-
PDF
- Split View
-
Views
-
Cite
Cite
Sanjay Kumar, Sonia Hasija, Rama Goyal, Sant Prakash Kataria, Rajeev Sen, Raman Wadhera, Ectopic parapharyngeal meningioma: diagnosis of a rare entity on FNAC, Journal of Surgical Case Reports, Volume 2012, Issue 12, December 2012, rjs024, https://doi.org/10.1093/jscr/rjs024
Close - Share Icon Share
Abstract
Meningioma is a tumour most commonly located intracranially that may rarely extend extracranially. Ectopic meningioma presenting as parapharyngeal mass is a rare entity. We report a case of an 18-year-old female who presented with a complaint of swelling below the right angle of mandible associated with difficulty in swallowing for the last 3 months. The swelling measured 1.5 × 1 cm and was firm, fixed, non-pulsatile, non-transilluminant and non-tender. Computer tomography revealed a heterogenous enhancing mass with foci of calcification in parapharyngeal space without any intracranial component. Intraoral fine needle aspiration cytology was performed. A cytological diagnosis of spindle cell lesion of neural origin with the closest possibility of meningioma was rendered. Excision biopsy confirmed the diagnosis of ectopic parapharyngeal meningioma. It is important for clinicians and pathologists to be aware of this entity at the unusual site.
INTRODUCTION
Meningiomas are the benign tumour derived from arachnoid cells. Most commonly they are located intracranially, but they may be found extracranially at various sites. It is rare for meningioma to extend out of central nervous system to present as cervical and parapharyngeal mass. Ectopic meningiomas are very rare with an overall incidence of 1–2% [1]. The various sites for ectopic meningioma include orbit, middle ear, soft tissues, skin, lung, mediastinum and upper airway, including nasal cavity, paranasal sinuses and nasopharynx [2]. Primary extracranial meningiomas of the head and neck have also shown to have a relationship with neurofibromatosis, particularly type 2 NF characterized by bilateral acoustic schwannomas and lack of skin findings and having a defect on chromosome 22q with an autosomal-dominant inheritance pattern [3]. These tumours may pose diagnostic difficulties for the clinicians and cytologists because of their presentation at unusual sites. The cytological diagnosis depends on the anatomic site of presentation and the entities commonly found at these sites. The diagnosis and management of these tumours are particularly important because of their infrequent occurrence, unpredictable clinical behaviour and association with specific genetic defects. The literature is generally limited to few case reports of parapharangeal meningiomas diagnosed on aspiration cytology with a few reviews of the literature.
A CASE REPORT
An 18-year-old female presented with a complaint of swelling below the angle of mandible on the right side which was associated with difficulty in swallowing since the last 3 months. Local examination revealed a swelling measuring 1.5 × 1 cm which was firm, fixed, non-pulsatile, non-transilluminant and non-tender. Oral cavity examination revealed a swelling of ∼1.5 cm diameter seen on the right side of the oropharynx. Computer tomography (CT) revealed that swelling is due to a heterogenous enhancing mass in parapharyngeal space with foci of calcification. The mass was not having any intracranial extension. The patient was subjected to fine needle aspiration cytology (FNAC) and the aspiration from the swelling yielded very low cellularity. A repeat FNAC with an intraoral approach was performed. Smears revealed loose cohesive clusters of cells in syncytial fragments along with concentric whorling pattern at places (Fig. 1). These cells were oval-to-spindle shaped with elongated nuclei having bland nuclear chromatin. At places, these cells had palisaded appearance with fibrillary pink substance. Singly scattered cells and myxoid substance were also observed in the haemorrhagic background. Occasional psamomma bodies were also discerned at places in the smears (Fig. 2). A cytological diagnosis of spindle cell lesion of neural origin with the closest resemblance of ectopic meningioma was rendered. The tumour was excised and subjected to histopathological examination. Microscopically, tumour was composed of oval-to-spindle cells with indistinct outline and eosinophilic cytoplasm. The nuclei were round to oval with homogenous chromatin. No mitosis was observed. In some areas, cells were arranged in whorling pattern. Numerous psamomma bodies were also noted (Fig. 3). The cytological diagnosis of extracranial meningioma was confirmed on histopathology. The patient is on regular follow-up without any complication.
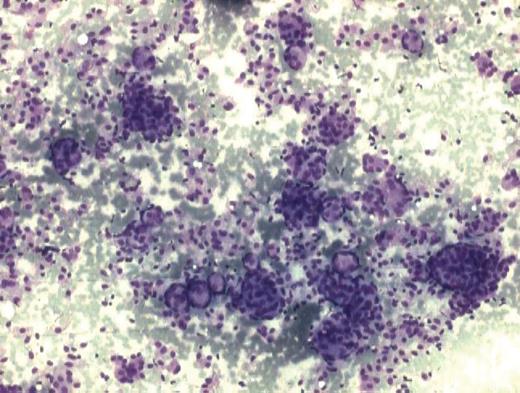
Cytology smear showing cells arranged in loose cohesive clusters with whorling pattern at places. (MGG stain ×100).
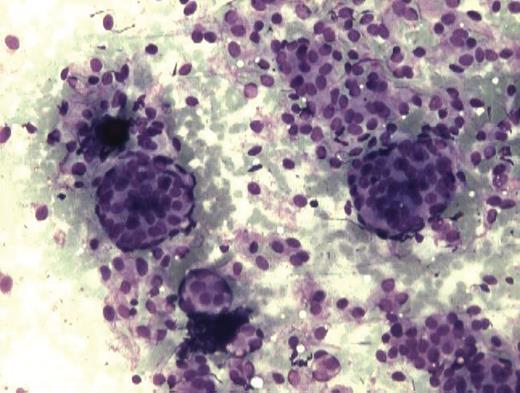
Smear showing occasional psamomma body in between cluster of cells. (MGG ×200).
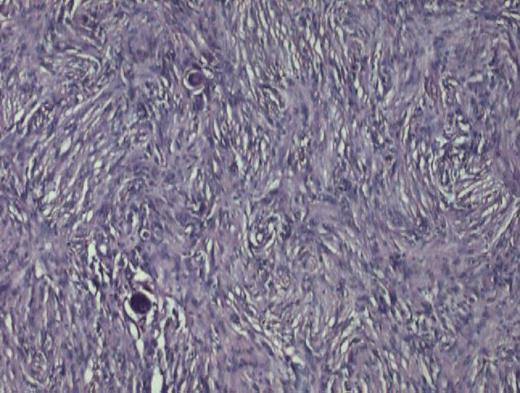
Photomicrograph showing psamomma bodies present in sheets of cells with meningothelial pattern. (Haematoxylin & Eosin stain ×200).
DISCUSSION
Meningiomas are relatively common benign neoplasm of the central nervous system comprising 15% of primary intracranial tumours and 12% of primary intraspinal tumours [4]. Females are affected twice when compared with males, because these tumours harbour hormone receptors. Genetic predisposition and high-dose radiation exposure remain the main risk factors of meningiomas [5]. However, extracranial and extraspinal meningiomas, termed as ectopic menigiomas, are extremely rare. They have been reported at various sites other than the head and neck region. They arise from meningothelial cells of arachnoid villi. However, they can also arise from fibroblast, Schwann cells or combination of these cells. These multipotent mesenchymal cells may proliferate at the ectopic sites to form meningioma. They are divided into four categories depending on their location. Ectopic meningiomas can present extracranially due to direct extension from cranial cavity. In these cases, they erode skull bone and present extracranially. Secondly, these tumours can arise from arachnoid cells and rests of cranial nerve sheaths. Most common location of these tumours is orbit and sheath of optic nerve. In the third category, they have no connection with central nervous system or cranial nerves but can arise from embryonic rests of arachnoid cells or multipotent mesenchymal cells. They can present anywhere in the body. The last category involves extracranial metastasis from primary intracranial tumours. Ectopic menigiomas are not easily aspirated due to their cohesive nature and pose a diagnostic challenge to the cytopathologist. They are cohesive tumours which are not aspirated easily unless they erode skull [6]. Meningiomas not related to central nervous system are difficult to explain especially when they are diagnosed on aspiration cytology [7]. The diagnosis of ectopic meningioma at this location is difficult as other tumours like paraganglioma, schwanomma and pleomorphic adenoma can mimic the cytologic findings and hence are preferably considered [1]. Biphasic population of cells, monomorphic round-to-oval and spindle cells arranged in syncytial and whorled pattern along with the presence of psamomma bodies have been described as a diagnostic feature of meningioma on cytology [8]. The above differentials need to be ruled out before diagnosing ectopic meningioma at these sites. The primary diagnosis of extracranial meningioma is difficult even on advanced radioimaging techniques like CT and MRI [9]. The diagnosis should always be confirmed on histopathology for further management. Four microscopic patterns have been described on histopatholgy: syncytial, transitional or psammomatous, fibrous and angioblastic. Extracranial meningiomas are commonly seen to exhibit syncytial or transitional pattern. Immunohistochemical (IHC) analysis aids in diagnostic accuracy as meningiomas show positive reactivity with epithelial membrane antigen and vimentin. IHC analyses of primary ectopic meningioma are similar to their intracranial counterparts [10].
While screening aspirates from head and neck lesions, possibility of meningioma should be considered in the differential diagnosis of parapharyngeal tumours. Cytological smear examination findings of tumour supported by radioimaging can be very helpful in preoperative diagnosis of meningioma presenting at an unusual site as was in our case. The treatment of choice for extracranial meningiomas is surgical excision. The completeness of surgical removal is the single most important prognostic factor [9]. The prognosis is good after complete resection without any recurrence. The low recurrence rate indicates the non-aggressive behavior of this lesion. Radiation may be effective in poor surgical patients and recurrent tumors [3]. It is important for the clinicians and the pathologists to be aware of the presentation of this tumour at unusual sites for an early diagnosis and timely management.



