-
PDF
- Split View
-
Views
-
Cite
Cite
Basmah A. Rafie, Omar J. AbuHamdan, Nawal S. Trengganu, Intraluminal migration of retained surgical sponge as a cause of intestinal obstruction, Journal of Surgical Case Reports, Volume 2013, Issue 5, May 2013, rjt032, https://doi.org/10.1093/jscr/rjt032
Close - Share Icon Share
Abstract
Despite near-universal implementation of protocols for surgical sponges, instruments and needles, incidents of retained surgical foreign bodies (RSFB) continue to be a significant patient safety challenge. We report a case of a 29-year-old woman who presented with small intestinal obstruction caused by complete intraluminal migration of a retained surgical sponge into the intestine 9 months after cesarean section. The diagnosis was confirmed by plain abdominal radiograph. The patient underwent exploratory laparotomy, sponge removal and became completely asymptomatic. Although safety standards for hospital employees have been developed during the past decades, no detection system to date has been evaluated as a replacement for traditional manual counting protocols and procedures. The best approach is the prevention of this condition, which can be achieved by implementation of standardized institutional regulations and strict adherence to them. Perhaps, with increasing use of the new technologies as adjunct to the counting, the incidence of RSFB will fall dramatically.
INTRODUCTION
Retained surgical sponge or gauze is also known as gossypiboma, meaning a mass within the body composed of a cotton matrix surrounded by a foreign body reaction. It is the most frequently encountered retained foreign body after open abdominal surgery [1]. It is rarely reported due to medico-legal implications. True worldwide incidence is unknown. However, a recent study estimated the incidence of retained surgical foreign bodies (RSFB) as 1 in 5500 operations [2]. Although a broad spectrum of gastrointestinal complications have been reported in the literature, intraluminal migration of a retained surgical sponge is considered rare [3]. The aim of this article is to report our personal experience of such a rare case, presenting features, and how to avoid such complications.
CASE REPORT
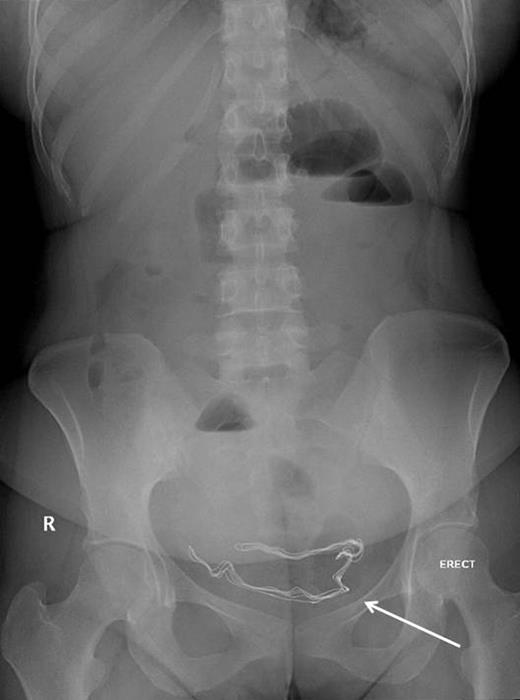
29-year-old woman was referred by her gynecologist with a history of diffuse colicky abdominal pain, nausea, repeated vomiting, constipation and progressive abdominal distention for 7 days prior to hospitalization. She had undergone an emergency cesarean section 9 months previously at a private hospital and since that time she had been complaining of recurrent attacks of nonspecific abdominal pain and occasional episodes of vomiting especially after heavy meals from which she had lost 10 kg since delivery. The patient had attended emergency departments at different institutions with similar complaints and had been discharged home after each occassion, but her symptoms passed undiagnosed. Five days prior to admission, abdominal roentography was done at an emergency department for her abdominal complaint, which showed radio-opaque density in the pelvis (Fig. 1), but it was mistakenly overlooked and she was discharged home with a diagnosis of nonspecific abdominal pain.
Upon admission, she was afebrile, vitally stable, and her abdomen was distended and tympanic. Bowel sounds were increased in frequency and pitch. Digital rectal examination showed normal-colored stool. Laboratory investigations showed a white blood cell count of 10 700 cells/ml and a sodium level of 123 mmol/l, while other biochemical parameters were within normal limits. Abdominal roentography revealed dilated small intestinal loops with a finding of a radio-opaque density in the abdomen (Fig. 2). A diagnosis of small intestinal obstruction most likely caused by retained surgical sponge was made. On abdominal exploration, the small intestine was dilated down to the ileum with an intraluminal mobile mass felt in the distal ileum (Fig. 3). Before proceeding for mass removal, at around 80 cm from the duodenojejunal junction, there were two adjacent segments of the jejunum adherent to each other and both were adherent to the peritoneal wall by fibrous adhesions. Consequently, adhenolysis, enterotomy and removal of the mass, which was manually pushed there (Fig. 4), followed by resection and anastomosis of the compromised jejunal segment, were achieved. The foreign body was found to be retained surgical sponge (Fig. 5). However, apart from the isolated area of adhesion, exploration of the rest of the abdominal cavity did not show any lesions in the peritoneal cavity or perforation or fistula or pelvic collection. The authors concluded that the transluminal migration of the sponge most likely occurred from that adherent part of the jejunum. The postoperative period was uneventful and the patient was discharged on the seventh day of her hospitalization in good condition.

Proximal small intestinal dilatation with the radio-opaque mark migrated proximally to the abdomen (arrow), indicating its mobile nature.
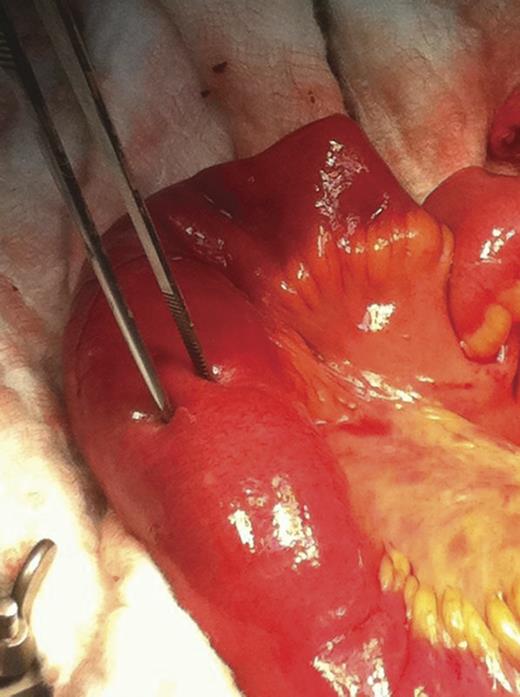
Intraluminal foreign body visible at the ileum with an intact normal wall (forceps).

Intraoperative removal of the foreign body from the jejunum (arrow).

DISCUSSION
Pathologically, there are two types of foreign body reactions in gossypibomas described in the literature. One of them is an aseptic fibrous response resulting in adhesion, encapsulation and granuloma. This form usually remains asymptomatic or causes chronic progressive symptoms over months to years. The other is an exudative reaction leading to cyst or abscess formation. Symptoms of this type are more severe and they clinically present earlier [1]. In rare instance, a surgical sponge may completely migrate into the intestinal lumen without any apparent opening in the intestinal wall [4].
Various hypotheses have been proposed to explain how the presumed transvisceral migration of such a foreign body might occur. A hypothesis based on experimental study proposed four stages in the process of migration. Initially, it is foreign body reaction, when the sponge is walled off by the omentum and some loops of intestine. Followed by secondary infection, when cotton filaments reach the intestinal lumen, cytolysis occurs. Then invasion of the sponge into the lumen occurs at the stage of mass formation. Finally, is the remodeling stage, when a fibrotic scar is formed at the site of migration [5].
Patil and colleagues suggested that an increased pressure of the intra-abdominal mass on the bowel loops can lead to necrosis of the intestinal wall partially or entirely. Consequently, this process can lead to fistula or obstruction [6].
More is being discovered about the risk factors associated with increased incidence of RSFB; emergency, prolonged surgical procedure, unplanned change in the course of a surgical procedure, involvement of more than one surgical team and patients with higher body-mass index [7, 8].
Multidisciplinary approaches and new technologies may help reduce this low-frequency but clinically significant event. Surgical counting technique, radiographs of the anatomic region corresponding to the operative field and, more recently, specialized radio-frequency (RF) system consisting of an RF detector and RF labeled surgical sponges. However, there are no known methods of them entirely eliminating the occurrence of RSFB [8]. Different hospitals utilize different methods to account for the surgical materials that are placed in the body. Meticulous counting and routine use of surgical textile materials that should be impregnated with radio-opaque markers, in addition to thorough exploration of the surgical sites at the conclusion of the operation, should reduce the incidence of RSFB. Unfortunately, 88% of RSFB cases occur after ‘correct’ surgical counts, indicating that manual counting alone is not a reliable mechanism in eliminating RSFB [7].
Although intraoperative roentgenograms are not routinely required, a cost-effectiveness analysis of routine radiographs after emergent operations found that intraoperative radiography was both less costly and more effective than the traditional counting strategy because of institutional costs and legal fees associated with retained surgical sponges [9].
A modern technological advance designed a specialized RF system to eliminate errors in the sponge count by removing the human error factor. The sensitivity and specificity of RF device technology were found to be much higher than those of surgical sponge counts or published findings on the use of intraoperative radiographs to identify retained surgical sponges [10].
CONSENT
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Conflict of interest
The authors declare that they have no conflicting interest and have not been supported or funded by any drug company.



