-
PDF
- Split View
-
Views
-
Cite
Cite
Raden Andri Primadhi, Yoyos Dias Ismiarto, Fathurachman Fathurachman, Modified partial talectomy followed by tibiotalocalcaneal fusion for neglected clubfoot: a case series and literature review, Journal of Surgical Case Reports, Volume 2025, Issue 5, May 2025, rjaf342, https://doi.org/10.1093/jscr/rjaf342
Close - Share Icon Share
Abstract
Clubfoot management is complicated, especially in severe cases. Various treatment methods have been introduced, and there is no consensus on the best surgical approach or the best fixation hardware. These case series aim to display the viability of this surgical procedure, despite the short-term follow-up. Three patients with neglected clubfoot were presented. All patients underwent one-stage deformity correction using partial talectomy followed by tibiotalocalcaneal arthrodesis using a lateral plate. Two patients recovered uneventfully, and one patient needed another surgery because of fixation failure due to a lack of reinforcing fixation. Partial talectomy and tibiotalocalcaneal fusion is a viable option for the treatment of neglected clubfoot considering its various advantages, albeit some possible pitfalls that were also described. This study provided a basis for further studies involving a larger sample of patients and a longer follow-up period.
Introduction
Clubfoot is a common musculoskeletal congenital abnormality that leads to locomotor disability and worsens substantially when left untreated. Over time, correctable deformities become fixed and more difficult to manage, resulting in the need for extensive open surgery consisting of reduction, reconstruction, and internal fixation [1].
The goal of treatment is to create a stable, painless, plantigrade, and functional foot. Various surgical options have been introduced (Table 1), including soft tissue release, corrective osteotomies, gradual correction with the Ilizarov method, arthrodesis, and even amputation [2–4]. Ankle arthrodesis or tibiotalocalcaneal arthrodesis was proven to be efficacious in maintaining the joint position after correction and preventing recurrence [3]. Nevertheless, ankle arthrodesis is an option for late-presenting cases of neglected clubfoot in which plantigrade could not be maintained due to irreversible weak ankle dorsiflexor muscles. Gradual correction using a multiplanar ring fixator is beneficial because of its minimally invasive features, safety, and reproducibility in the context of poor skin condition [3, 5]. However, this technique is still considered complicated, and patient compliance is also essential [6].
| Methods . | Advantages . | Disadvantages . |
|---|---|---|
| Correction | ||
| Gradual correction | - Minimum soft tissue stripping - Less risk of neurovascular injury - Facilitating multiplanar correction | - Patient inconvenience - Compliance is compulsory - Risk of pin tract infection |
| One-stage correction with total talectomy | - Patient comfortability - Earlier rehabilitation program | - Presenting neurovascular injury risk from acute correction - Resulting joint incongruence |
| One-stage correction with Lambrinudi procedure | - Patient comfortability - Earlier rehabilitation program | - Risk of talar vascularity disturbance |
| One-stage correction with partial talectomy | - Patient comfortability - Earlier rehabilitation program - Better in preserving talar vascularity | - Need additional temporary fixation for protection |
| Fixation | ||
| Multiple screwing | - Minimum soft tissue dissection | - Less stability - Not suitable in porotic bone |
| Plating | - Good stability | - Larger incision is needed - Nonadaptive to particular joint position |
| Nailing | - Good stability with longer lever arm - Ability to fix the joint in various position | - Not widely available - Technically demanding |
| Ring external fixator | - Facilitating gradual correction and joint compression | - Patient inconvenience - Compliance is compulsory - Risk of pin tract infection |
| Methods . | Advantages . | Disadvantages . |
|---|---|---|
| Correction | ||
| Gradual correction | - Minimum soft tissue stripping - Less risk of neurovascular injury - Facilitating multiplanar correction | - Patient inconvenience - Compliance is compulsory - Risk of pin tract infection |
| One-stage correction with total talectomy | - Patient comfortability - Earlier rehabilitation program | - Presenting neurovascular injury risk from acute correction - Resulting joint incongruence |
| One-stage correction with Lambrinudi procedure | - Patient comfortability - Earlier rehabilitation program | - Risk of talar vascularity disturbance |
| One-stage correction with partial talectomy | - Patient comfortability - Earlier rehabilitation program - Better in preserving talar vascularity | - Need additional temporary fixation for protection |
| Fixation | ||
| Multiple screwing | - Minimum soft tissue dissection | - Less stability - Not suitable in porotic bone |
| Plating | - Good stability | - Larger incision is needed - Nonadaptive to particular joint position |
| Nailing | - Good stability with longer lever arm - Ability to fix the joint in various position | - Not widely available - Technically demanding |
| Ring external fixator | - Facilitating gradual correction and joint compression | - Patient inconvenience - Compliance is compulsory - Risk of pin tract infection |
| Methods . | Advantages . | Disadvantages . |
|---|---|---|
| Correction | ||
| Gradual correction | - Minimum soft tissue stripping - Less risk of neurovascular injury - Facilitating multiplanar correction | - Patient inconvenience - Compliance is compulsory - Risk of pin tract infection |
| One-stage correction with total talectomy | - Patient comfortability - Earlier rehabilitation program | - Presenting neurovascular injury risk from acute correction - Resulting joint incongruence |
| One-stage correction with Lambrinudi procedure | - Patient comfortability - Earlier rehabilitation program | - Risk of talar vascularity disturbance |
| One-stage correction with partial talectomy | - Patient comfortability - Earlier rehabilitation program - Better in preserving talar vascularity | - Need additional temporary fixation for protection |
| Fixation | ||
| Multiple screwing | - Minimum soft tissue dissection | - Less stability - Not suitable in porotic bone |
| Plating | - Good stability | - Larger incision is needed - Nonadaptive to particular joint position |
| Nailing | - Good stability with longer lever arm - Ability to fix the joint in various position | - Not widely available - Technically demanding |
| Ring external fixator | - Facilitating gradual correction and joint compression | - Patient inconvenience - Compliance is compulsory - Risk of pin tract infection |
| Methods . | Advantages . | Disadvantages . |
|---|---|---|
| Correction | ||
| Gradual correction | - Minimum soft tissue stripping - Less risk of neurovascular injury - Facilitating multiplanar correction | - Patient inconvenience - Compliance is compulsory - Risk of pin tract infection |
| One-stage correction with total talectomy | - Patient comfortability - Earlier rehabilitation program | - Presenting neurovascular injury risk from acute correction - Resulting joint incongruence |
| One-stage correction with Lambrinudi procedure | - Patient comfortability - Earlier rehabilitation program | - Risk of talar vascularity disturbance |
| One-stage correction with partial talectomy | - Patient comfortability - Earlier rehabilitation program - Better in preserving talar vascularity | - Need additional temporary fixation for protection |
| Fixation | ||
| Multiple screwing | - Minimum soft tissue dissection | - Less stability - Not suitable in porotic bone |
| Plating | - Good stability | - Larger incision is needed - Nonadaptive to particular joint position |
| Nailing | - Good stability with longer lever arm - Ability to fix the joint in various position | - Not widely available - Technically demanding |
| Ring external fixator | - Facilitating gradual correction and joint compression | - Patient inconvenience - Compliance is compulsory - Risk of pin tract infection |
Single-stage correction is a viable option not only for mild deformities but also for more severe deformities [2]. However, single-stage correction is difficult due to reduction and fixation. A long-standing deformity makes reduction difficult not only due to the presence of bony or soft tissue obstacles but also because of the risk of neurovascular and skin damage in acute correction. Moreover, some salvage procedures are needed to facilitate reduction.
Talectomy is a useful salvage procedure to correct a very rigid foot and ankle, particularly when gradual correction is not feasible [7]. Talectomy without arthrodesis will result in sufficient laxity of the soft tissue contracture to permit correction of the associated deformities [7]. Talectomy, however, produces an incongruous joint, and full correction is often still difficult to obtain [8]. Other disadvantages included inadequate bony support in the medial column of the foot and improper positioning of the calcaneus in the ankle mortise [9]. Lambrinudi triple arthrodesis is performed following the removal of the bone wedge located at the plantar-distal surface of the talus to correct the refractory equinus but also presented the risk of obliteration of artery in the tarsal sinus [10, 11].
Taking various surgical options into account, we can arrange the management strategy based on (i) gradual or acute correction, (ii) correction maneuver, (iii) fixator choice, and (iv) postoperative protocol. This case series reported the efficacy of the partial talectomy to facilitate the reduction, followed by tibiotalocalcaneal arthrodesis, which might be the suitable technique for certain patients’ characteristics. Here are also described the pitfalls of this method particularly from surgical technique perspectives.
Case series
Three complex cases of late-presenting neglected congenital clubfoot deformity in adults who had never sought appropriate orthopedic management before were described in this case series. All three patients were in early adulthood, and their ages ranged between 19 and 26 years. They were still able to walk with weight bearing on their inverted foot and ankle. Patients’ complaints at presentation consisted of poor cosmetic appearance, pain, and gait complications. The reasons behind the neglect of this medical condition included lack of access to appropriate health services and the patients’ families’ lack of education regarding the importance of clubfoot treatment. The main indications for choosing single-stage correction was the likelihood of these patients to be noncompliant for gradual correction.
This study was registered and approved by the Institutional Review Board of Hasan Sadikin Hospital No. LB.02.01/X.6.5/248/2022 before its implementation.
Case 1
A generally healthy 26-year-old man presented to our clinic complaining of a long-standing deformity of his foot and ankle (Fig. 1a–c). The patient reported that treatment of childhood clubfoot was not acknowledged within his family construct. At the presentation, his main complaint was poor cosmetic appearance, although pain and gait difficulty were present. We decided to undergo single-stage correction with partial talectomy followed by tibiotalocalcaneal arthrodesis using a lateral plate (Agofix, Agomed Medizin-Technik GmbH, Germany). The distal tibia articular surface preparation was done using lateral transfibular approach prior to plate placement.
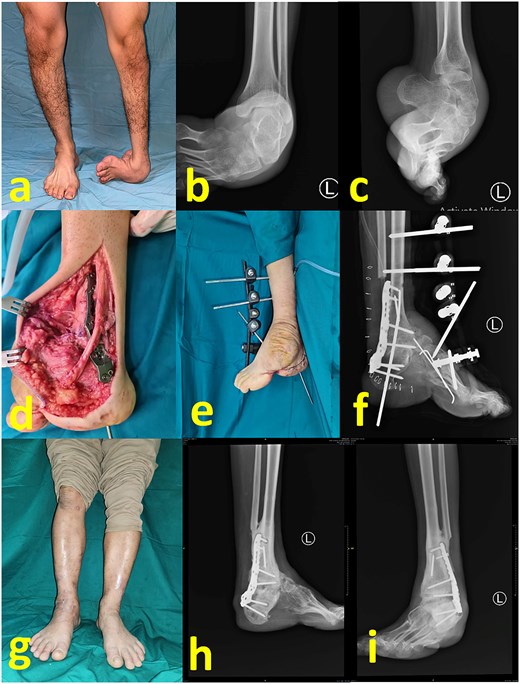
(a) Preoperative clinical images; (b) and (c) preoperative radiograph; (d) intraoperative image after partial talectomy followed by fixation with plate and screw; (e) immediate postoperative image depicting additional fixation with Schanz screw and external fixator; (f) immediate postoperative radiograph; (g) latest clinical images after 1 year postoperative; (h) and (i) latest radiograph after 1 year postoperative.
The patient was placed in the lateral decubitus position under regional anesthesia. The distal fibula was removed via the lateral transfibular approach. The plantar flexor tendon including the Achilles tendon was initially lengthened, but residual equinus remained due to bony obstruction as well as massive soft tissue contracture. Subsequent axial partial talectomy at the talar dome was performed as much as necessary to facilitate reduction. A lateral tibiotalocalcaneal plate that was applied to firm the ankle (Fig. 1d) was reinforced by a uniplanar external fixator (Fig. 1e and f). First metatarsal dorsal closing wedge osteotomy was completed to address the cavus midfoot. The surgical wound was irrigated and closed in a standard fashion.
An external fixator was worn for 1 month postoperatively and no weight bearing was permitted. Partial weight bearing was permitted 1 month following external fixator removal. The patient was allowed to begin full weight-bearing 2 months postoperatively while undergoing rehabilitation therapy, including proprioceptive exercise. Latest follow-up at 1-year postoperative period showed a stable and plantigrade ankle, with radiological signs of healed arthrodesis (Fig. 1g–i).
Case 2
A 19-year-old woman presented with a crooked ankle and foot resulting from an untreated childhood clubfoot (Fig. 2a–c). The cause of this neglect was delayed diagnosis and treatment, as there was limited access to adequate healthcare facilities in her remote hometown.
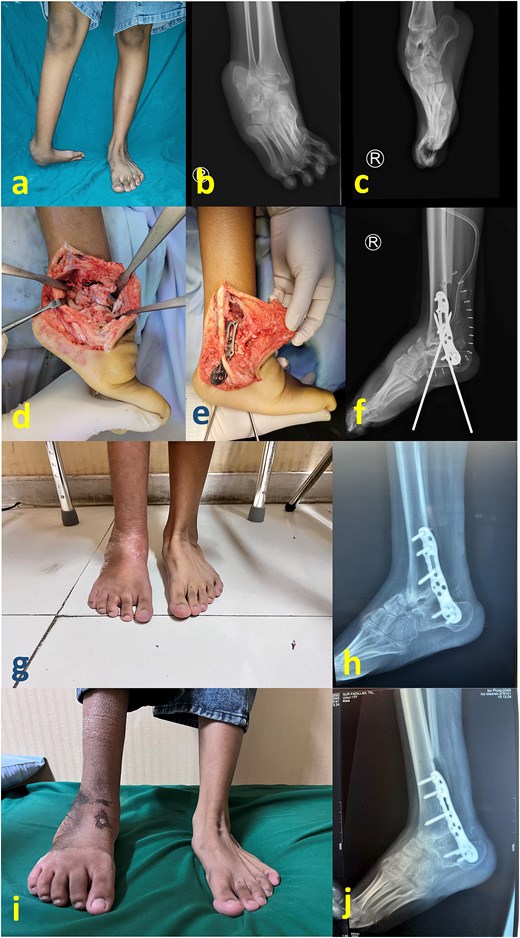
(a) Preoperative clinical images; (b) and (c) preoperative radiograph; (d) intraoperative image after partial talectomy followed by (e) fixation with plate and screw; (f) immediate postoperative image depicting additional fixation with Schanz screw; (g) clinical images at 2 months postoperative (h) 2 months postoperative radiograph; (i) latest clinical images after 1 year postoperative; (j) latest radiograph after 1 year postoperative showing healed arthrodesis.
Similar to the first case, surgery via the transfibular approach, posteromedial tissue release, reduction facilitated by partial talectomy and tibiotalocalcaneal plate fixation were performed (Fig. 2d and e). For this patient, the fixation was reinforced with two Schanz screws that were inserted from the calcaneal plantar side (Fig. 2f). Compared with the first case, this patient’s leg was thinner with less deforming forces such that an external fixator was deemed unnecessary. Another reason for not removing these Schanz screws was to prevent the patient from prematurely bearing weight on the affected foot, as postoperative follow-up monitoring would be technically hindered. At 2 months postoperation, the Schanz screws were removed. The patient was allowed to gradually bear weight, transitioning from partial to full weight-bearing (Fig. 2g and h). Full healed arthrodesis with stable plantigrade ankle was achieved at 1 year postoperative follow-up (Fig. 2i and j).
Case 3
A 22-year-old man presented with neglected clubfoot without a prior history of treatment (Fig. 3a–c). The surgical steps were similar to those in Cases 1 and 2 (Fig. 3d and e), except that the fixation was reinforced with merely a posterior cast splint. Postoperative complications occurred, including loss of fixation and wound breakdown (Fig. 3f). A subsequent operation was performed to address this problem, including hardware removal, debridement, and fixation using a ring external fixator (Fig. 3g and h). The external fixator was removed after 2 months (Fig. 3i), and weight bearing was allowed. The wound healed uneventfully, stable and platigrade ankle, as well as the healed arthrodesis can be observed at 1 year since the first surgery (Fig. 3j–l).
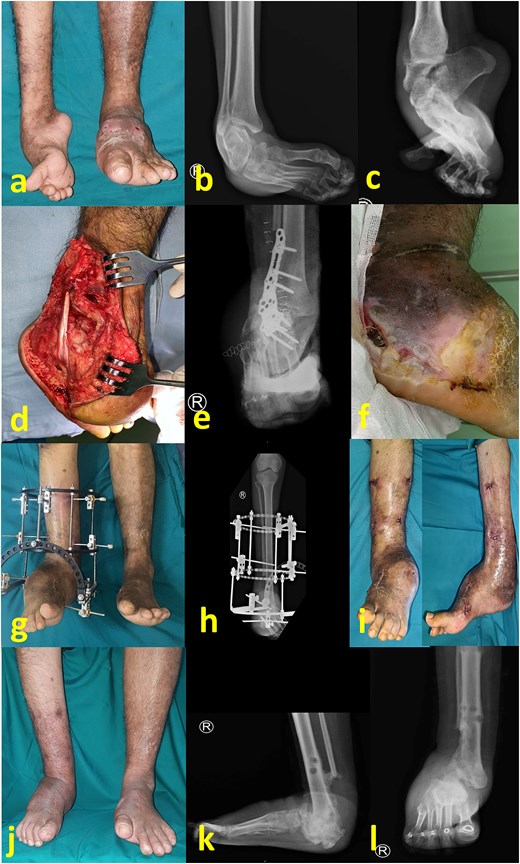
(a) Preoperative clinical image; (b) and (c) preoperative radiograph; (d) intraoperative image after partial talectomy; (e) immediate postoperative radiograph; (f) clinical image after 1 month, showing wound breakdown and loss of fixation; (g) clinical images after reoperation consisted of plate removal, debridement, reduction, and fixation with Ilizarov frame; (h) immediate radiograph after second surgery; (i) clinical image after frame removal at 2 months postoperative; (j) latest follow up image showing stable plantigrade ankle despite a persistent bulk at lateral foot; (k) and (l) latest radiograph at 1 year after first surgery, showing healed arthrodesis.
Discussion
In clubfoot cases, hindfoot deformity is considered the most difficult to treat [12]. In the late stage, the goal is to obtain a stable plantigrade foot with joint preservation if possible. If the hindfoot is flexible, osteotomy can realign the cavovarus foot without scarifying the joint. However, in rigid hindfoot cases, arthrodesis may be inevitable, as firm fixation is needed to prevent deformity recurrence [13]. Triple arthrodesis can effectively treat residual clubfoot deformities or cavus foot deformities due to joint adaptive changes and certain neurological conditions resulting in neuromuscular imbalances [14, 15]. Neglected clubfoot cases often show dorsiflexion weakness, regardless of its neuropathic or nonneuropathic origin. Clubfoot patients have less maximal ankle power, less maximum dorsi- and plantarflexor moment and less maximum dorsiflexion range of motion during walking [16]. Longstanding equinus position will compromise the dorsiflexor muscles and tendons, as an addition to the existing imbalance between thinner anterior and bulkier posterior muscle groups. Additionally, clubfoot is associated with neuromuscular dysfunction. Ankle dorsiflexion weakness can result from peroneal nerve dysfunction or more proximal spinal problems [17]. Ankle arthrodesis is a salvage procedure to restore the ankle plantigrade. Considering the concomitant need for talocalcaneal fixation in neglected clubfoot deformities, tibiotalocalcaneal fusion would be preferred.
Gradual correction using an external fixator raises some issues regarding patient comfort and compliance. When the patient or caregiver is incompliant, there is an increased risk of an underachieved desired correction, as well as pin tract infection. In addition, patients were often concerned about prolonged treatment time, inconvenience, activity limitation, and impact on social life in terms of cosmetic appearance. The use of external fixators is associated with depression, social isolation, and negativity [18, 19]. For these reasons, single-stage correction and internal fixation were chosen for particular patients. All patients here presented in early adulthood. Aside from inadequate diagnosis and lack of initial treatment due to living in a remote area, the relatively mild symptoms further delayed the medical visit. Surprisingly, they were still able to walk independently on their severely inverted foot, only complaining of mild pain. The motivation for surgery at present is the desire for a better cosmetic appearance, predominantly in adulthood, which is related to their social life and need for more mobility.
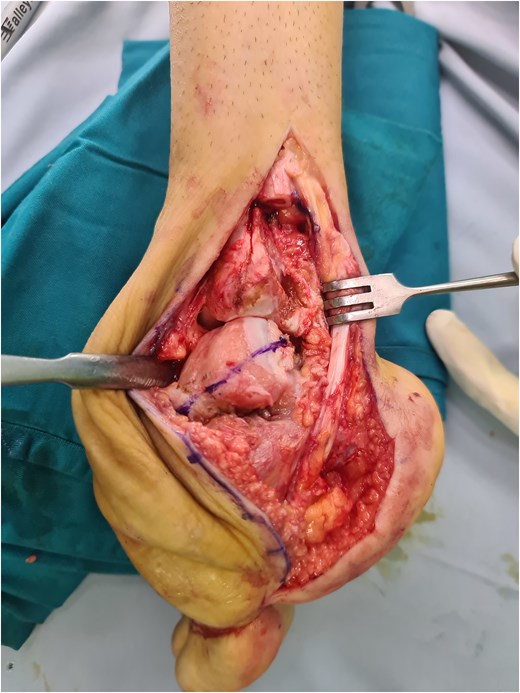
The partial talectomy method used in this case series was performed by removing a portion of the talar dome in axial plane using an oscillating saw to correct the hindfoot equinovarus deformity, mainly the equinus (Fig. 4). The bone cuts were done as much as necessary until the desired reduction was achieved. The lateral transfibular approach was selected due to its association with good exposure for deformity correction in the sagittal plane and its sufficient proximity to the articular surface. As mentioned before, bone cutting in this area will preserve the vascularization in the inferior talus or sinus tarsi, in contrast to the Lambrinudi procedure [11]. Compared with total talectomy, which results in an incongruous joint, partial talectomy is still able to facilitate proper contact between the distal tibia and cut talus. Various internal fixation methods are available to protect correction and to prevent recurrence. Generally, tibiotalocalcaneal fusion can be performed using multiple screws, plates and screws, or intramedullary nails. However, multiple screw placement would not be preferred due to poor bone stock. Gursu et al. reported the use of intramedullary nail fixation after talectomy in the management of severe rigid equinovarus deformity in adults. Intramedullary nails have a biomechanical superiority and ability to reduce incongruity between surfaces with sequential reaming [20]. Nevertheless, intramedullary nails are still not widely available worldwide, especially in developing countries, in which many similar neglected clubfoot cases can be found. Lateral plating is viable, especially when a lateral transfibular approach is used. Other than the anatomical tibiotalocalcaneal plate that is utilized in this study, various plates, such as reversed proximal humeral plates, can be applied as long as they enable sufficient screw placement [21].
An unfortunate case was presented in Case 3, in which fixation failure and wound breakdown occurred. This morbidity occurred because of inadequate protection after surgery, as the reinforcing external fixator or Schanz screws were not applied, in addition to the patient’s incompliance. Nonetheless, the results still favored the partial talectomy methods despite the fixation change.
Considering the indications, this technique is generally suitable for patients who are not compliant for gradual correction due to low level of education or socioeconomic problems prompting difficulty to have a regular hospital visit or multiple surgeries. Contraindications for this technique is predominantly the presence of other deformity centered in other location, such as distal tibia-fibula or calcaneus. External fixators or Schanz pin were applied postoperatively to protect the correction during the healing phase and to prevent recurrence, as the muscular imbalance occurred due to a long-standing deformity.
As a case series, this study has several main limitations. First, the small number of patients is inadequate to validate the efficacy of this method. Second, the short-term follow-up was also insufficient to evaluate the results. However, this study was conducted to report the technical viability of this method as a basis for future cohort studies. The follow-up time of approximately 2 months was selected to observe the short-term effect for the patients, particularly the ability to bear weight and correction results.
This case series showed that partial talectomy followed by tibiotalocalcaneal arthrodesis using lateral plating is a viable treatment option for neglected clubfoot in adults, particularly in terms of one-stage vs gradual correction, surgical approach, and implant choice. This technique can be applied to the patients that are not suitable for gradual correction, while addressing some potential pitfalls.
Conflict of interest statement
None declared.
Funding
None declared.



