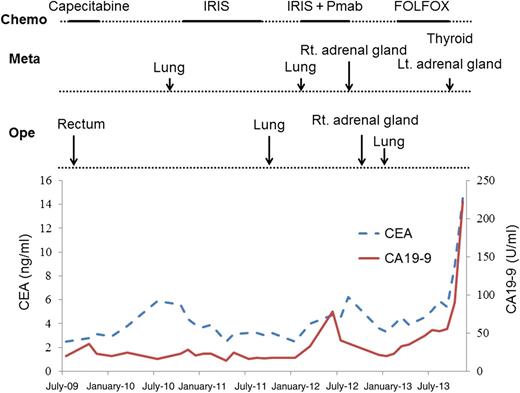
Clinical course and changes of tumor markers. CEA: carcinoembryonic antigen; CA19-9: carbohydrate antigen; Chemo: chemotherapy; Ope: operation; Meta: metastatic place; IRIS: irinotecan with tegafur–gimeracil–oteracil potassium; Pmab: panitumumab; FOLFOX: oxaliplatin with fluorouracil and folinic acid; Rt: right; Lt: left.
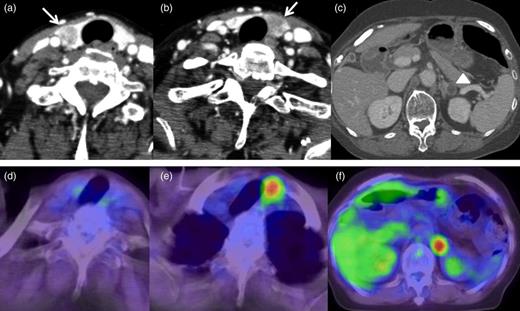
CT scans and PET scans of the neck and abdomen. (a and b) CT scan of the neck detected low-density nodules in bilateral lobes of the thyroid gland (arrows). (c) CT scan of the abdomen detected a low-density nodule with clear border in the left adrenal gland. (d) PET scan did not show abnormal uptake of 18FDG in the nodule in the right lobe of the thyroid gland. (e) PET scan showed abnormal uptake of 18FDG in the nodule in the left lobe of the thyroid gland. (f) PET scan detected abnormal uptake of 18FDG in the nodule in the left adrenal gland.
Subtotal thyroidectomy and left adrenalectomy were performed without any complications in November 2013. The patient's postsurgical progress was favorable, and she was discharged 11 days after the operation.
Pathological examinations of the excised thyroid gland and left adrenal gland revealed adenocarcinomas, consistent with metastatic rectal adenocarcinoma. In the thyroid gland, a nodule was detected in each lobe, and multiple small metastatic lesions were observed histologically around the nodules. Venous invasion was present, but lymphatic invasion was not detected. Immunohistochemical (IHC) staining of cytokeratin 20 (CK20), a colorectal cancer marker, was positive in the tumor cells (Fig. 3).
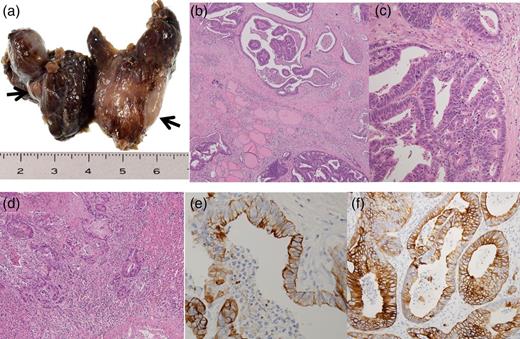
Pathological findings of resected thyroid gland. (a) Macroscopic findings of thyroid gland detected a nodule in each lobe (arrows). (b and c) Microscopic findings of thyroid gland detected adenocarcinoma consistent with metastatic rectal adenocarcinoma (original magnification, ×100 and ×200, respectively). (d) Microscopic findings of the left adrenal gland detected adenocarcinoma consistent with metastatic rectal adenocarcinoma (original magnification, ×100). (e) IHC staining of CK20 was positive in tumor cells of the thyroid gland (original magnification, ×400). (f) IHC staining of CK20 was positive in tumor cells of the left adrenal gland (original magnification, ×400).
DISCUSSION
Thyroid gland metastasis of colorectal cancer is clinically rare. Shimaoka et al. reported in their study that thyroid metastases were histologically detected in 188 of 2180 autopsy cases of malignant tumors (8.6%), but that 109 of these cases (58%) were only microscopic metastases, and <5% of the thyroid gland metastases were clinically apparent. In that report, primary carcinomas that frequently metastasized to the thyroid gland were found to be malignant melanomas (39%) as well as breast (21%), kidney (12%) and lung (11%) cancers, whereas colorectal cancers only metastasized to the thyroid gland in 4% of cases [2].
Willis put forward two hypotheses to explain why thyroid gland metastasis was rare: (i) the thyroid gland receives an abundant supply of arterial blood, and rapid blood flow prevents tumor cells from tumor fixation in the thyroid gland and (ii) the high oxygen saturation and high iodine content in the thyroid gland prevent tumor growth in the thyroid gland [3]. The author also hypothesized that adenomatous or fibrous changes resulted in decreased arterial blood flow, low oxygen and/or iodine concentration in the thyroid gland, thereby facilitating metastasis.
The metastatic pathway to the thyroid gland has been proposed to be either hematogenous or lymphogenous [4, 5]. In previous reports, many cases have been found to co-present with synchronous or metachronous lung or liver metastasis, supporting the hematogenous metastatic pathway to the thyroid gland in colorectal cancer [6–8]. Similarly, in the present case, lung metastases and adrenal gland metastases were seen, and this supported the hematogenous metastatic pathway. Additionally, histological examination of the present case detected venous invasion without lymphatic invasion in the thyroid gland, further supporting the hematogenous metastatic pathway.
The typical surgical treatment for solitary thyroid gland metastasis is partial resection of the thyroid gland including the metastatic tumor, but surgery may range from partial resection to total thyroidectomy, and the need for lymphadenectomy is not certain. In the present case, histologically small metastatic lesions were detected around the nodules, and thus, partial resection might have resulted in residual cancer cells. The prognosis of thyroid gland metastasis of colorectal cancer is very poor, because systemic extension is usually seen, and most of the patients have synchronous or metachronous metastasis in the other organs at the time of detection of the thyroid metastasis. However, Hegerova et al. [9] reported that those who underwent thyroid resection had better outcomes compared with those without thyroid surgery for thyroid gland metastasis. Hence, treatment should be decided based on the total condition of tumor progression, and metastasectomy is a valid choice of treatment as long as all of the metastatic lesions can be resected, or if the metastatic lesion causes clinical adverse events.
Thyroid metastasis of colorectal cancer is rare, but we have to consider thyroid gland metastasis in follow-up examinations for the recurrence of colorectal cancer. Treatment should be decided in consideration of the tumor progression.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- adrenal glands
- computed tomography
- cancer
- adrenalectomy
- follow-up
- neoplasm metastasis
- surgical procedures, operative
- thyroidectomy
- thyroid
- metastasis to the lung
- rectal carcinoma
- subtotal thyroidectomy
- tnm tumor staging system
- low anterior resection of rectum
- rectosigmoidectomy
- metastasectomy
- regional lymph node dissection
- right adrenal gland



