-
PDF
- Split View
-
Views
-
Cite
Cite
Kenneth Hiew, Richard Glendinning, Nigel Parr, Manal Kumar, The twisted diversion: a paralyzing complication, Journal of Surgical Case Reports, Volume 2013, Issue 1, January 2013, rjs027, https://doi.org/10.1093/jscr/rjs027
Close - Share Icon Share
Abstract
Ileal conduit remains a widely used urinary diversion performed after radical cystectomy. However, complications of ileal conduits remain an important concern in urological surgery. We report a rare case of an ileal conduit stricture, which can have grim complications if unobserved during the operation. Following an initial operation of radical cystectomy and ileal conduit formation in France in 2011, an 80-year-old male travelled back to the UK after 4 months of general weakness and limb paralysis. Initial blood test shows life-threatening hyperkalemia and worsened renal function. Subsequent ultrasound KUB scan and loopogram revealed obstructive uropathy. The initial management includes intravenous antibiotics and bilateral nephrostomies were inserted to aid diversion of urine. A thorough surgical exploration revealed a twisted, fibrous mesenteric band adhered to the proximal part of the ileal conduit. Only one case report of ileal conduit stenosis was described many years after the procedure.
INTRODUCTION
Despite recent advancement in radiotherapy and molecular-related therapies, radical cystectomy remains the mainstay of treatment for muscle-invasive bladder cancer. The ileal conduit has been considered the standard urinary diversion method after cystectomy. Although technically easier to perform compared with continent reservoirs, ileal conduit has not been associated with lower complications. We report a case of a male patient with a recent 4-month history of cystectomy and ileal conduit, presented to the accident and emergency department with an ileal conduit stricture.
CASE REPORT
An 80-year-old gentleman presented to A&E department for general weakness and paralysis of all four limbs. His past medical history includes Type 2 diabetes mellitus, spinal stenosis at the level of L2/L3, L3/L4 and L5/S1. His drug history includes aspirin, simvastatin and omeprazole.
The initial diagnosis was thought to be Guillan–Barre syndrome. However, he denied any recent flu-like symptoms or dysphagia. He said that he had become unwell since his cystectomy operation 4 months prior to his attendance at A&E. He also denied any loin pain. On examination, his abdomen was soft, a draining ileal conduit stoma was observed, sensation and reflex at all limbs were intact, but motor power of all limbs was diminished.
His initial blood test shows the potassium level of 9.1 mEq/l, serum urea of 20.1 mM/l, creatinine of 521 µM/l. He was immediately treated with calcium gluconate 10%, insulin-sliding scale and salbutamol nebulisers. An ultrasound scan of the renal tracts was carried out and subsequently shows bilateral hydronephrosis. Computed topography of the head revealed no intracranial bleed or infarct for the cause of paralysis. Due to his worsened renal function, a loopogram was performed and showed a stricture 4 cm proximal to the skin opening of the ileal conduit (see Fig. 1).
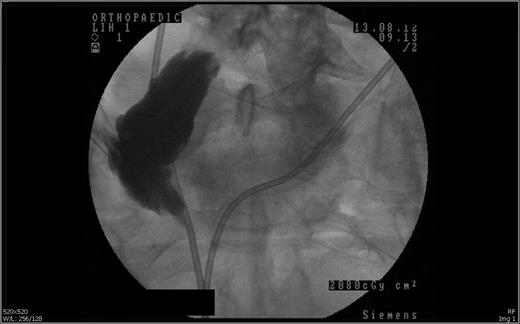
Loopogram revealed the stricture at 4 cm proximal to the skin opening of the conduit.
The patient was treated conservatively with 2 weeks of intravenous Ciprofloxacin antibiotics and nephrostomy tubes were inserted as a diversion. He underwent a laparatomy and revision of ileal conduit 2 months later. The surgical exploration revealed a small fibrous tissue band of mesenteric origin 4 cm proximal to the skin opening of the ileal conduit. The patient recovered uneventfully, his renal function improved remarkably and he was discharged back to community care after a stormy hospital stay.
DISCUSSION
Ileal conduit stricture has been described in a ∼2.5–8.5% at a median of 10 years after surgery [1]. In relation to our case, the phenomena occured 4 months after the procedure. Prior authors have suggested the occurrence of ileal conduit stricture is secondary to ischaemia which has resulted in severe transmural inflammation with submucosal fibrosis [2]. Magnusson et al. [3] used transmission electron microscopy to demonstrate a reduced height of microvilli, presence of glycocalyceal bodies and an increased number of lysosomes. Other hypotheses such as reaction to noxious agent in the urine, immune causation were also proposed.
Ileal conduit strictures can be investigated through three means: computed topography urogram, loopogram and looposcopy. Due to our patient's nature of renal failure, CT urogram is not feasible. A series of X-ray was initiated after contrast liquid was injected through the stoma. In our case, it showed a stricture 4 cm proximally to the skin opening of the ileal conduit.
Stenosis at the skin level can be managed by dilating the stoma opening, usually by inserting a lubricated digit down to the fascial layer for several minutes. The downside is patients may need frequent and repeated technique, and it also carries the small risk of forming false passage or opening [4]. In our case, the strictured conduit is at the fascial level that requires surgical exploration and revision.
Although ileal conduit stricture is rare, this potentially serious and life-threatening complication can be prevented with cautious surgical closure of abdomen. Stringent follow-up in stoma centre is also an essence to continuity of patient care. In the case described, the patient experienced significant morbidity in terms of re-admission to hospital, further surgical procedures and prolonged hospital stay. Consequently, surgeons should always be mindful of checking that the mesenteric pedicle is not twisted to avoid further perils during the postoperative period.
Acknowledgements
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare no support from any organization for the submitted work, no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
References
- ultrasonography
- hyperkalemia
- conduit implant
- renal function
- blood tests
- asthenia
- constriction, pathologic
- limb
- mesentery
- paralysis
- urinary diversion
- urologic surgical procedures
- ileum
- urine
- urinary tract obstruction
- percutaneous urography
- radical cystectomy
- ileal conduit procedure
- antibiotic therapy, intravenous
- exploratory surgery
- diversion procedure



