-
PDF
- Split View
-
Views
-
Cite
Cite
Aliyu M. Kodiya, Yusuf B. Ngamdu, Mala B. Sandabe, Abdullahi Isa, Hamman I. Garandawa, Solitary isolated neurofibroma of the soft palate, Journal of Surgical Case Reports, Volume 2013, Issue 1, January 2013, rjs029, https://doi.org/10.1093/jscr/rjs029
Close - Share Icon Share
Abstract
Neurofibroma of the soft palate is an unusual tumor and probably only two cases have been reported in English literature previously. Solitary isolated neurofibroma of the soft palate not associated with von Recklinghausen's disease is even more infrequent. To the best of our knowledge, this case represents the third reported in English literature. Complete surgical excision was achieved after tracheostomy due to envisaged difficulty in intubation. We present a 40-year-old man with an uncommon soft palatal neurogenic tumor.
INTRODUCTION
The exact cause of solitary neurofibroma remains unknown. It has been postulated that solitary neurofibroma is hyperplastic hamartomatous malformations rather than a neoplastic disease [1]. Neurofibroma is an uncommon benign neoplasm which originates from nerves that is composed of Schwann cells, perineural cells and fibroblasts. Soft palatal neurofibromas are rare and present with slowly growing painless mass [2]. Generally, neurofibromas present as either solitary mass or as part of neurofibromatosis syndrome or von Recklinghausen’s disease [3].
Neurofibroma is considered to be one of the most common neurogenic tumor but an uncommon intraoral neoplasm [4]. Its most common site is the skin presenting as multiple fibromata as part of syndrome of neurofibromatosis (von Recklinghausen’'s disease) or poliglandular syndrome multiple endocrine neoplasia (MEN) III [5]. Peak age of presentation is said to be third decade of life; however, its occurrence between 10 months and 70 years of age has been reported. Debilitating or immunocompromising diseases are not known predisposing factors [6] and sex predilection is contradictory [5].
Intra-oral neurofibromas may present as sessile nodule or pedunculated progressive but slow growing lesion. Often painless but may be painful due to pressure effects. Commonly seen on the tongue, may occur at any site like the palate (soft or hard), cheek mucosa, floor of the mouth [7] and in the mandible intraosseous location has been described [8].
We present a successfully treated 40-year-old man with symptomatic left-sided solitary isolated soft palatal neurofibroma.
CASE REPORT
A 40-year-old man referred to our clinic from a peripheral hospital with a 2-year history of lump in the throat. He developed muffled voice and some swallowing difficulties 5 months prior to presentation. About 2 months to presentation, he noticed rapid increase in the size of the lesion and pain. There was no history of respiratory difficulty or cervical swelling. He has never smoked cigarette nor take alcohol or its beverage.
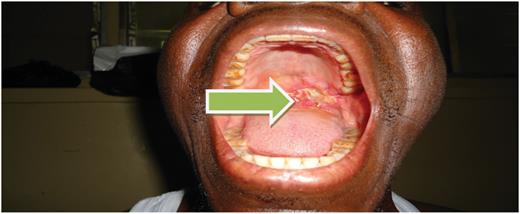
Physical examination revealed good oral hygiene, a pedunculated left-sided soft palatal mass ∼4 × 5 cm ulcerated on the medial surface, touching the tongue base and faucial pillars on the ipsilateral side but not attached to them. No contact bleeding was observed, and the rest of the mucosa appeared normal. There is no palpable significant cervical lymph nodes (Fig. 1).

Full blood count, electrolyte, urea and creatinine, urinalysis and chest X-rays were normal. Computerized tomographic scan revealed a mass in the oropharynx, non-contrast enhancing, no calcification and no bony involvement.
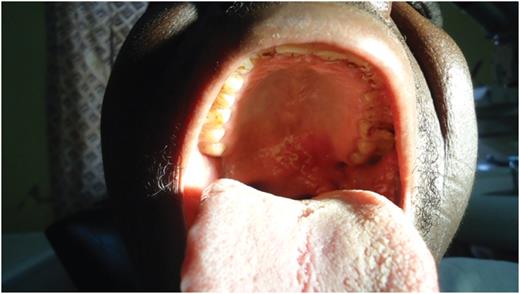
Examination under anaesthesia via tracheostomy confirmed our findings and tumour was completely excised. Histological examination revealed features consistent with neurofibroma with no evidence of malignancy. Post-operatively there has been sustained clinical improvement (Fig. 2). It is interesting to note that keeping follow-up appointments by patient is usually difficult in this part of the world, especially post-operative cases of benign or slow growing lesions. This is partly due to poverty and partly due to ignorance. Although our patient is in his 11th month post-operative, we saw him last 2 weeks after surgery (Fig. 3).
DISCUSSION
Neurofibroma is a benign neurogenic neoplasia rarely seen in the pharynx. It may be related to systemic disorders like MEN or neurofibromatosis syndrome (von Recklinghausen's disease), thus the importance of its accurate diagnosis. In this index case, it is an isolated solitary soft palatal disease not associated with any systemic pathology.
Complete surgical excision remains the gold-standard treatment for neurofibromas. Total surgical excision in the head and neck region may pose challenge to the surgeon due to infiltrative nature of the disease. Occasionally, such procedure may require sacrifice of vital structures leading to significant functional deficit or leave a cosmetic defect which increases the morbidity and mortality of the disease. Although intra-lesional excision will reduce morbidity, it is usually associated with recurrence [9, 10]. In our patient, we achieved complete excision without loss of function or a defect. Alternative to surgery is not readily feasible, for instance radiation therapy is not possible in diffused cases, however, in solitary plexiform type radiotherapy may retard growth and shrink the tumour [9].
Our patient presented with symptoms of dysphagia, muffled voice, rapid increase in size of the lesion and associated pain. We achieved complete symptom resolution with surgical excision of the tumor without need for any alternative therapy.
Oropharyngeal or soft palatal lesions should be excised completely where possible, this may reduce the frequency of surgery if histology confirm lesion to be benign. Tracheostomy as an adjunct to surgery is useful in large lesion like in our patient. This reduces anaesthetic difficulties and provide wider operation field for the excision. Continuous surveillance is necessary due to the relative risk of malignant transformation infrequently reported in some cases of radiotherapy-treated schwannomas [3].
Solitary isolated neurofibromas of the soft palate not associated with neurofibroma syndrome or systemic pathologies are uncommon. Complete surgical excision where possible remains the best treatment modality. Tracheostomy as an adjunct to surgery is safe and decreases anaesthetic difficulties.



