-
PDF
- Split View
-
Views
-
Cite
Cite
Kalimuthu Santhi, Ing Ping Tang, Ahamad Nordin, Narayanan Prepageran, Congenital cholesteatoma presenting with Luc's abscess, Journal of Surgical Case Reports, Volume 2012, Issue 12, December 2012, rjs026, https://doi.org/10.1093/jscr/rjs026
Close - Share Icon Share
Abstract
Congenital cholesteatoma (CC) rarely presents with Luc's abscess. As a result of widespread usage of antimicrobial agents, Luc's abscess is hardly encountered in current clinical practice. Herein, we report a case of Luc's abscess as the first presenting symptom in a 5-year-old boy with underlying CC. Patient's clinical findings, radiological investigations and treatment were also discussed.
INTRODUCTION
Congenital cholesteatoma (CC) can occur in any part of the temporal bone and the commonest site being in the middle ear, most probably due to its early presentation with conductive hearing loss [1, 2]. However, it only accounts for 2–5% of all cholesteatomas and 0.2–1.5% of all intracranial tumors [3]. The common presentation of CC is hearing loss, transient otorrhea, otalgia and ear fullness [3]. Rarely, it can present with mastoid sub-periosteal abscess especially in older children due to long-standing complications [4].
CASE REPORT
A 5-year-old boy presented with progressive left supra-auricular swelling for 2 weeks associated with left ear pain and low-grade fever. There were no complaints of ear discharge or hearing impairment by the child or parents. There was no recurrent ear pain before. Further history revealed no recent upper respiratory tract infection or trauma. Clinical examination showed a fluctuant mass measured 2 × 3 cm at the left supra-auricular region that was consistent with abscess. Otoscopic examination demonstrated mild edematous external auditory canal with intact tympanic membrane. There was a whitish mass seen medial to the tympanic membrane.
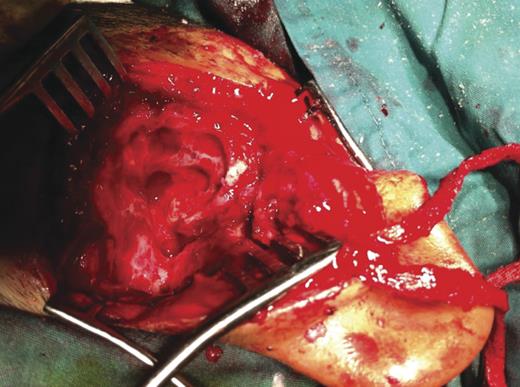
Tympanogram showed type B with failed auditory brainstem response on the affected side and normal hearing on the right side. High-resolution computerized tomography (HRCT) of temporal bone revealed soft tissue mass in middle ear cleft and ossicular destruction suggestive of cholesteatoma and Luc's abscess formation at left temporal bone (Fig. 1). Under general anaesthesia, surgical exploration through post-auricular incision confirmed lucs abscess. Further exploration of middle ear and mastoid cavity revealed cholesteatoma eroding all ossicles and involving mastoid bone. Modified radical mastoidectomy was done (Fig. 2). Postoperatively, patient recovered well without any complications.
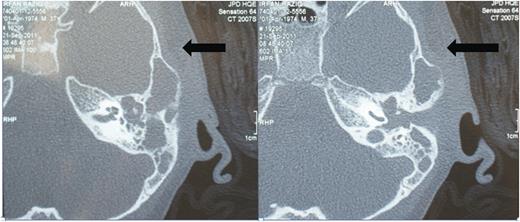
Pre-operative HRCT of left temporal bone. Axial image demonstrates Luc's abscess at left temporal region with soft tissue density and ossicular destruction.
DISCUSSION
CC is defined as cyst line by stratified squamous epithelium with keratin filled debris which is capable of surrounding tissue destruction as it expands [1]. This property of tissue destruction thought to be mediated by pressure-induced bone resorption and enzymatic dissolution of bone by cytokine-mediated inflammation [4]. In 1965, Derlacki and Clemis proposed criteria for CC as a cholesteatoma discovered behind an intact tympanic membrane with no history of otorrhea, prior otological intervention or previous perforations [5]. However, there are some exceptions to these criteria when patients presents with previous history of acute otitis media or as a suppurative complication of CSOM such as mastoiditis and sub-periosteal abscess [4, 6]. Therefore, underlying CC should always be suspected in children presenting with sub-periosteal abscess as a first symptom [4].
This fact is supported by Migirov et al. [4] who reviewed seven cases of CC patients presenting with mastoid sub-periosteal abscess. In our case, CC was not suspected as the cause for Luc's abscess due to its rare clinical presentation. The definite diagnosis of CC was established after a high-resolution computer tomography of temporal bone and confirmed by surgical exploration.
In pre-antibiotic era, Luc's abscess often presented as a complication of otitis media and its incidence since then has dramatically reduced with widespread usage of broad spectrum antibiotics [7, 8]. In 1900, Henri Luc described it as a sub-periosteal temporal abscess of otitic origin without intraosseous suppuration and suggested the possible pathway of microorganism spread from middle ear submucosa by anatomical pathways especially via the superior meatus, incisura Rivinus and along the branches of deep auricular artery [7]. Later this theory was supported by Le Marc’ Hadour and Chauveau in 1910 and they proposed three stages of periosteal involvement in the middle ear infection namely juxtatympanic stage, progression to entire circumference of canal skin and finally spread to sub-periosteum of temporal bone [7]. Clinically, it can be located anterior, superior or posterior to the auricle [7].
The role of HRCT in diagnosing middle ear pathology has been well established. This is crucial in assessing the location, extent of disease, identifying anatomical variations and for appropriate operative planning as evident by our case. In the absence of CC, Luc's abscess can be easily treated by limited surgical procedures either by pus drainage through an incision in the superior part of the external auditory meatus or through retroauricular incision combined with myringotomy and grommet insertion [7, 8]. In this case, patient underwent Luc's abscess drainage via retroauricular approach followed by a modified radical mastoidectomy to remove all disease and to prevent future recurrence.



