-
PDF
- Split View
-
Views
-
Cite
Cite
Carlo Amati, Vito Pesce, Andrea Armenio, Giuseppe Solarino, Biagio Moretti, Tumoral calcinosis of the hand, Journal of Surgical Case Reports, Volume 2015, Issue 4, April 2015, rjv036, https://doi.org/10.1093/jscr/rjv036
Close - Share Icon Share
Abstract
Tumoral calcinosis is a rare condition described in literature as a deposition of calcium salts in soft tissues. We here report a rare case of Tumoral calcinosis in the index finger of a hand in a 22-year-old woman. Because of the absence of any trauma, normal serum phosphate and calcium levels and no symptoms but a cosmetic defect, our case is classified as a primary tumoral calcinosis. As well as described in literature, also in this case the surgical excision was the mainstay treatment for this benign pathology. For the particular area involved we performed a radical excision followed by an interesting reverse homodigital artery flap from the ulnar side of the index.
INTRODUCTION
Tumoral calcinosis is a rare condition described in literature as a deposition of calcium salts in soft tissues.
The first case was described in 1899 by Duret and termed endotheliome calcifie. After that in 1935 Teutschlaender called lipocalcinogranulomatosis another case of tumoral calcinosis. Only in 1945 the term Tumoral calcinosis was proposed by Inclan and since then it has been accepted worldwide.
We here report a rare case of Tumoral calcinosis in hand. In more than 250 cases reported in literature only a few presented the involvement of the hand.
CASE REPORT
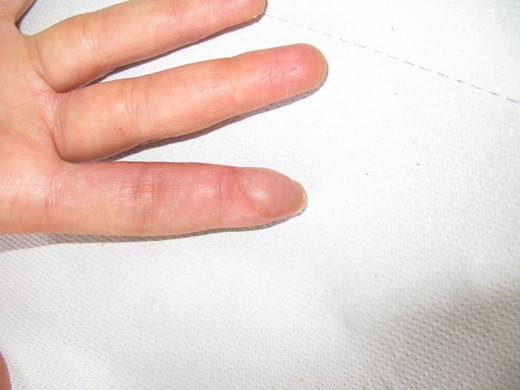
A 22-year-old woman, right dominant hand, visited our Department complaining of the presence of several small swellings localized under the skin of the pulp of the index finger (Figs 1–5). She reported an increase in the number of swellings in a period of about 2 years. She noted the first one 3 years before. She never felt pain. An X-ray of the index finger showed multiple not well-defined round-like calcified lesions, without involvement of the bone or of the distal interphalangeal joint. There were no other such lesions in the body. The patient was apyrexial and in good general health. There were no signs of tenosynovitis, palmar space or flexor sheath infection. She had no lymphangitis or regional lymphadenopathy.




ESR, cell blood count, electrolytes, uric acid, cholesterol and triglyceride levels were all normal.
The results obtained from a DXA examination reported a value of −1.5 at lumbar spine and a value of −1.8 at the femoral neck. There was no evidence of any underlying disease.
For this clinical presentation we decided to treat this young patient with a surgical excision of the calcific deposits. A wide excision of the volar surface of the distal phalanx including the calcified nodules was performed. Skin affected by tumoral calcinosis was also excised preserving the neurovascular bundles and FDP insertion. The masses appeared yellowish and chalky, with a maximum size of 0.5 × 0.5 × 0.3 cm (one of them).
The soft tissue defect was reconstructed by harvesting a reverse homodigital artery flap from the ulnar side of the index and transposing the flap into the defect. The flap was based on ulnar digital artery reverse flow. A full thickness skin graft was also harvested from the forearm to cover the flap donor area.
Postoperative recovery was uneventful with no loss of flap or skin graft. The patient was discharged 4 days post-surgery and resumed normal activity by 6 weeks.
The specimen was sent for histological examination. Histology confirmed the presence of granules and deposits of calcium in the soft tissue.
DISCUSSION
Since Duret first described this disease in 1899 in a 17-year-old girl and then in her younger brother, more than 250 cases have been reported [1, 2].
In the most of cases described in literature Tumoral calcinosis occurs in younger patients like our patient, but affects multiple joints and has a familial tendency [3, 4]. Sites of preference are lateral and superior aspect of shoulder, posterior aspect of elbow [5] and laterally around the hips and buttocks. Very rare positions are the hands and the wrists [6, 7]. Isolated hand involvement is extremely rare. Malik and Acharya [8], Sabesta et al. [9], Murai et al. [10] reported only four cases of hand involvement. Recently has been described a case of hand involvement in a 35-year-old woman [11].
It has been suggested that tumoral calcinosis should be divided into three subtypes on a pathogenetic basis [12]: (i) primary normophosphatemic tumoral calcinosis recognized in patients with normal serum phosphate and serum calcium levels and no evidence of disorders previously associated with soft tissue calcification; (ii) primary hyperphosphatemic tumoral calcinosis, in patients with an elevated serum phosphate level, a normal serum calcium level, and no evidence of disorders previously associated with soft tissue calcification; (iii) secondary tumoral calcinosis when the patients have a concurrent disease capable of causing multiple soft tissue calcification and familial occurrence.
The present case had normal serum phosphate but reduced serum calcium levels, several localized calcifications and no evidence of previous soft tissue calcification. A DEXA examination showed an osteopenia at the spine site (T score −1.2) and at the femoral neck (T score –0.5). These features indicate that our case could be classified as primary normophosphatemic tumoral calcinosis.
Primary normophosphatemic forms occur without a recognizable cause. A localized soft tissue modification is hypothesized as a pathogenetic role. An abnormal tissue response to local trauma, as suggested by Pakasa and Kalengayi (1997), may be a cause of tumoral calcinosis. However, a trauma has rarely been reported by patients as in this case.
Surgical excision in tumoral calcinosis is the mainstream treatment [13]: this is recognized by several authors; recurrence is rare. Researchers advocate meticulous excision.
In our case, after a deep inspection, we found about 7–8 calcific masses under the skin. None of them had ulcerations and there was no discharge of any kind of fluid. We performed a radical excision followed by a reverse homodigital artery flap from the ulnar side of the index and transposing the flap into the defect. The flap was based on ulnar digital artery reverse flow. A full thickness skin graft was also harvested from the forearm to cover the flap donor area. This procedure is well documented in literature with good results [14], while the classical cross-finger flap is less and less used. Our patient had an excellent recover considering the exterior aspect and a two-point discrimination at the 12-month follow-up of about 8 mm.
The histological examination highlighted the presence of an irregular structure with fibrous connective tissue bands, calcareous deposits and the absence of any uric acid crystals. On microscopy macrophages, multinucleated giant cells and chronic inflammatory cells lining the fibrous bands were noted.
The laboratory investigations were within normal limits, including serum calcium, C-reactive protein and white blood cells.
At the 12-month follow-up appointment, our patient did not show any recurrence.
Our main objectives were to remove completely the mass and use a reconstructive procedure that was reliable, would heal quickly and allow the patient to regain her quality of life.
CONFLICT OF INTEREST STATEMENT
None declared.



