-
PDF
- Split View
-
Views
-
Cite
Cite
Toyin A Oyemolade, Augustine A Adeolu, Oluwafunmito L Oyewo, Vivian C Oko-Azu, Neuroblastoma of the thoracic spine in an adult: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 9, September 2024, rjae602, https://doi.org/10.1093/jscr/rjae602
Close - Share Icon Share
Abstract
Neuroblastoma (NB) in the adults is extremely rare. Even less encountered is NB involving the adult spine with only a few reported cases. Because of its rarity, there are as yet no well-established treatment guidelines for NB in the adults. Treatment strategies, therefore, are often extrapolated from paediatric data. We report a case of a 51-year-old man with NB involving the thoracic spine who had surgical excision with a good postoperative outcome in the short term.
Introduction
Neuroblastoma (NB) arises from primitive sympathetic ganglion cells with primary lesions therefore mainly occurring in the adrenal glands and the paraspinal sympathetic ganglia [1, 2]. It is considered primarily as a tumour of the paediatric age group, and represents the fourth most common malignant extracranial childhood tumour [3, 4]. NB in the adult population is extremely rare with only 1/10 million diagnosed per year compared to 1/100 000 in children [5]. Because of the rarity of adult NB, the staging, risk assessment, and management strategies are usually extrapolated from paediatric data [6]. Even less encountered is the NB involving the adult spine with only a few reported cases and, to the best of our knowledge, none from our country [3, 7]. We present a case of such managed by us with satisfactory early postoperative outcome.
Case report
A 51-year-old man presented with low back pain of 15 months duration and progressive lower limb weakness of 2 months. There was associated paraesthesia, as well as spasms in the lower limbs. He was no longer able to walk in the 13 days preceding the presentation. There was no history to suggest tuberculosis or metastatic lesions.
Neurological examination revealed spastic paraplegia. The muscle stretch reflexes were exaggerated with bilateral sustained ankle clonus. The sensory level was T12, and anal sphincteric tone was reduced. Other systemic examination findings were normal.
Thoracic spine MRI showed collapsed T11 vertebral body (Fig. 1), T1 isointense and T2 hyperintense extradural mass compressing the spinal cord and involving the posterior elements (Figs 1 and 2). There was no radiological evidence of metastatic lesions. He subsequently had T10–12 laminectomy, near total tumour excision, and spinal stabilization with rigid vertical strut and spinal process wire [8]. The tumour histomorphological and immunohistochemical features were consistent with NB.

Sagittal T1 (a) and T2 (b) weighted thoracic MRI images showing collapsed T11 vertebral body and tumour involvement of the T11 spinous process.
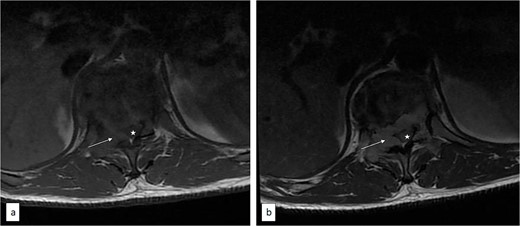
Axial T1 pre (a) and post (b) contrast thoracic spine MRI showing contrast-enhancing extradural tumour (arrow) compressing the spinal cord (asterisk).
He made significant postoperative neurological improvement, the power improved to 4-4+, and he was ambulating with Zimmer’s frame at the time of discharge from in-patient care. He was last seen at the follow-up clinic 16 months post-surgery. At this time, he was ambulating without support; power was grade 4+-5 in the lower limbs.
Discussion
NB is largely a disease of the paediatric age group, predominantly affecting children in the first decade of life [9, 10]. It arises from primitive sympathetic ganglion cells and has a broad spectrum of clinical behaviours, with some tumours regressing spontaneously or maturing, while some progress despite intensive multimodal treatment [11–13]. A number of staging systems for NB, including the surgicopathologic International Neuroblastoma Staging System (INSS), have been developed [14]. Many of these systems did not consistently incorporate prognostically significant factors, such as age, disease stage, the status of MYCN, DNA ploidy, chromosome 11q status, and histopathologic classification. These factors have been incorporated into the International Neuroblastoma Risk Group (INRG) Staging System (INRGSS) by the INRG Task Force [15]. Based on the INSS or the INRGSS, NB can be categorized into low, intermediate, and high-risk groups with potential for treatment stratification and prognostication.
NB in the adult patient is very rare [5]. Only a handful of cases of NB involving the adult spine have been reported [3, 7]. When present, NB involving the spine may present with motor, sensory, or autonomic symptoms, which may require urgent treatment to prevent irreversible neurological deficits [16]. Our patient had back pain, a sensory deficit, and significant motor weakness at presentation.
There are as yet no well-established management guidelines for NB in the adult population in general, and those involving the spine in particular, because of its rarity [3, 6, 7]. Therefore, treatment strategies are often extrapolated from paediatric data [6]. The available treatment options for spinal NB include surgery, chemotherapy, and radiotherapy [16]. Low-risk groups can be treated with surgery alone, while intermediate and high-risk groups require surgery with postoperative intensive induction chemotherapy [17]. Unresectable tumours may be treated with chemotherapy followed by radiotherapy [3]. Initially unresectable tumours may become amenable to surgery after neoadjuvant chemotherapy [7]. Our patient can be considered as low risk (localized tumour, near total excision, and no evidence of metastasis) based on INSS criteria and, as such, can be managed with surgery without chemotherapy or radiotherapy with a good prognosis in the short and medium term. He is now 16 months post-surgery; he is ambulating without support and has no evidence of tumour recurrence.
Conclusion
NB involving the adult spine is very rare and, as yet, has no established standard of care. The low-risk group can be managed with surgery alone, while the outcome in the intermediate and high-risk groups can be improved by surgery combined with chemotherapy and/or radiotherapy.
Acknowledgements
To the resident doctors and house officers in our unit who were involved in the care of the patient.
Conflict of interest statement
None declared.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.



