-
PDF
- Split View
-
Views
-
Cite
Cite
Kandi Ejiofor, Surgical repair of a mandibular bony defect following the removal of an amelobalstoma, Journal of Surgical Case Reports, Volume 2013, Issue 1, January 2013, rjs028, https://doi.org/10.1093/jscr/rjs028
Close - Share Icon Share
Abstract
This case report describes a 35-year-old Caucasian radiographer who presented with a significant mandibular bony defect following multiple excisions of an ameloblastoma. As a result, there was an absence of teeth on the lower-right mandible and a clear defect in the mandible. The treatment objectives were to rebuild the mandibular defect, with a long-term view of inserting dental implants. In a novel approach outlined in this presentation, tissue expansion of the submucosa, a titanium construct and an iliac bone graft were used to rebuild the patient’s jaw. This surgical technique is recommended for the reconstruction of bony defects.
INTRODUCTION
Ameloblastomas are rare benign odontogenic tumours, most commonly found in a patient’s lower jaw. Although rarely metastatic, the growth of these lesions can result in defects in the jaw easily destroying surrounding bony tissues. For this reason, the treatment is often excision of the lesion, with wide excision margins, resulting in the absence of a part, or all, of the mandible. The surgical approach for correction of this mandibular defect is often reconstruction of the mandible in view of inserting dental implants at a later date. Despite surgical advancements, reconstruction of the jaw still remains a daunting challenge. Careful preoperative planning and precise execution are paramount to the success. At the moment, bone grafting with non-vascularized bone remains a good option where facilities for soft tissue flaps are not readily accessible [1]. Creating an effective wound closure and reducing the incidence of infection is an important stage in the success of the operation, and has been combated here by tissue expanding the submucosa, using Osmed pellets, prior to surgery. This is a relatively new technique to the mandibular region and has the potential to revolutionize the success of microsurgeries in this area.
In this report, I describe a woman who underwent a repair of her mandibular defect by a combination of innovative techniques, in order to reduce the risk of complications and get her back to an aesthetically pleasing level.
CASE REPORT
A 35-year-old lady presented to the craniofacial surgeons looking for a permanent fixture to the bony defect in her lower-right mandible. In 1991 she had her first operation to remove the ameloblastoma and then had it further excised 6 years later due to a reoccurrence. This resulted in an absence of teeth from the canines back and removal of bone down to the inferior alveolar nerve. The patient has since been clear of any further reoccurrences and wears lower dentures for aesthetic reasons.
She has no significant past medical history nor family history, nor does she have any known drug allergies. She does not smoke or drink alcohol.
On clinical examination, the patient experiences mild parasthesia in the distribution of her right inferior dental nerve, particularly the lateral aspect of the lower lip.
On examination, there is clear absence of teeth on the lower-right side from the canines back (to include the premolar, molar and wisdom teeth) and presence of healthy oral mucosa with laxity to move the submucosa medially. There is a loss of the vertical height of the posterior body of the mandible of about 50% and the vestigial remnants of the lingual plate are just palpable and visible on plain radiograph and CT. Scans show that the superior margin of the resection is well corticated under the inferior dental nerve (Fig. 1a and b). No functional problems exist. As a long-term solution to her defect, the patient wishes to get dental implants. The surgical approach taken, prior to the implants, shall be discussed.
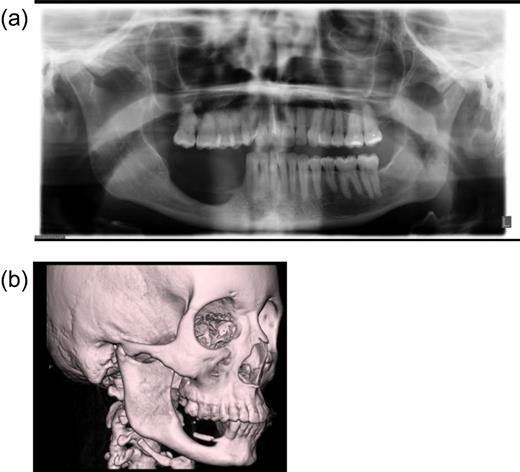
Imaging of the patient's mandibular defect pre-surgically. (a) Radiolocal image of patient's jaw. (b) CT scan of head
The patient was initially given the option between a bone graft or vascularized tissue (free fibular flap) and informed of the complications—a bone graft carries a risk of rejection and vascularized tissue needs an increased amount of post-operative care to ensure that the tissue remains vascularized. The patient was not keen on a free flap and given the fact that the bony deformity was <5 cm, non-vascularized iliac bone graft was deemed to be sufficient to carry out this operation [2].
The surgery occurred in several steps. The first step was achieving significant tissue expansion (>2 cm) using Osmed pellets, guided into the submucosa and kept over the alveolar ridge for several months (Fig. 2a–c).
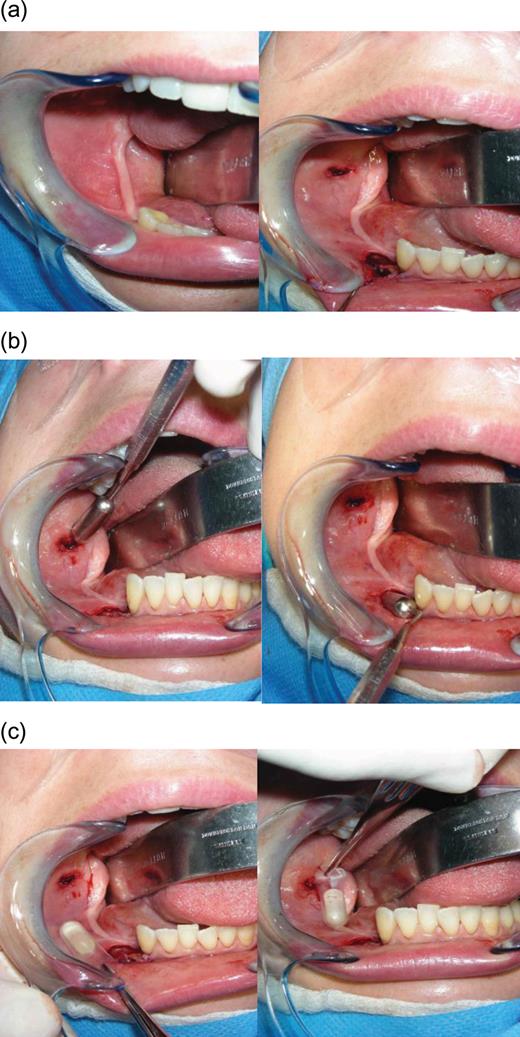
Image of patient's oral cavity during insertion of Osmed pellets. (a) Incisions made in the submucosa. (b) Guides used to size the tunnel for the Osmed pellets. (c) Osmed pellets before insertion into the submucosa
Two months later, the patient underwent the main bulk of her operation. The Osmed pellets were removed from the subperiosteum (Fig. 3a and b) and the iliac bone graft was taken, made up of cortical and cancellous bone and placed to one side (Fig. 4a–c). An epidural catheter was placed inside the soft tissue of the graft site and left overnight. It had a continuous fusion of a local anaesthetic to improve post-operative pain and encourage early mobilization.
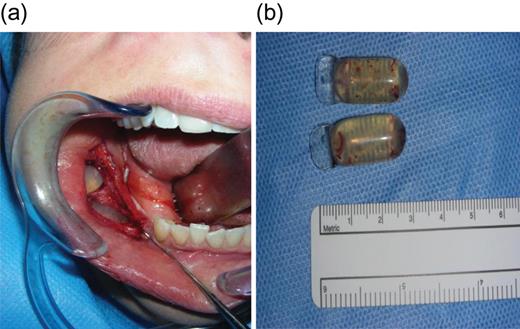
Submucosa after adequate tissue expansion. (a) Opening of submucosa to reveal Osmed pellets. (b) Size of Osmed pellets
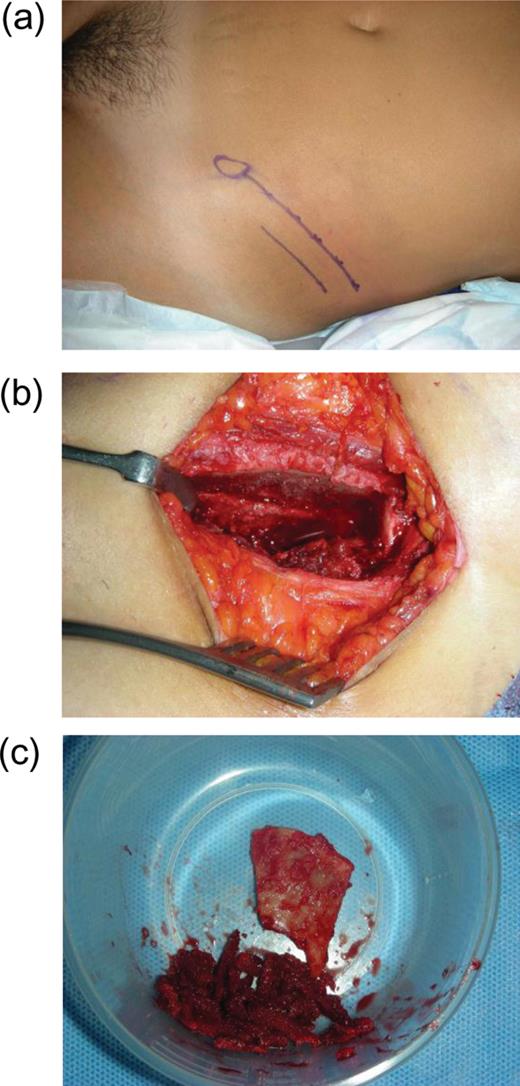
Autogenous iliac bone grafting. (a) Marking of bone graft incision site. (b) Open site where iliac bone graft is harvested from (c) cortical and cancellous iliac bone
Previously, using CT scans, a titanium construct was made to guide the outline of the bone graft and complete the missing height and width of the mandible [3]. Once fitted to the patients jaw, it was packed with the bone graft and screwed down into position (Fig. 5). A slight groove was made on the mandible to allow space for the inferior dental nerve to lay, so that the construct did not compact the nerve and cause functional problems.

Titanium construct packed with iliac bone graft and screwed into position on the lower mandible
To complete the surgery, the periosteum was sutured over the construct and then the buccal muscosa was sutured over again to form a double-layered closure (Fig. 6a–c).The purpose of this was to prevent infection and rejection, by ensuring that there was an increased distance between the foreign object (titanium construct) and the outside environment. The dental implants are scheduled to be inserted several months after this operation.
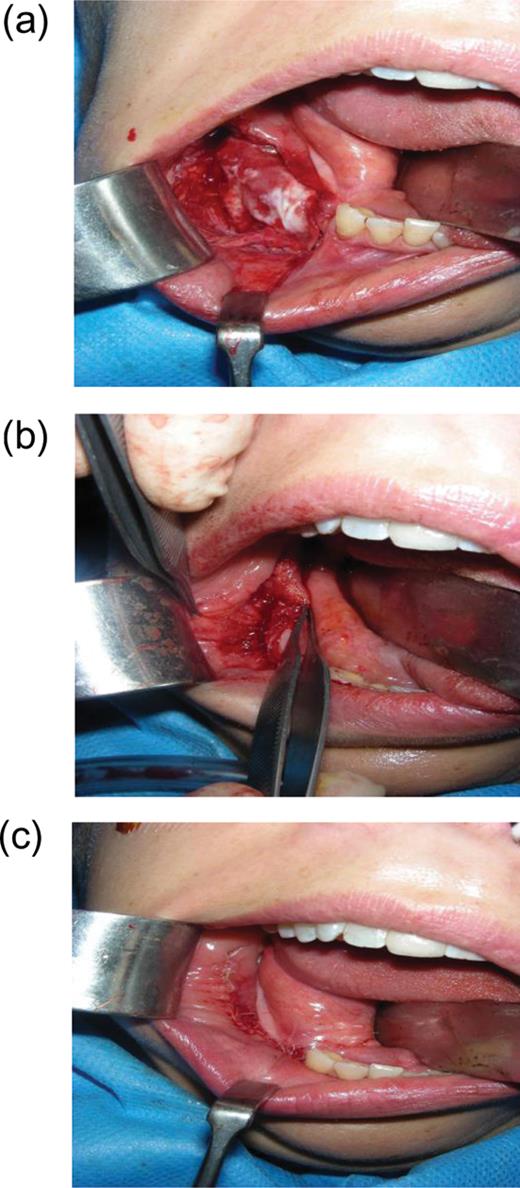
Image of patient's surgical site. (a) Tissue expanded submucosa is sutured close. (b) Buccal mucosa is sutured close. (c) Image of post-surgical site
DISCUSSION
Bony defects in the maxillofacial area are a huge problem in clinical orthodontics, caused by a wide range of injuries and diseases presenting as either cosmetic or functional defects and in some instances both. It is the importance of accounting for the anatomical, functional and aesthetic aspects that make the reconstruction so challenging. Often patients suffering from ameloblastomas undergo resection as treatment and are left with bony defects that require reconstruction. In this case, the intention was to realize an aesthetically pleasing appearance for the patient and it has been shown that bone grafting with subsequent dental implants is a successful method [4].
As in this case, it is recommended that non-vascularized autogenous bone grafting can be used when a two-layer watertight closure is attainable [5]. Sources of bone could have been harvested from either local or distant sites but in this case, an extra-oral site (iliac bone) was used as a moderate amount of bone was needed [6].
The surgery lasted 5 h and incorporated several novel techniques to improve the outcome of the operation.
The use of Osmed pellets was innovative, as pellets of this size have only recently been experimented on goats maxilla [7]. As well as allowing for space to put the construct, the pellets allowed for a tension-free closure. Otherwise, the result would have been a high-tension closure, leading to rapid breakdown of the graft providing an entrance for infection, a common complication occurring when titanium plates are exposed [8]. Advantages of the Osmed tissue expanders are that the material is safe with a low complication rate and low risk of infection due to small incision site and minimal trauma [9].
The titanium construct is another relatively novel approach and was invaluable in the success of this surgery, as it guided reconstruction of the mandible, allowing for dental implants to be put in at a later date. At present, an alloplastic material such as titanium is often used for mandibular reconstruction as it is resistant to corrosion, adaptable and biocompatible [10].
Although the insertion of dental implants is the end goal for this surgery, the importance of this case report is to highlight the novel techniques involved in making this surgery a success. The use of small Osmed pellets in the submucosa of the mouth to cause sufficient tissue expansion and create a tension-free closure, combined with the titanium construct packed with grafted iliac bone to rebuild the jaw was an approach recommended by the doctors for the repair of bony defects of <5 cm. I suggest prudent management of future cases post-operatively to ensure a continued success of the graft.
Acknowledgements
I would like to thank the following individuals for their participation in this case report: Mr Niall Kirkpatrick, Consultant Cranio-facial surgeon and Mr Jonathan Collier, Consultant Cranio-facial surgeon.



