-
PDF
- Split View
-
Views
-
Cite
Cite
Leonardo Berto, Arthur Cardoso Paroneto, Gabriel Ferreira Santos Vasconcelos, Ewerton Borges de Souza Lima, Paulo Henrique Schmidt Lara, Paulo Santoro Belangero, Carlos Vicente Andreoli, Alberto de Castro Pochini, Benno Ejnisman, Surgical treatment of traumatic rupture of the teres major tendon in a professional gymnast: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 9, September 2024, rjae568, https://doi.org/10.1093/jscr/rjae568
Close - Share Icon Share
Abstract
Teres major injuries are rare and are generally treated conservatively, except in high-performance athletes. This report describes a case of traumatic rupture of the teres major at its myotendinous junction in a professional gymnast. The patient underwent surgical treatment 10 days after the injury. Six months post-surgery, the patient achieved complete recovery of the range of motion and strength, returning to the pre-injury performance level, guided by physiotherapy rehabilitation. This is the first documented case in the literature of surgical treatment of this injury in a professional gymnast. The main lesson from this case is that early surgical repair in elite athletes can result in excellent functional outcomes and allow return to sport at the pre-injury performance level.
Introduction
Avulsions or myotendinous injuries of the teres major are uncommon, typically occurring in high-level athletes after trauma [1, 2]. These injuries are challenging to diagnose and present unique physical examination findings, with most literature consisting of case reports and series [2–5]. They are most commonly seen in baseball athletes, with fewer reports in waterskiing, wakeboarding, tennis, climbing, and military activities [2]. Treatment is debated, with conservative physiotherapy often yielding good results, while surgical intervention is usually reserved for high-performance athletes and conducted in the acute or subacute phase [6, 7]. This case report documents the first surgical treatment of a teres major rupture in a high-level gymnast, detailing postoperative recovery and return to sport.
Case report
A 23-year-old left-handed male professional gymnast experienced sudden pain and loss of strength in his left shoulder during an extension movement on parallel bars, during training. Two days post-injury, he presented with deformity in the left dorsal region (Fig. 1), pain on palpation in the teres major and latissimus dorsi areas, and a full range of motion but reduced strength in extension and lateral rotation compared with the right shoulder. Neurological examination was normal. He denied any comorbidities or anabolic steroid use. Radiographs were unremarkable, but a T2-weighted magnetic resonance imaging (MRI), performed 1 week after the injury, showed a hyperintense signal at the myotendinous junction of the teres major (Fig. 2).

Clinical image of the patient’s back showing a muscle deformity on the left side, at the teres major/latissimus dorsi topography, indicated by the white arrow.
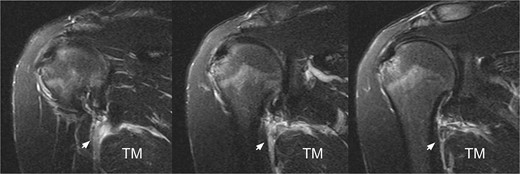
T2-weighted MRI revealing a hyperintense signal at the myotendinous junction of the teres major, indicated by the white arrow.
Treatment
Given the complete rupture on the MRI and the high functional demand of the patient, surgical treatment was indicated and performed 10 days post-injury. The patient was positioned in a right lateral decubitus position with the left upper limb in 90° abduction (Fig. 3). A single 8 cm incision was made at the posterior axillary fold (Fig. 4). After identifying the radial nerve, a complete tear of the teres major at the myotendinous junction was visualized (Fig. 5). The tendon was tied with FiberWire (Arthrex, Naples, FL, USA) (Fig. 6) and its mobility confirmed. The humeral insertion site was exposed, debrided, drilled with two parallel holes 3 cm apart, and fixed with two Pec Buttons. The sutures were tensioned to stabilize the tendons. The shoulder’s range of motion was evaluated, confirming adequate repair tension (Fig. 7), and the incision was sutured. Final intra-op radiographic image is shown in Fig. 8. Post-surgery, no neurovascular changes were noted.
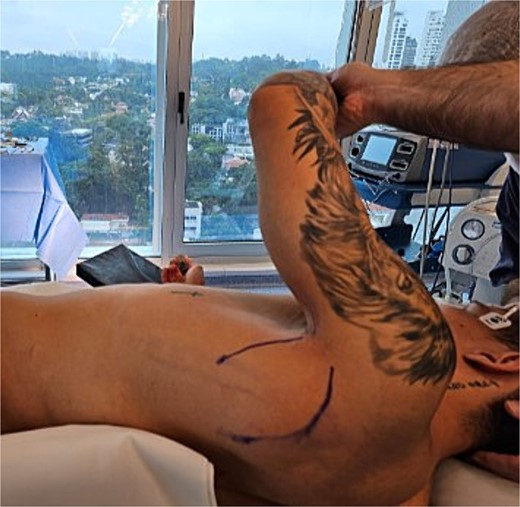
Patient positioned in a right lateral decubitus position with the left upper limb free over the body in 90° abduction.

A single incision was made at the level of the posterior axillary fold, ~8 cm in length.



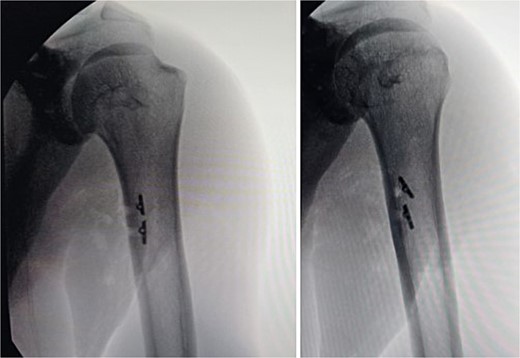
Post-surgery anteroposterior radiographies of the arm showing both Pec Buttons used for the teres major repair.
Outcome and follow-up
Post-surgery, the patient rested with a sling for 1 week. In the second week, he began passive range of motion exercises under physiotherapy supervision. By the fourth week, he removed the sling completely and started active-assisted exercises. Between the fifth and eighth weeks, he achieved a full range of motion. By the 13th week, he was performing isometric and isotonic exercises. Subsequently, he began weight training and gradually returned to basic sports movements. The patient resumed sporting activities, including international competitions, at his pre-injury performance level. Six months post-surgery, he reported high satisfaction with the results, noting consistent improvement in shoulder range of motion and strength, acknowledging the surgery and intensive rehabilitation as crucial for his continued professional gymnastics career without limitations.
Discussion
This report is the first documented case of surgical treatment of the teres major in a high-level gymnast. The first report of isolated teres major surgical treatment was in 2013 [2], following an injury during waterskiing in a 33-year-old male patient who experienced refractory pain and loss of strength with conservative treatment for 1 month before undergoing surgery. One year post-surgery, the patient had strength identical to the contralateral side.
Recently, Rademaker et al. [5] in 2023 reported a similar case of a judo athlete with avulsion of the teres major and latissimus dorsi confirmed by MRI. Due to the high level of physical activity, the patient underwent surgical treatment with a technique similar to that of this case, showing excellent postoperative evolution in terms of recovery of strength, pain, and range of motion.
In 2023, Roar Petersen et al. [6] reported a middle-aged female gymnast with combined teres major and latissimus dorsi injuries from an eccentric contraction on uneven bars. She felt a pop in her right shoulder, followed by swelling and reduced muscle function. An MRI confirmed the injury. She continued to exercise without guided physiotherapy, avoiding abrupt movements. After 6 months of non-surgical treatment with adapted exercises, she was pain-free and could perform physical activities without strength asymmetries, though she still experienced some stretching sensations.
Given their anatomical relationship, the surgical techniques for repairing the teres major and latissimus dorsi are similar. These can be performed using two transosseous tunnels or a single incision, as used in this report [8]. The single incision approach offers ease of tendon visualization, while the dual access method is beneficial for greater tendon retraction [5, 8–10].
In the past, injuries to the pectoralis major were often managed non-surgically. However, studies over the years have shown that surgical treatment can provide superior functional and strength outcomes compared with non-operative management, especially in athletes [11, 12]. Similarly, we believe that the treatment of teres major injuries will follow a comparable trajectory, with clinical practice evolving to favor early surgical repair for these injuries.
This case report is the first to document the surgical treatment of a teres major rupture in a gymnast, detailing the patient’s diagnosis, surgery, and rehabilitation. However, the study has limitations: absence of objective strength measurements and functional evaluations, short 6-month follow-up and its methodology which limits generalizability. Future research should include larger cohort studies to compare the long-term efficacy of surgical and conservative treatments for teres major injuries in elite athletes, incorporating objective muscle strength measurements, standardized functional evaluations, and extended follow-up periods to assess durability and late complications.
Conclusion
Early surgical repair of teres major injuries in high-level athletes is a viable therapeutic option with the potential for excellent functional outcomes and a return to sport at the pre-injury performance level.
Conflict of interest statement
The authors declare no conflicts of interest.
Funding
This study received no financial support from public, commercial, or non-profit sources.



