-
PDF
- Split View
-
Views
-
Cite
Cite
Stephen Obidike, Akeh Woha, Fuad Aftab, Fused ureters in patient with horseshoe kidney and aortic abdominal aneurysm, Journal of Surgical Case Reports, Volume 2014, Issue 11, November 2014, rju113, https://doi.org/10.1093/jscr/rju113
Close - Share Icon Share
Abstract
Horseshoe kidney (HSK) is a very common developmental abnormality in the kidney. They are associated with abnormalities like multiple renal arteries, abnormal position of the ureter in the renal pelvis and highly placed ureteropelvic junction. These can result in urological complications. However, the ureters run their separate course and empty individually into the urinary bladder. Surprisingly, anatomical anomalies do occur and can lead to unexpected findings on investigation or surgical treatment. Such anomalies can present diagnostic and management challenges to unsuspecting clinicians. This report deals with one of such anomalies that seem not to have been reported before in the literature. This case is a rare finding of fused ureters over the renal isthmus in a patient with HSK who also has aortic abdominal aneurysm (AAA). Simultaneous occurrences of HSK and AAA have been reported severally in the past, and the authors are paying attention on the ureteral anomaly.
INTRODUCTION
Horseshoe kidney (HSK) is the most common renal developmental abnormality occurring at the metanephric stage of the renal embryonic development resulting in the poles of both the kidneys fusing together [1–3]. Fusion is usually at the lower poles resulting in the kidneys been caught at the level of the developing inferior mesenteric artery [1, 2]. However, in ∼0.17–0.25% of cases, the fusion occurs at the upper pole resulting in an inverted horseshoe [1–4].
No racial preferences have been noted in the occurrence of HSK and the male-to-female ratio is 2 : 1 [3, 4]. Most HSKs are diagnosed on routine radiological investigation, but there is high incidence of injury to them from blunt abdominal trauma. Anatomically, HSK involves three main anomalies; changes in vascular supply, rotation and abnormal position [2]. The uretopelvic junction has been reported to be higher in HSK patients and their ureters also enter at a higher level into the renal pelvis, which may result in increased incidence of urinary complications [1–3]. However, the ureters usually run their individual course and empty into the urinary bladder.
In the literature, there are reports of HSK patients having bilateral ureteral duplication, crossed, single ureter, ectopic ureter, retrocaval ureters and triple ureter [1–6]. However, the authors of this case report did not come across any literature that reported fusion of both ureters at any point in its course down to the urinary bladder in a patient with HSK. In this article, the authors wish to report a case of fused ureters in a patient with HSK and aortic abdominal aneurysm (AAA).
CASE REPORT
This is a case of a 75-year-old lady referred to the emergency department by her community doctor due to 2 days history of epigastric pain and nausea not responding to antacids and proton pump inhibitors. She has a background history of HSK, AAA (last abdominal ultrasound 6 months prior to presentation showed the AAA measured 5 cm), hyperthyroidism for over 50 years, cholecystectomy ∼20 years ago and Helicobacter pylori infection. She smokes ∼10 cigarettes a day for over 30 years and her brother have had AAA repair.
On examination she was found to be euthyroid with a pulsatile mass in the abdomen, easily palpable around the paraumbilical region. There were decreased femoral pulse with no popliteal or pedal pulses on the right lower limb, whereas there were normal femoral and popliteal but no pedal pulses on the left lower limbs on both palpation and hand-held Doppler. Aside from these, other systems were unremarkable.
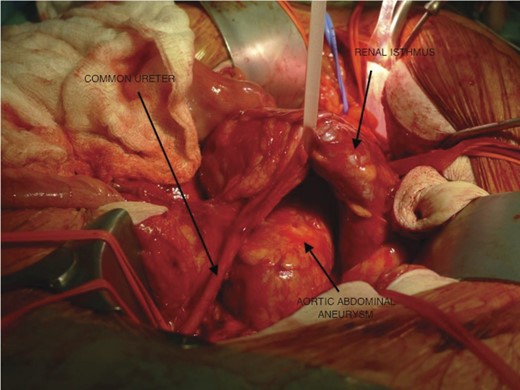
Computed tomography scan done revealed bilobed juxtarenal AAA measuring ∼6.7 cm in transverse diameter, but no leaks or ruptures were reported. An open AAA repair was done and a HSK was found with both ureters uniting over the renal isthmus forming a common ureter that continued down to the urinary bladder (Figs 1–6). Although the patient died from complications of the surgery, the authors wish to discuss the presence of fused ureters in a patient with HSK.
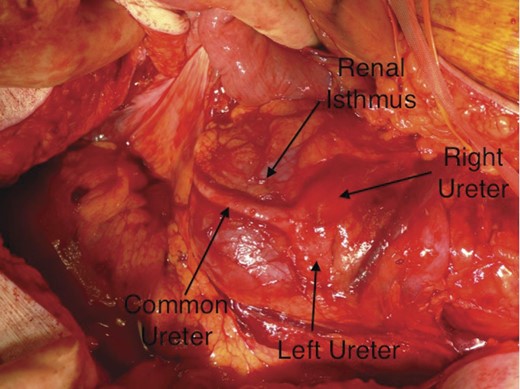
The left and right ureters running over the renal isthmus and fusing to form a common ureter.
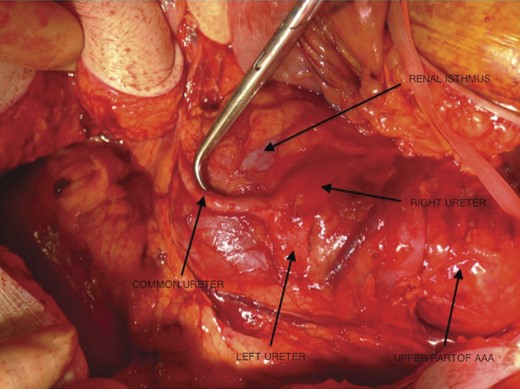
The upper part of the aortic aneurysm, the left and right ureters running over the renal isthmus and fusing to form a common ureter (been pushed by the surgical instrument).
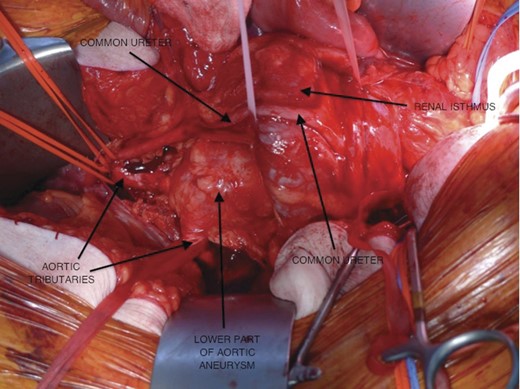
The lower part of the aortic aneurysm with some tributaries from the aorta, the left and right ureters running over the renal isthmus and fusing to form a common ureter.
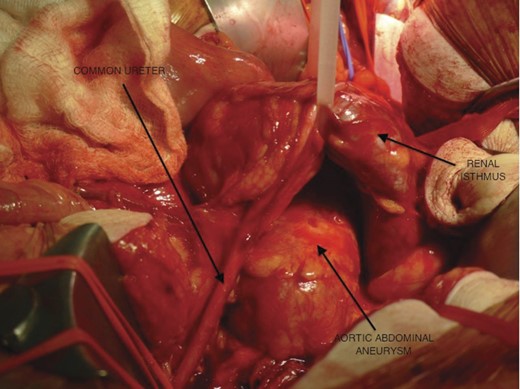
The renal isthmus been pulled up to expose the aneurysm with the common ureter running into the pelvis.
The renal isthmus been pulled up to expose the aneurysm with the common ureter deviated to the right side on its way to the pelvis.
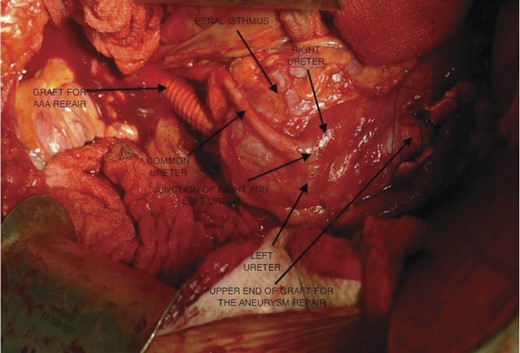
The lower part of the aorta with a graft inserted into the aorta, sticking out slightly above the renal isthmus; the left and right ureters running over the renal isthmus and fusing at a junction to form a common ureter.
DISCUSSION
HSK occurring at same time with AAA is rare. It has been seen in ∼0.12% of cases [2, 4]. Pubmed reported 176 cases between 1956 and 1999 [2]. However, there has never been any report of fusion of the ureters in HSK patients in the literature. HSK occurring without any other anatomical abnormality may lead to complications such as increased vesicoureteric reflux, increased risk of infection, renal insufficiency, stricture and increased rate of calculi formation especially staghorn calculi [1–7, 8].
Raj et al. (2004) reported that 20% of HSK have associated renal calculi due to high insertion of the ureter in the renal pelvis with subsequent obstruction of the ureteropelvic junction leading to stasis. These patients were also found to have hypovolaemia and hypercalciuria [9]. The authors think that the presence of fused ureters in HSK patients may further increase the chances of developing the complications.
Moreover, the authors are of the opinion that fused ureters may present further clinical challenges in the diagnosis of symptoms like subumbilical colicky abdominal pain without other symptoms of bowel obstruction. It will also have clinical implications as a single stone occluding the common ureter can cause hydronephrosis to both kidneys at same time.
Furthermore, it can present surgical challenge during open abdominal surgeries and caesarean section, especially if the clinician was not aware of its existence. In view of the fact that this is probably the first report of this case, it will be too early to advise intravenous pyelogram on all patients with HSK to evaluate the course of their ureters before surgery even if they have no urinary symptoms but such investigation may be considered if in doubt. The clinical significance of having a centrally located common ureter that drains directly into the bladder cannot be easily overlooked. It is worth noting that this anomaly can exist in patients with HSK and thus the clinician should be alert in thinking beyond the box in cases of unusual lower central abdominal pain that may not be easily explained by other common abdominal or pelvic pathologies.
CONFLICT OF INTEREST STATEMENT
None declared.



