-
PDF
- Split View
-
Views
-
Cite
Cite
Byung Seup Kim, Han Suk Ryu, Kyung Ho Kang, Sung Jun Park, Intrathyroidal parathyroid hyperplasia in tertiary hyperparathyroidism, Journal of Surgical Case Reports, Volume 2013, Issue 5, May 2013, rjt034, https://doi.org/10.1093/jscr/rjt034
Close - Share Icon Share
Abstract
We report herein a case of intrathyroidal parathyroid hyperplasia in a patient with tertiary hyperparathyroidism. The patient was recommended for parathyroidectomy due to sustained hypercalcemia after kidney transplantation. Preoperative radiologic evaluations showed a benign-looking thyroid mass and three enlarged parathyroid glands. Intraoperative intact parathyroid hormone (iPTH) level and frozen biopsy results indicated a missed parathyroid gland after immediate subtotal parathyroidectomy. Then, a secondary partial resection of thyroid including the thyroid nodule was performed. An excised intrathyroid nodule was diagnosed to be parathyroid hyperplasia by frozen biopsy, and intraoperative iPTH level abruptly decreased. A benign-looking thyroidal mass in patients with secondary or tertiary hyperparathyroidism should be carefully evaluated considering the possibility of an intrathyroidal parathyroid hyperplasia.
INTRODUCTION
Parathyroidectomies to manage hyperparathyroidism are difficult in cases where the parathyroid gland is located in an uncommon site. The site of the inferior parathyroid glands varies between patients because of their descent through the neck with the thymus during embryological development [1]. We report a case of intrathyroidal parathyroid hyperplasia in a patient with tertiary hyperparathyroidism.
CASE REPORT
A 41-year-old female with a 13-year history of hemodialysis for chronic renal failure underwent a kidney transplant in May 2011 without complications or rejection reactions. Blood tests performed prior to the kidney transplantation indicated that serum total calcium (Ca) and intact parathyroid hormone (iPTH) level were 9.9 mg/dl (normal, 8.2–10.4 mg/dl) and 453.3 pg/ml (normal, 14–72 pg/ml), respectively. Postoperative laboratory tests performed three months later revealed elevated serum Ca (10.4 mg/dl), which lasted for 15 months. Her iPTH level did not return to normal after kidney transplantation (Fig. 1). The patient was diagnosed with tertiary hyperparathyroidism and was recommended for surgery.
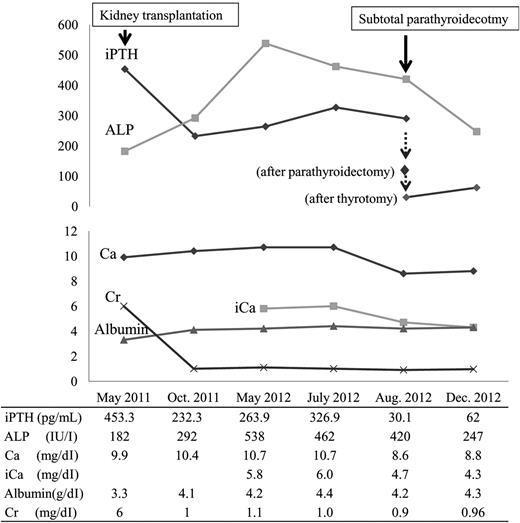
Serum intact parathyroid hormone (iPTH), alkaline phosphatase (ALP), calcium (Ca), ionized calcium (iCa), albumin and creatinine (Cr) levels from kidney transplantation to subtotal parathyroidectomy.
In the preoperative evaluation, two-hour-delayed 99mTc-sestamibi scintigraphy showed increased uptake in both inferior parathyroid glands (Fig. 2). Computed tomography (CT) of the neck showed a calcified nodule posterior to the right superior thyroid gland, a solid nodule in the right lower thyroid gland and an enlarged parathyroid gland posterior to the left inferior thyroid (Fig. 3). Sonography (SONO) showed a benign-looking nodule in the right lower thyroid and two adjoining enlarged parathyroid glands posterior to the left lower thyroid (Fig. 4). The right mid-thyroid nodule appeared benign, and a fine-needle aspiration biopsy was not performed. The right inferior parathyroid gland could not be identified in the CT or SONO findings. During neck exploration, four oval masses similar to parathyroid glands were observed (right superior: 1.7 × 1.0 cm, right inferior: 0.5 × 0.3 cm, left superior: 1.0 × 0.7 cm, left inferior: 0.8 × 0.6 cm). The left inferior parathyroid gland was partially preserved, while the other lesions were completely removed. Intraoperative frozen biopsy of the four masses revealed two cases of parathyroid hyperplasia, a parathyroid hyperplasia with a calcified nodule in the right superior area and a lymph node in the right inferior area. The right inferior parathyroid was not found during right neck exploration.
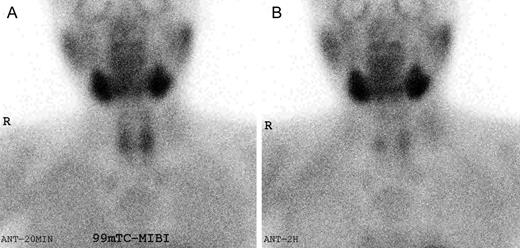
99mTc-sestamibi (MIBI) scintigraphy. (A) MIBI uptake in both thyroid areas 20 min after MIBI injection. (B) MIBI uptake in both inferior parathyroids 2 hours after MIBI injection.
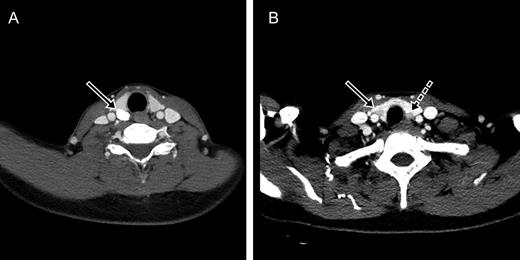
Parathyroid glands and the thyroid nodule on computed tomography. (A) A calcified nodule posterior to the right superior thyroid (arrow). (B) A solid nodule in the right lower thyroid gland (arrow) and an enlarged parathyroid gland posterior to the left inferior thyroid (dotted arrow).
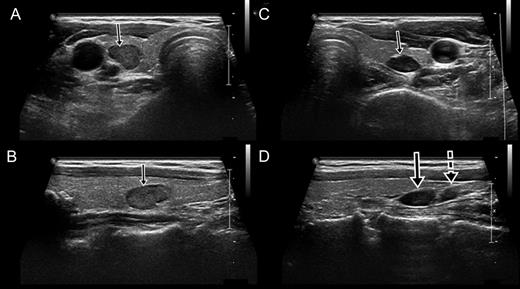
Sonography showed the right parathyroid gland within the thyroid and the adjoining left parathyroid glands. (A) Transverse view of the right parathyroid gland within the thyroid (arrow). (B) Longitudinal view of the right parathyroid gland (arrow). (C) Transverse view of the left superior parathyroid gland. (D) Longitudinal view of the left superior (arrow) and inferior (dotted arrow) parathyroid glands. The left superior parathyroid had migrated to an inferior position.
Intraoperative iPTH levels 20 min after the parathyroidectomy were still elevated (102.6 pg/ml). A small and soft nodule (12 mm diameter) was palpable in the lower pole of the right thyroid lobe. A partial resection of thyroid including the nodule was performed (Fig. 5). Intraoperative frozen biopsy of the intrathyroidal nodule revealed parathyroid hyperplasia (Fig. 6). Intraoperative iPTH levels decreased 20 min after the thyrotomy (30 pg/dL). After surgery, the patient's serum Ca and iPTH levels returned to normal, and renal function was well maintained.
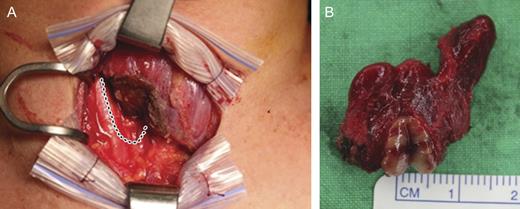
The resected thyroid. (A) Dotted lines show the right lower thyroid contour before resection. (B) Split intrathyroidal parathyroid gland.
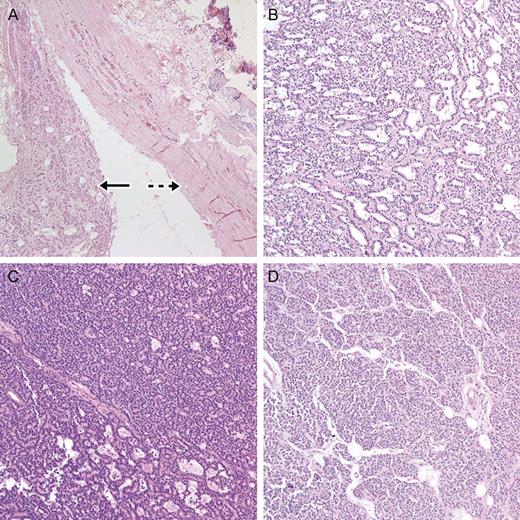
Microscopic finding from the parathyroid glands. (A) Right superior parathyroid hyperplasia (arrow) with a calcified nodule (dotted arrow) (H&E stain ×100). (B) Left superior parathyroid hyperplasia (H&E stain, ×200). (C) Right inferior parathyroid hyperplasia (H&E stain, ×200) was within the thyroid. (D) Left inferior parathyroid hyperplasia (H&E stain, ×200).
DISCUSSION
There are some case reports of pathologic intrathyroidal parathyroid glands causing primary hyperparathyroidism. Roy et al. reported that the incidence of an intrathyroidal parathyroid adenoma among ectopic parathyroid adenoma is 18% [2]. This phenomenon is seen less commonly in patients with secondary or tertiary hyperparathyroidism. There are few reports about intrathyroidal hyperplasia in secondary hyperparathyroidism [3, 4]. Low et al. reported intrathyroidal hyperplasia in 9% (1 patient) of recurrent hyparparathyroidism (11 patients) among patients who underwent parathyroidectomy to correct secondary hyperaparathyroidism [4]. The indication for surgery is secondary hyperparathyroidism, which cannot be managed with medical therapy and persists >6 months. Therefore, parathyroidectomy is performed less often for treatment of secondary hyperparathyrodism. The lack of case reports prevents calculation of the incidence of intrathyroidal parathyroid hyperplasia in secondary or tertiary hyperparathryoidism.
Intrathyroidal parathyroid adenoma or hyperplasia is an occasionally overlooked cause of surgical failure in hyperparathyroidism. There have been some efforts to preoperatively identify pathologic intrathyroidal parathyroid glands. Grisel et al. reported that an intrathyroidal parathyroid adenoma was accurately located using a sestamibi scan and ultrasonography [5]. Although sestamibi scan and ultrasonography were performed in our case, we did not identify the intrathyroidal parathyroid hyperplasia preoperatively. The accuracy of a sestamibi scan for identifying the location of multiple hyperplasia is decreased compared with that of a single adenoma. When the superior parathyroid gland is enlarged, the superior parathyroid gland migrates posteriorly and inferiorly, leading to an appearance of higher uptake in the inferior location [6]. In our case, the left superior enlarged parathyroid had migrated to an inferior position, and the left superior and inferior parathyroids looked like a single lesion on the preoperative CT. We thought that both migrated superior parathyroid glands appeared to be inferior parathyroid glands on preoperative sestamibi scan.
Abdo et al. performed thyroid venous sampling prior to lobectomy to identify a pathologic intrathyroidal parathyroid gland [7]. Heller et al. proposed specific ultrasound criteria to facilitate the preoperative diagnosis of intrathyroid parathyroid adenoma [8]. Ing et al. used diagnostic fine-needle aspiration biopsy on an intrathyroidal parathyroid gland [9]. These efforts are not commonly used. It is known that intraoperative iPTH monitoring is a good predictor of a successful parathyroidectomy in secondary hyperparathyroidism [10]. In our case, we knew that immediate parathyroidectomy had failed though intraoperative iPTH monitoring and frozen biopsy. We then confirmed the presence of a hyperfunctioning, intrathyroidal parathryoid gland with iPTH monitoring and frozen biopsy. When intraoperative iPTH monitoring was combined with a preoperative evaluation including a sestamibi scan, SONO and CT, the detection of intrathyroidal parathyroid was possible in tertiary hyperparathyrodism without specific procedures.
In conclusion, a benign-looking thyroidal mass in patients with secondary or tertiary hyperparathyroidism should be carefully evaluated considering the possibility of an intrathyroidal parathyroid gland. When the intraoperative iPTH level does not show an abrupt decrease after standard parathyroidectomy, the thyroid mass should be considered an investigated lesion.



