-
PDF
- Split View
-
Views
-
Cite
Cite
Paul Sooby, Raj Harshen, Rita Joarder, An unusual triad of pneumatosis intestinalis, portal venous gas and pneumoperitoneum in an asymptomatic patient, Journal of Surgical Case Reports, Volume 2015, Issue 4, April 2015, rjv035, https://doi.org/10.1093/jscr/rjv035
Close - Share Icon Share
Abstract
Pneumatosis intestinalis (PI) is defined as the presence of gas within the serosal or mucosal layer bowel wall. This sign is usually found upon radiographic imaging and is most commonly secondary to acute gastro-intestinal ischaemia. Fifteen per cent of cases can present with a primary condition called pneumatosis cystoides intestinalis (PCI). PCI is usually a benign condition and patients are usually asymptomatic. Portal venous gas (PVG) or the presence/accumulation of free gas within the hepatic portal vein. It is most commonly associated with acute bowel ischaemia, and when seen in the presence of ischaemia the mortality rate is between 75 and 90%. Other associations include mechanical causes (e.g. obstruction), chemotherapy, liver transplant and diverticulitis. Benign PI has previously been described with PVG, but usually in the presence of other associated conditions such as AIDS, malignancy or chemotherapy. Some examples have been described without these associations, but not with free intra-peritoneal air. We describe a case of PCI and PVG with pneumoperitoneum, investigations and ongoing management.
INTRODUCTION
Pneumatosis intestinalis (PI) and portal venous gas (PVG) are individually worrying radiological signs. Both are associated with severe mesenteric ischaemia and when present with symptoms of abdominal pain have a mortality rate in excess of 75%. However, both can exist either individually or concurrently without any underlying abdominal or systemic pathology. We describe a rare scenario where PI, PVG and pneumoperitoneum were found in an asymptomatic patient.
CASE REPORT
A 78-year-old male presented to the surgical assessment unit, following an abnormal chest X-ray performed for a persistent productive cough with fever. The on-duty radiologist identified that this patient had significant free air under the diaphragm on his erect chest X-ray, and contacted the general practitioner directly who in turn organized admission to the surgical services.
The patient denied abdominal pain, upper/lower abdominal symptoms. He reported a fever for 2 days prior to the time of presentation but denied further pyrexias in the previous 48 h. He still had an ongoing productive cough, but without chest pain or difficulty in breathing. His medical history included hypertension and hypercholesterolaemia. His current medication list included ramipril and simvastatin. He had no previous surgery or known allergies. He drank ∼10 units of alcohol per-week and he was an ex-smoker with a 15 pack-year history.
On examination, the patient had non-tender and soft abdomen with no distension, organomegaly and bowel sounds were present. His observations were normal. His CVS examination was unremarkable. He had mild crepitations at the right lung base, but respiratory examination was otherwise unremarkable. A digital rectal examination was unremarkable.
Baseline bloods (including a lactate) were found to be normal. A CT scan demonstrated significant free intra-peritoneal air (Figs 1–3). Circumferential and linear intra-mural gas within the small bowel was seen consistent with PI. Small locules of air were seen in close proximity to the liver which was suggestive of PVG in the peripheral portal system. A faecal calprotectin level was also sent; this was later found to be negative.

A coronal CT image of the abdomen taken at initial presentation, demonstrating free air under the diaphragm (pneumoperitoneum) and PVG, both marked on images.
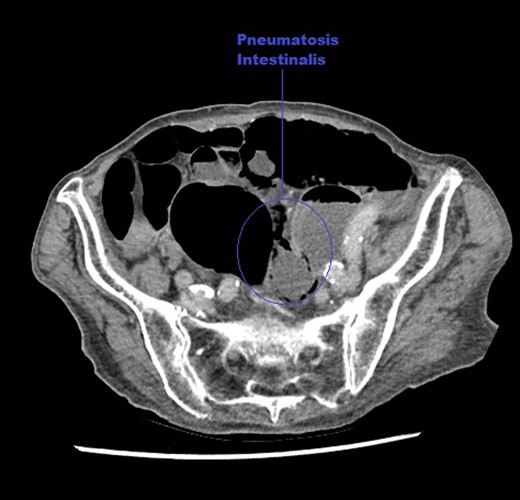
An axial CT image of the abdomen taken at initial presentation, demonstrating PI marked on the image.
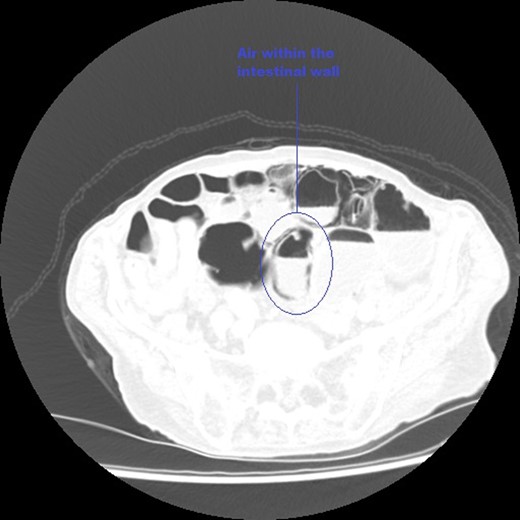
An axial CT image of the pelvis in lung view windows, taken at initial presentation clearly demonstrating intra-mural air within the bowel, marked on image.
His observations remained stable, his abdominal examination remained unremarkable and an arterial blood gas was normal. He was observed for 8 h but remained well. He discharged home with open access but was to re-attend in 48 h for repeat CT scan and re-evaluation. This second scan demonstrated an increase within the intra-abdominal air, and the gas within the portal venous system became more prominent. The patient remained asymptomatic, observations remained normal and repeat blood tests were unremarkable.
The patient was discharged with follow-up in clinic with a consultant general surgeon. Upon review, he remained well and was discharged from clinic. This patient was reviewed again 2 months later when admitted for a separate admission under orthopaedics for the management of a fractured neck of femur following a mechanical fall. His abdomen remained soft and non-tender and he denied any abdominal pain. He was discharged home from orthopaedics following the placement of a dynamic hip screw with an uneventful recovery.
DISCUSSION
PI is a rare radiographic finding with an incidence in the general population of ∼0.03%. PI is not a disease but a radiographic finding with a poorly understood pathogenesis. The mechanical theory states an increase in pressure in the bowel lumen, lungs or mediastinum causes gas to dissect through the serosal/mucosal bowel wall. The bacterial theory states that gas-forming organisms enter the layers of the bowel wall. PI can be divided into primary or secondary. The most common form of PI occurs secondary to acute gastro-intestinal ischaemia. Other associations of secondary PI include malignancy, chemotherapy, trauma, mechanical bowel disorders, COPD, liver-failure and post-endoscopy. Where PI is identified the mortality rate is ∼44%, and historically the presence of PI has necessitated a laparotomy. There is a rarer primary form of PI, referred to as pneumatosis cystoides intestinalis (PCI) accounting for 15% of cases. This condition is benign and usually presents incidentally [1, 2].
PVG is a radiological sign and marker of serious underlying GI pathology. The mortality for PVG ranges between 75 and 90%. The most common cause for PVG is acute mesenteric ischaemia accounting for ∼64% of cases. Other associations include inflammatory bowel disease, acute intestinal obstruction, trauma, malignancy, chemotherapy, liver transplant and diverticulitis. Benign PVG caused by gastric dilatation and following endoscopic procedures has been seen. Idiopathic PVG has been described but makes up ∼2% of cases [2, 3].
Both PI and PVG have been described concurrently, most commonly in symptomatic patients with severe intra-abdominal necrosis. This patient group typically have poor outcomes. PI and PVG have also been described in the asymptomatic patient. A 2009 case series of 88 cases of PI/PVG established three distinct subgroups: mechanical, ischaemic and benign. Of 88 patients, 19 were identified with benign PI including 6 patients with both PI and PVG. Two had a history of malignancy, one with acute liver failure and one with COPD. Nine patients who were identified with benign PI and/or PVG were placed under observation, all making an uneventful recovery. Thus a management algorithm for PI/PVG patients where patients are risk stratified into high-, medium- and low-risk groups was proposed, where low-risk patients are observed with medical treatment alone [4, 5].
PI can also be seen with pneumoperitoneum and it proposed that this is caused by the rupture of the intra-mural gas blebs. It is important to state that this rupture does not represent a true bowel perforation through all layers of bowel wall. Most gas blebs exist within the submucosal and subserosal layers of the bowel but these blebs do not communicate with the lumen of the bowel [6].
This case demonstrates that both the rare findings of PCI and PVG can present together in the well-asymptomatic patient. This was made even more unusual as the patient had no risk factors for either of these structural abnormalities. Whilst rare this has been described in literature before. However, this patient also had a significant pneumoperitoneum on CT imaging along with these other signs making this case particularly unusual.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- ischemia
- acquired immunodeficiency syndrome
- gastrointestinal tract vascular insufficiency
- diagnostic radiologic examination
- cancer
- chemotherapy regimen
- diverticulitis
- intestines
- liver transplantation
- pneumatosis cystoides intestinalis
- portal vein
- diagnostic imaging
- mortality
- mucous membrane
- peritoneum
- pneumoperitoneum
- portal venous gas



