-
PDF
- Split View
-
Views
-
Cite
Cite
Muhammad Affan Baig, Sneha Sohail, Muhammad Burhan Baig, Rahmat Gul Omarzai, Abdur Rehman, Chylolymphatic mesenteric cyst in a young adult: a case report, Journal of Surgical Case Reports, Volume 2026, Issue 1, January 2026, rjaf1007, https://doi.org/10.1093/jscr/rjaf1007
Close - Share Icon Share
Abstract
Mesenteric cysts are rare, benign tumors more commonly found in children than adults, accounting for 1 in 250 000 hospital admissions. Chylolymphatic mesenteric cysts arise from ectopic lymphatic proliferation in the mesentery and usually present with non-specific symptoms such as abdominal pain, swelling, or intestinal obstruction. Their variable presentation often delays diagnosis, which is frequently confirmed during surgical exploration. We report the case of a 25-year-old female presenting with abdominal swelling, pain, and nausea. Examination revealed a soft, non-tender right hemi-abdominal mass. Contrast-enhanced computed tomography showed a well-defined cystic lesion adjacent to small bowel loops. Following pre-operative evaluation, an exploratory laparotomy with complete excision was performed. The cyst contained milky fluid, consistent with a chylolymphatic mesenteric cyst, and histopathology confirmed a benign lesion. The postoperative course was uneventful. This case highlights the diagnostic challenge of such cysts in adults and supports surgical excision as a safe and effective treatment option.
Introduction
Mesenteric cysts are rare, benign, cystic tumors of the gastrointestinal mesentery, with fewer than 1000 reported cases [1, 2]. They are more common in children than adults, with an incidence of 1:20 000 in infants and 1:250 000 in adults [3]. These cysts are considered malformations of the lymphatic system, with no definitive risk factors identified. They may arise anywhere along the gastrointestinal mesentery, from duodenum to rectum, and can occasionally extend into the retroperitoneum [4]. Chylolymphatic mesenteric cysts represent one of six types of mesenteric cysts, accounting for 7.3% of all abdominal cysts. They are benign, endothelial- or mesothelial-lined lesions resulting from lymphatic obstruction or proliferation of ectopic lymphatics [5, 6]. While pediatric cases are more frequently reported, adult cases remain scarce in literature [7].
We present the case of a 25-year-old female who underwent successful surgical excision of a chylolymphatic mesenteric cyst at our institution.
Case presentation
A 25-year-old married female, mother of one, presented to our institution with a 1-month history of central, slightly right-sided abdominal swelling. Initially painless, it was later associated with dull abdominal pain responsive to analgesics and nausea. The swelling remained unchanged in size. Past surgeries included a lower-segment cesarean section 6 months earlier and an appendectomy 6 years ago. She had normal menstrual cycles and no comorbidities.
Examination revealed a round, non-distended abdomen with a right-sided bulge near the umbilicus. The mass measured ~5 × 5 cm, soft, cystic, smooth, mobile transversely but restricted vertically, and non-tender. No cough impulse, pulsation, or skin changes were noted. Percussion was dull over the mass; the rest of the abdomen was normal.
Biochemical tests were normal. Ultrasound revealed a 56 × 52 mm right sub-hepatic cystic lesion, likely a mesenteric cyst. CT confirmed a 5.2 × 4.9 cm well-defined cyst with enhancing walls, abutting small bowel loops (Fig. 1).
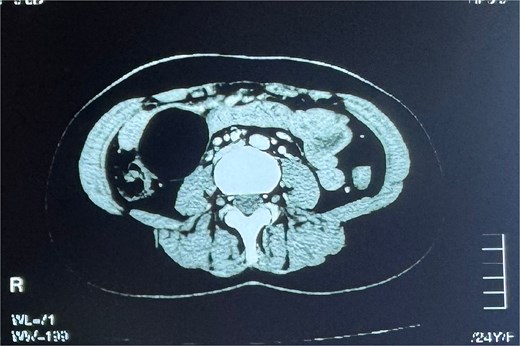
Contrast-enhanced CT scan of the abdomen showing a well-defined, rounded cystic lesion with enhancing walls in the right hemi-abdomen, abutting adjacent small bowel loops.
Following preoperative assessment, exploratory laparotomy revealed a 5 × 5 cm unilocular mesenteric cyst 30 cm distal to the duodenojejunal junction (Figs 2 and 3).

Intraoperative image showing a unilocular cyst within the mesentery, located ~30 cm distal to the duodenojejunal junction.
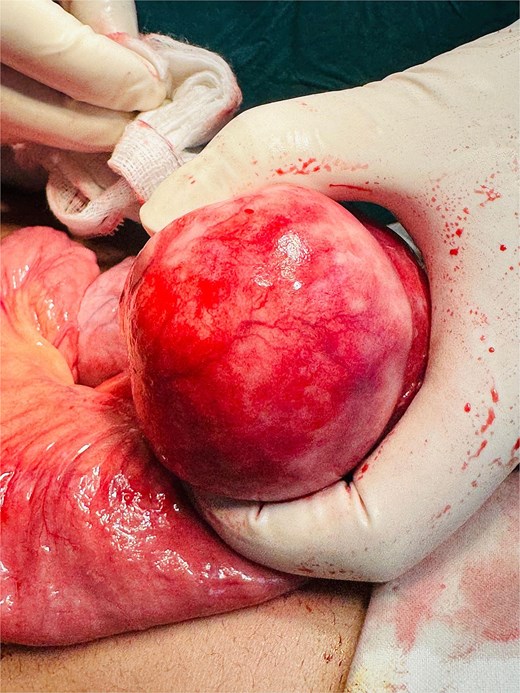
Intraoperative image showing a well-circumscribed, tense, unilocular mesenteric cyst with smooth external surface, arising from the small bowel mesentery ~30 cm distal to the duodenojejunal junction.
The cyst contained milky white fluid consistent with a chylolymphatic cyst and was completely excised (Figs 4 and 5).

Intraoperative image demonstrating surgical excision of the mesenteric cyst from the small bowel mesentery.

Intraoperative view of the operative field after complete excision of the mesenteric cyst, showing intact surrounding bowel loops without injury.
Histopathology confirmed a benign chylolymphatic mesenteric cyst, showing a focal bland mesothelial lining with papillary budding, chronic inflammatory infiltrate, underlying fibroblastic stroma, congested vessels, and absence of granulomas or malignancy (Fig. 6).
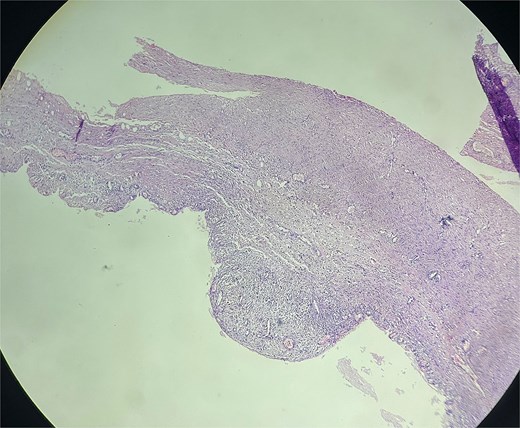
Histopathological section of the excised mesenteric cyst showing focal bland mesothelial lining with papillary budding, chronic inflammatory infiltrate, and underlying fibroblastic stroma, consistent with a chylolymphatic mesenteric cyst.
The postoperative course was uneventful. The patient was discharged on day two and remains asymptomatic on follow-up.
Discussion
Mesenteric cysts were first reported in 1507 by an Italian anatomist, Benevenni, who noted the cyst while performing an autopsy on an 8-year-old boy. In 1880, Tillaux was the first to successfully remove a cystic mass in the mesentery by surgical excision [8]. Chylolymphatic cysts are a more common variant of abdominal mesenteric cysts, but very few cases have been reported in the adult population as compared to the pediatric population [3]. Mesenteric cysts exhibit a slight male predominance, with a male-to-female ratio of 1.4:1 [9].
Mesenteric cysts present with variable symptoms, ranging from abdominal mass, pain, and distension in some patients to being discovered incidentally as a radiological finding in others. The patient may also present with severe symptoms in some cases, either due to infection, compression of surrounding structures, or rupture with hemorrhage [10, 11]. Rarely, a mesenteric cyst may mimic symptoms of acute pancreatitis or an acute abdomen. On examination, a tender and distended abdomen may be present, while in other cases, a palpable mass is the only finding noted [12]. Our study describes the case of a patient who presented with non-specific symptoms of a palpable abdominal mass, abdominal pain, and nausea, which are in line with the symptoms commonly reported in previous cases.
Common investigations involved in the management of a case of mesenteric cyst include transabdominal ultrasonography and a Computed Tomography scan, which are useful in visualizing the location of the benign cyst. An abdominal X-ray or magnetic resonance imaging (MRI) may also be performed for investigation [2, 12]. We performed a transabdominal ultrasonography, which showed a right sub-hepatic cystic lesion. A subsequent contrast-enhanced CT scan also helped visualize a well-defined, rounded cyst lesion with enhancing walls in the right hemi-abdomen, measuring 5.2 x 4.9 cm.
Histopathologically, chylolymphatic mesenteric cysts are usually lined by endothelium or mesothelium, supported by a fibrous or fibroblastic stroma, and may show varying degrees of chronic inflammation [5, 6]. In our case, the cyst demonstrated a focal bland mesothelial lining with papillary budding, fibroblastic stroma, and chronic inflammatory infiltrates, consistent with the benign features reported in previous series. Importantly, no evidence of granulomas, atypia, or malignancy was observed, further supporting the diagnosis of a benign chylolymphatic mesenteric cyst. These findings align with descriptions in the literature, which emphasize the benign nature of such cysts despite their variable clinical presentation [5, 6, 13].
The management of a mesenteric cyst is most often surgical, through an exploratory laparotomy and surgical enucleation of the cyst [9, 13]. In some cases, with a particularly large cyst involving adjacent structures, such as the small bowel, en-bloc surgical removal of the cyst as well as the involved bowel segment is performed [14]. Rarely, mesenteric cysts have also been managed with medication, followed later by elective surgery, as in a case presented by Leung et al., where a patient was managed with intravenous fluids, analgesics, antiemetics, and broad-spectrum antibiotics, followed by an elective laparotomy 9 months after initial presentation [15]. Our patient was managed by adequate pre-operative care and anesthesia assessment, after which an exploratory laparotomy was performed with surgical enucleation of the cyst.
Post-operative care can vary based on the treatment method employed. In case of need for bowel resection, or surgical repair of adjacent structure affected by the mesenteric cyst, the patient requires intensive post-operative care in the hospital, and frequent follow-up for months after discharge [14]. More often, enucleation of the cyst alone, without any surgery for adjacent structures, is performed, which requires less intensive post-operative care, and the patient can be discharged on the second or third post-op day. Follow-up in these cases is still required, but less frequently [13]. Our patient was in good general health following surgery and was discharged on the second post-op day, with advice for follow-up.
Conclusion
Mesenteric cysts are rare, benign tumors with diverse presentations that often delay diagnosis. Although typically asymptomatic, they can cause significant complications if left untreated, highlighting the importance of timely recognition and management. Complete surgical excision is the preferred treatment, offering both diagnostic confirmation and a low risk of recurrence. Our case demonstrates the diagnostic challenges of chylolymphatic mesenteric cysts in adults and emphasizes surgery as a safe and effective approach. Continued reporting of such cases will improve understanding and support standardized management strategies.
Conflict of interest statement
None declared.
Funding
The authors received no funding for this work.



