-
PDF
- Split View
-
Views
-
Cite
Cite
Patrick Tomasetti, Christine Jacbosen, Thomas Gander, Wolfgang Zemann, Emergency decompression of tension retrobulbar emphysema secondary to orbital floor fracture, Journal of Surgical Case Reports, Volume 2013, Issue 3, March 2013, rjt011, https://doi.org/10.1093/jscr/rjt011
Close - Share Icon Share
Abstract
Orbital floor fractures are generally the result of blowout orbital and may be associated with orbital emphysema leading to proptosis and even to loss of vision. A 49-year-old woman fractured the orbital floor in a fall. After blowing her nose, she developed exophthalmos and severe reduction in vision. She consulted our department and underwent emergency surgical management with orbital drainage. Decompression led to immediate resolution of the exophthalmos and postoperative improvement in visual acuity. Urgent decompression is indicated by the presence of proptosis, elevated intraocular pressure, and progressive loss of vision in cases of orbital trauma with additional emphysema. Surgical treatment of tension emphysema includes lateral canthotomy or cantholysis, needle aspiration, transconjunctival, or lateral blepharoplasty approach, and bone decompression depending on the severity of the case. Sneezing or blowing the nose can lead to proptosis and decreased visual acuity secondary to trauma to the orbit. Under such circumstances, emergency decompression is essential.
INTRODUCTION
Orbital floor fractures are generally the result of blowout orbital trauma or severe facial injury. Orbital emphysema is the abnormal presence of air in the orbit and periorbital tissues, and tends to develop in fractures affecting the paranasal sinuses and orbital walls. Predisposing factors include sneezing, coughing, nose blowing and air travel. The air passes through mucosal sinus lacerations into the orbital space and can induce elevation in the intraorbital pressure with consequent proptosis.
Most cases are benign and resolve spontaneously. However, patients must be followed closely for potential complications. Patients developing acute orbital compartment syndrome with central retinal artery occlusion and loss of vision require rapid decompression.
This article presents a rare case of orbital floor fracture, which required an emergency surgical approach when posttraumatic tension retrobulbar emphysema developed which was exacerbated by nose blowing.
CASE REPORT
A 49-year-old woman was referred to our department of Oral and Maxillofacial Surgery with a history of blunt trauma in the region of the left eye incurred in a fall 1 day earlier. As there was no functional disturbance, she did not seek medical help initially. The next day, while blowing her nose she developed swelling, pain and progressive loss of vision. Physical examination revealed severe left-sided exophthalmos, accompanied by palpebral and orbital swelling and subconjunctival hematoma. Eye movement in all directions was painful. There was no diplopia at the first ophthalmological evaluation, but a loss of visual acuity of 6/10, accompanied by severe proptosis and increased intraocular pressure (IOP) were indications for rapid surgical treatment.
Spiral computed tomography (CT) was performed using 1 mm slices with a soft tissue and bone algorithm. A non-dislocated orbital floor fracture and a large amount of intraorbital emphysema were found, especially retrobulbar between the ocular muscles and around the optic nerve, causing exophthalmos (the distance from the corneal apex to the line connecting orbital rims was 18.8 mm; normal 9.0 mm) (Figs 1–2).
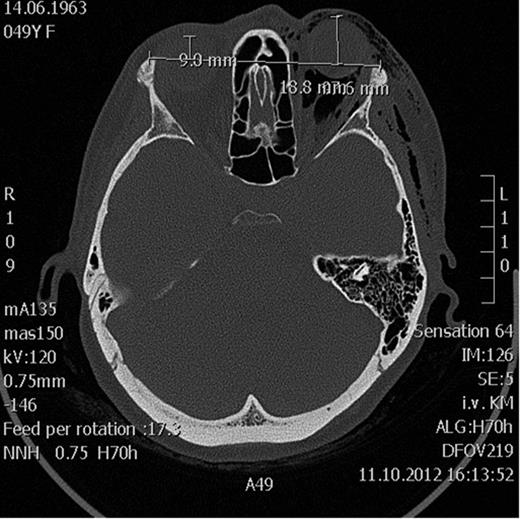
Axial CT scan showing massive emphysema of the orbit leading to proptosis.
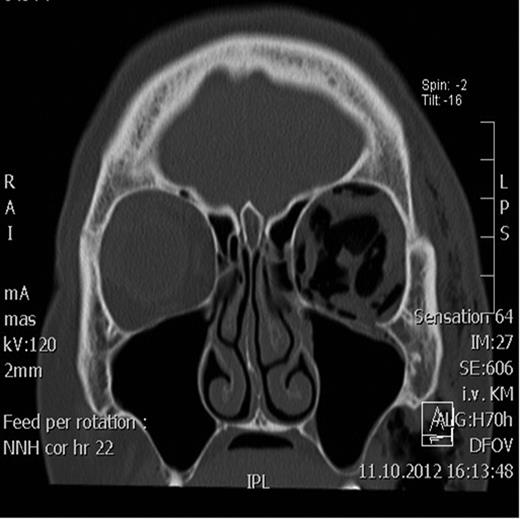
Coronal CT scan showing the retrobulbar emphysema prior to decompression.
Owing to the clinical findings and the severity of the symptoms, surgical decompression was performed under general anesthesia. Lateral blepharoplasty and transconjunctival incisions were made (Fig. 3). The left orbital floor was exposed, revealing a non-dislocated bone defect, without herniation of the periorbital tissue. The surgical management with orbital drainage produced excellent results, with sudden resolution of the proptosis and a postoperative improvement in visual acuity, confirmed by further ophthalmological evaluation (Figs 4–5). The patient was put on amoxicillin and clavulanic acid every 8 h, and advised not to blow her nose vigorously and to use a nasal decongestant.

Patient after emergency decompression using blepharoplasty incison.
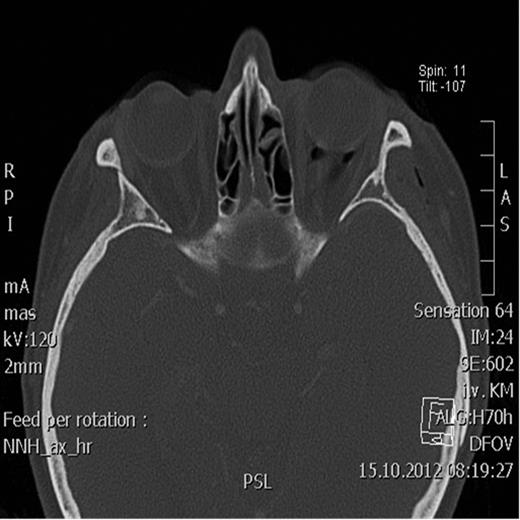
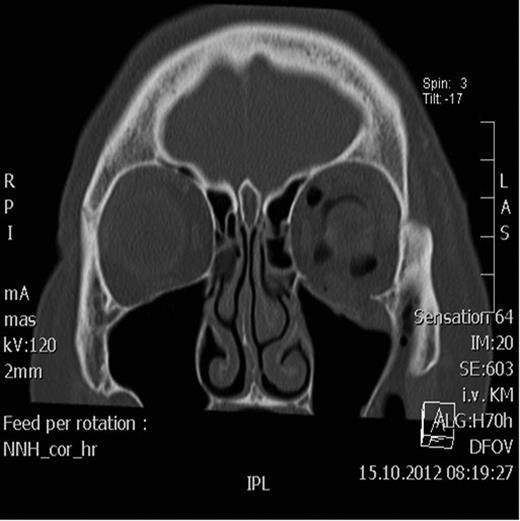
Postoperative axial CT scan showing normal position of the bulbus.
Two days after surgery, the patient was discharged with restored visual acuity and continuing resolution of the left periorbital swelling and proptosis.
DISCUSSION
Orbital emphysema is the abnormal presence of air within the fascial layers of the orbit. About 63% of cases occur as a result of blunt orbital or facial trauma, involving the paranasal sinuses and orbital walls [1]. Other infrequent sources of intraorbital air include postoperative complications, infection, esophageal rupture, spontaneous pneumothorax and barotrauma [2, 3]. Emphysema usually appears in the periorbital area, rather than within the orbit itself.
In this case, the increased intraorbital pressure followed by intrabulbar hypertension may have caused occlusion of the central retinal artery and optic nerve ischemia (particularly, if the intrabulbar pressure exceeded 65–70 mmHg), which may result in a transient or permanent loss of vision [4]. It is usually associated with sneezing, nose blowing and coughing, which increase the pressure inside the nasal cavities and force air through sino-orbital communication into the orbit. After the air enters, orbital tissue can occlude the bony breach and act as a one-way valve across the fracture site permitting air to enter but not to leave the orbit [5].
There have been some reports of spontaneous orbital emphysema after forceful nose blowing, sneezing or coughing, with no antecedent facial trauma, often as a result of rupture of the lamina papyracea (orbital lamina) [6, 7].
The diagnosis of orbital emphysema is usually made from the history alone, with sudden periorbital swelling and closing of the eyelids on the affected side, supported by the results of physical examination (crepitation, tenderness, pain and ecchymosis) and confirmed by orbital CT.
Orbital emphysema without impaired vision usually resolves spontaneously within 2 weeks. During this time, patients should avoid blowing their nose, sneezing and activities that lead to increased pressure in the nasal cavity [8]. Conservative non-surgical approach includes treatment with antibiotics and antiinflammatory drugs, and high-dose cortisone in cases of ophthalmoplegia with increased IOP.
Orbital infection, such as cellulitis, is a rare complication and is associated with concomitant sinusitis or the penetration of infected nasal secretions into the orbital space [9].
Surgical treatment of tension emphysema includes lateral canthotomy or cantholysis, orbital decompression via needle aspiration, transconjunctival or lateral blepharoplasty approach and bone decompression [1, 10]. Needle decompression is a simple, rapid technique, described by Lindberg, although potential complications require careful consideration, such as retrobulbar hemorrhage, scleral perforation and optic nerve damage.
Our case is a rare example of an orbital floor fracture complicated with orbital emphysema requiring an urgent surgical approach. The typical predisposing constellation was present, i.e. orbital wall rupture and Valsalva maneuver. The need for acute management is important as the systemic absorption of the air mass can take 7–10 days.
Urgent decompression was indicated by the presence of proptosis, elevated IOP and progressive loss of vision due to pressure on the central retinal artery and optic nerve [3]. We preferred to perform decompression via lateral blepharoplasty and transconjunctival approaches due to the retrobulbar localization of the air. This is more difficult to achieve with a needle without damaging important orbital structures (Fig. 3).
We administered prophylactic antibiotics and decongestants, but did not prescribe steroids, as the visual improvement was immediate and sustained after surgical intervention.
CONCLUSION
If tension emphysema occurs, the orbit must be decompressed to relieve the compressive effect of the air accumulation and reverse the potentially sight-threatening condition.



