-
PDF
- Split View
-
Views
-
Cite
Cite
Anwar Sadat Seidu, Kouakou Emile Tano, Anita Esi Botchway, Jeffery Addo-Tham, Paa Ekow Hoyte-Williams, Neglected finger ring entrapment: a case series illustrating lessons for clinical practice, Journal of Surgical Case Reports, Volume 2024, Issue 9, September 2024, rjae598, https://doi.org/10.1093/jscr/rjae598
Close - Share Icon Share
Abstract
Finger ring entrapment could compromise the neurovascular status of the finger if not treated promptly. We aimed to report two cases of neglected finger ring entrapment following minor blunt trauma to the hand and illustrate some lessons for clinical practice. Both patients were right-hand dominant, presented 3–4 weeks after the onset of symptoms, and had circumferential ulceration of the affected fingers. The removal of both rings was performed using a wire cutter and bender. Neglected finger ring entrapment could result in multiple sequelae of the affected finger. Timely invention in finger ring entrapment is crucial to forestall neurovascular sequelae. We recommend immediate removal of all jewellery on fingers following any form of hand trauma as a primary preventive measure. We also recommend that clinicians who intend to use a ring-cutting method assess the material used to forge the ring to aid proper selection of a cutting device.
Introduction
A ring is a common ornament worn on the fingers and other parts of the body for varied reasons [1–3]. Finger ring entrapment is an infrequent presentation to the emergency department with no reported incidence [4–7]. It may be caused by tissue swelling following pregnancy, trauma, infection, allergic reaction, etc [4]. In Sub-Saharan Africa, there are few reports on the subject. To the best of our knowledge, our search did not reveal reported cases of neglected finger ring entrapment. If treatment is not given promptly, an entrapped ring may pose an imminent threat to the neurovascular structures and soft tissue of the involved finger [4, 5]. There are many studies illustrating different techniques for removing entrapped finger rings [6–11]. A systematic review by Kalkan et al (2013) classified the treatment options into two broad methods: noncutting techniques, and ring-cutting techniques [5]. We aimed to report two cases of neglected ring entrapment in a young male and female adult following minor blunt trauma to the hand that were managed in succession at a Teaching Hospital in Ghana and illustrate some lessons for clinical practice.
Case summary
Case 1
A 24-year-old right-hand dominant male presented 3 weeks after a ring entrapment on his right ring finger. He sustained a minor blunt domestic injury to his hand which resulted in pain and progressive swelling of the right ring finger. The pain and swelling increased after 24 hours and he noticed he could no longer remove the ring on his finger. He used several home strategies to remove the ring which were futile. He resorted to taking over-the-counter analgesics. After about a week, he noticed a gradual ulceration of the skin underneath the ring. Three weeks after the initial incident, he reported to the emergency department for removal of the ring. He reported late because of financial constraints. There was no history of psychiatry illness.
On examination, there was an entrapped ring on the right ring finger. There was a circumferential ulceration over the proximal phalanx. The ulcer had granulated and buried the ring on the dorsal, medial, and lateral aspects of the finger (Fig. 1A and B). The finger was flexed at 900 at the proximal interphalangeal (PIP) joint with a reduced range of motion. Capillary refill and sensation at the tip of the finger were intact. The patient consented to the removal of the ring. The hand was prepped and draped under a digit block with 10 ml of 1% lidocaine. An attempt was made to use a manual ring cutter, but it broke down because the metal used to forge the ring was from harder metal. A wire cutter was then used to cut the ring and two wire benders were used to aid its removal from the finger. The extensor digitorum tendon was intact. The wound was debrided, irrigated copiously with saline, and dressed with vaseline gauze (Fig. 1C). The patient was given a follow-up plan for physiotherapy and an outpatient clinic but was lost to follow-up.
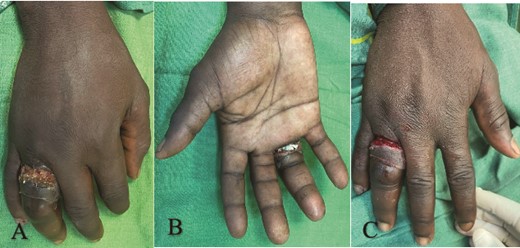
(A) Dorsal view showing circumferential ulcer with ring buried on the right ring finger, (B) ventral view showing entrapped ring, and (C) after ring removal and wound debridement.
Case 2
A 21-year-old right-hand dominant female presented to the outpatient clinic 4 weeks following an entrapped ring on her right index finger. She has no history of psychiatric illness. She sustained a minor blunt domestic injury to the right hand which resulted in pain and swelling of the index finger. A day after the injury, she noticed the ring was trapped and multiple attempts to remove it proved futile. She did not seek medical advice due to financial constraints but rather resorted to taking analgesics to control the pain with the hope that the swelling would resolve. She noticed a progressive ulceration of the skin over the proximal phalanx. On examination, there was a swollen right index finger with an entrapped ring. There was ulceration on the medial and lateral aspects of the finger. The skin on the dorsal aspect of the finger was healed and the ring was trapped beneath it (Fig. 2A and B). There was no discharge from the wound. The distal sensation and capillary refill were intact. The PIP joint was flexed at 1200 with a reduced range of movement. The PIP joint was stiff with limited extension. She was counselled for ring removal. Under a ring block with 10 ml of 1% lidocaine, the hand was prepped and draped. The skin on the dorsum of the finger was incised and dissected to expose the ring beneath it. It was noticed that the ring was made from a hard metal. A wire cutter was used to cut the ring and two wire benders were used to bend the ring to facilitate removal. The extensor digitorum and extensor indicis tendons were intact. Sensation and capillary refill were intact after the procedure. The wound was irrigated with saline, debrided and dressed with vaseline gauze (Fig. 2C). The patient was given a follow-up plan for physiotherapy and outpatient clinic but was lost to follow-up.
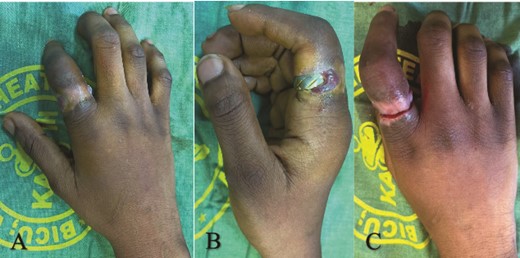
(A) Dorsal view showing right index finger with ring buried within granulation tissue, (B) lateral view showing circumferential ulceration, and (C) after ring removal.
Discussion
The two cases in this study were young adults, both right-hand dominant who presented 3–4 weeks after finger entrapment. Both patients had a prior history of minor blunt domestic trauma to their hands and tried multiple times to remove their rings at home without success. Both patients in this study were young which is consistent with literature in Sub-Saharan Africa [1]. A study in Nigeria by Echem et al (2019) reported the mean age of patients as 22.92 ± 9.33 years [1]. The duration of symptoms of the patients in this study however was unusual compared to the available literature. Most patients with ring entrapment present early to the emergency department when the pain and swelling commences. The mean duration of symptoms before presentation is reported to be 5.72 ± 4.57 days [1]. The presentation in this study was therefore late. It is safe to say presenting 3–4 weeks following finger ring entrapment with circumferential ulceration of the finger should be considered neglected. Our literature search did not reveal any reports of neglected finger ring entrapments; thus this may be the first of such cases to be reported. In neglected cases like these, it is crucial to evaluate the mental state of these patients. Both patients in this study were of sound mind and had no history of psychiatric illness. They presented late because of financial constraints.
In both cases, trauma was the underlying cause of the finger ring entrapments as seen in other literature. Other causes of finger ring entrapments include tissue swelling from pregnancy, allergic reactions, and infections [4, 5, 12]. The best preventative remedy in this study would have been the immediate removal of the rings following the hand trauma. Both patients attempted multiple home removal techniques several hours after the hand trauma. We posit that pressure ischemia and necrosis from the surrounding tissue swelling and ring constriction may have resulted in the ulceration of the skin of the proximal phalanx of the affected fingers. The multiple removal attempts at home may have also played a role because of the multiple minor injuries to the skin that may have resulted from this process. Thus, it is recommended that patients seek medical advice after a couple of failed home removal techniques of an entrapped finger ring.
Most patients with finger ring entrapment present early for management. Delayed presentation result in increasing pain and swelling which may result in neurovascular compromise [3, 13]. The neurovascular structures of the finger are thinly covered and are thus susceptible to compression from an entrapped or impacted ring. When entrapped or impacted, it may lead to ischemia and gangrene of the distal segment of the finger. It may also cause neuropraxia if the digital nerves are compromised resulting in impaired sensation of the finger [4, 5]. Other sequelae to finger ring entrapment include tendon injury, infection, and stiffness [4]. Both patients in this study did not suffer finger ischemia and gangrene even though their ring entrapments were prolonged. A plausible explanation could be that the pressure exerted by the entrapped ring on the sides of the finger where the digital arteries run was not high enough to compromise the blood supply to the fingers. Another explanation could be that the finger ulceration may have prevented any further build up of compartmental pressure required to compromise the blood supply to the finger.
Even though there are various treatment techniques with modifications thereon by authors in published literature [6–11], there is less scholarly attention given to finger ring entrapment by authors of emergency medicine or hand surgery textbooks. Kalkan et al (2013) provided a compressive treatment algorithm for ring removal techniques by reviewing the existing literature [5]. They classified the treatment into noncutting techniques and ring-cutting techniques. The noncutting techniques preserved the ring which may be of symbolic or emotional significance to the patient. This technique is subdivided into the winding, compression, caterpillar, twin thread, and glove techniques [5]. The ring-cutting techniques are used when there is imminent neurovascular compromise to the finger; there is ulceration of the skin, or the noncutting techniques fail [4, 5]. The common devices used for ring cutting include pliers, pincers, manual ring cutters, dental drills or saws, electric saws, Dremel motor saws, etc [4, 5, 12].
In patients who have finger ulceration as in this study, the ring-cutting techniques are the most suitable method for removal. The device used to cut the ring generally depends on availability and the type of material used to forge the ring [5, 12]. For softer materials like plastic, gold, copper, or silver, the manual ring cutter can be used [5]. Pliers and pincers can be used to cut rings containing tungsten carbide or ceramic [5]. For titanium or steel rings which are harder metals, it is recommended to use the electric saw, dental drill or saw, or Dremel motor saws [5]. In the first case, the ring material was not evaluated, so the manual ring cutter was used and was destroyed thereof. Subsequently, a wire cutter and bender were improvised to cut the ring. Because the cases were managed in succession about a month apart, there was a proper evaluation of the ring material in the second case to forestall using the wrong cutting device. Early physiotherapy to restore finger function is a crucial part of the management [14]. In this study, both patients were lost to follow and thus we are unable to report on the wound healing and functional outcomes of their fingers. Both patients had stiffness of the PIP joint prior to surgical intervention.
Conclusion
Neglected finger ring entrapment could result in multiple sequelae of the affected finger. Timely invention in finger ring entrapment is crucial to forestall neurovascular sequelae. We recommend immediate removal of all jewellry on fingers following hand trauma as a primary preventive measure. We also recommend the assessment of the material used to forge the ring to aid proper selection of the ring cutting device.
Author contributions
All authors conceived the study, A.S.S. drafted the manuscript, A.S.S., J.A.T., and A.E.B. wrote the case summaries and gathered the pictures. K.E.T. and P.E.H.W. supervised the study. All authors reviewed and approved the final manuscript.
Conflict of interest statement
None declared.
Funding
No funding received for the study.
Consent
Informed consent was obtained from both patients to publish this content.



